J Korean Neurosurg Soc.
2021 Jul;64(4):575-584. 10.3340/jkns.2021.0024.
C7 Fracture as a Complication of C7 Dome-Like Laminectomy : Impact on Clinical and Radiological Outcomes and Evaluation of the Risk Factors
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University Hospital, Seoul, Korea
- 2Department of Neurosurgery, Seoul National University College of Medicine, Seoul, Korea
- 3Department of Neurosurgery, Seoul National University Bundang Hospital, Seongnam, Korea
- 4Department of Brain and Cognitive Sciences, Seoul National University College of Natural Sciences, Seoul, Korea
- KMID: 2517690
- DOI: http://doi.org/10.3340/jkns.2021.0024
Abstract
Objective
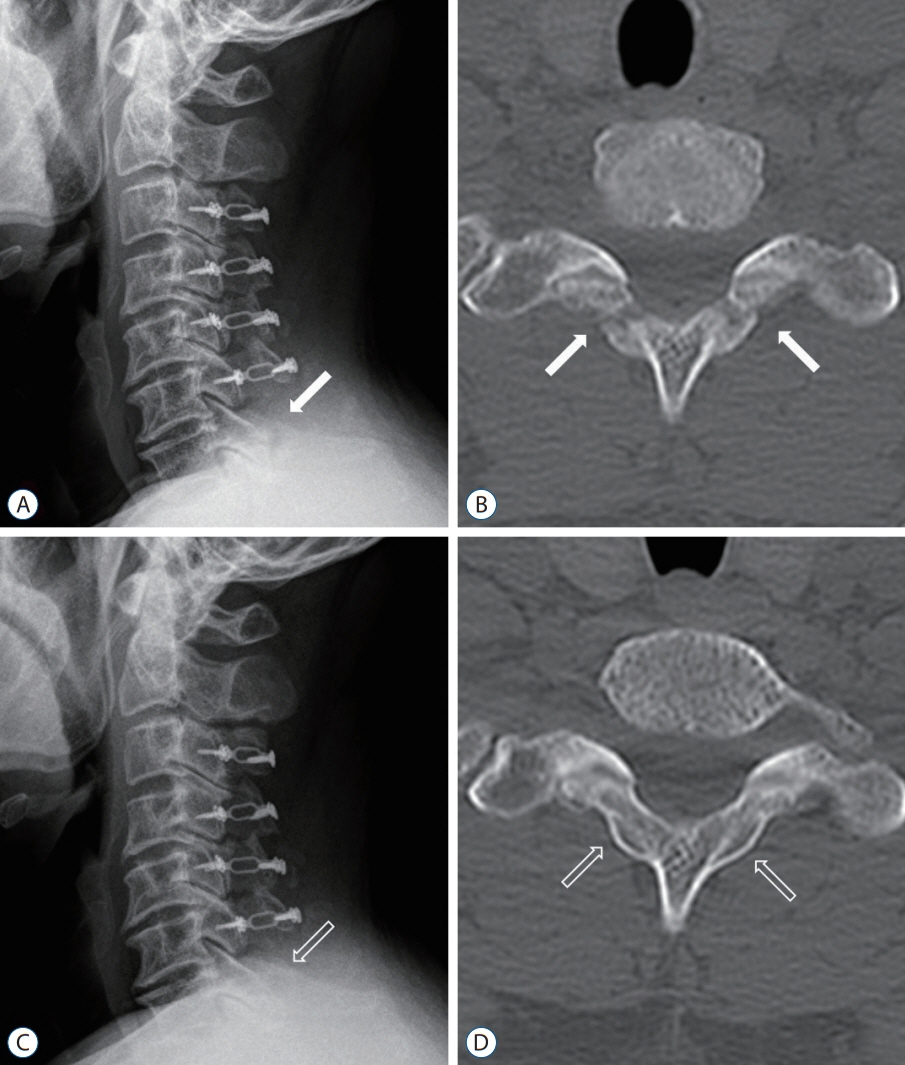
: Cervical expansive laminoplasty is an effective surgical method to address multilevel cervical spinal stenosis. During surgery, the spinous processes of C2 and C7 are usually preserved to keep the insertion points of the cervical musculature and nuchal ligament intact. In this regard, dome-like laminectomy (undercutting of C7 lamina) instead of laminoplasty is performed on C7 in selected cases. However, resection of the lamina can weaken the C7 lamina, and stress fractures may occur, but this complication has not been characterized in the literature. The objective of the present study was to investigate the incidence and risk factors for C7 laminar fracture after C7 dome-like laminectomy and its impact on clinical and radiological outcomes.
Methods
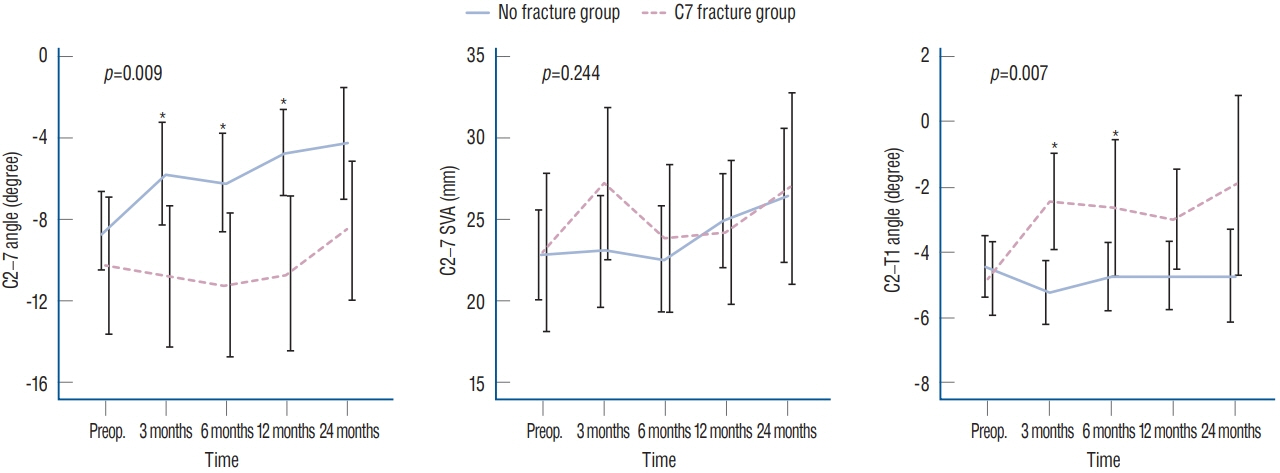
: Patients who underwent cervical open-door laminoplasty combined with C7 dome-like laminectomy (n=123) were classified according to the presence of C7 laminar fracture. Clinical parameters (neck/arm pain score and neck disability index) and radiologic parameters (C2–7 angle, C2–7 sagittal vertical axis, and C7–T1 angle) were compared between the groups preoperatively and at postoperatively at 3, 6, 12, and 24 months. Risk factors for complications were evaluated, and a formula estimating C7 fracture risk was suggested.
Results
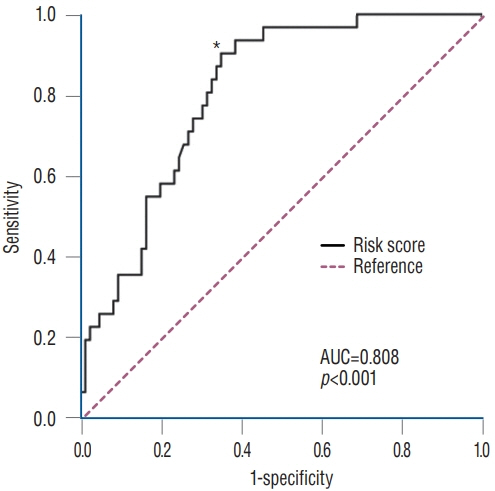
: C7 lamina fracture occurred in 32/123 (26%) patients and occurred at the bilateral isthmus in 29 patients and at the spinolaminar junction in three patients. All fractures appeared on X-ray within 3 months postoperatively, but patients did not present any neurological deterioration. The fracture spontaneously healed in 27/32 (84%) patients at 1 year and in 29/32 (91%) at 2 years. During follow-up, clinical outcomes were not significantly different between the groups. However, patients with C7 fractures showed a more lordotic C2–7 angle and kyphotic C7–T1 angle than patients without C7 fractures. C7 fracture was significantly associated with the extent of bone removal. By incorporating significant factors, the probability of C7 laminar fracture could be assessed with the formula 'Risk score = 1.08 × depth (%) + 1.03 × length (%, of the posterior height of C7 vertebral body)', and a cut-off value of 167.9% demonstrated a sensitivity of 90.3% and a specificity of 65.1% (area under the curve, 0.81).
Conclusion
: C7 laminar fracture can occur after C7 dome-like laminectomy when a substantial amount of lamina is resected. Although C7 fractures may not cause deleterious clinical outcomes, they can lead to an unharmonized cervical curvature. The chance of C7 fracture should be discussed in the shared decision-making process.
Figure
Reference
-
References
1. Ames CP, Smith JS, Eastlack R, Blaskiewicz DJ, Shaffrey CI, Schwab F, et al. Reliability assessment of a novel cervical spine deformity classification system. J Neurosurg Spine. 23:673–683. 2015.
Article2. Colantonio DF, Saxena SK, Vanier A, Rodkey D, Tintle S, Wagner SC. Cervical spine computed tomography hounsfield units accurately predict low bone mineral density of the femoral neck. Clin Spine Surg. 33:E58–E62. 2020.
Article3. Diebo BG, Challier V, Henry JK, Oren JH, Spiegel MA, Vira S, et al. Predicting cervical alignment required to maintain horizontal gaze based on global spinal alignment. Spine (Phila Pa 1976). 41:1795–1800. 2016.
Article4. Fujimura Y, Nishi Y. Atrophy of the nuchal muscle and change in cervical curvature after expansive open-door laminoplasty. Arch Orthop Trauma Surg. 115:203–205. 1996.
Article5. Hosono N, Sakaura H, Mukai Y, Fujii R, Yoshikawa H. C3-6 laminoplasty takes over C3-7 laminoplasty with significantly lower incidence of axial neck pain. Eur Spine J. 15:1375–1379. 2006.
Article6. Hyun SJ, Kim KJ, Jahng TA, Kim HJ. Clinical impact of T1 slope minus cervical lordosis after multilevel posterior cervical fusion surgery: a minimum 2-year follow up data. Spine (Phila Pa 1976). 42:1859–1864. 2017.
Article7. Ishikawa M, Matsumoto M, Chiba K, Toyama Y, Kobayashi K. Longterm impact of atlantoaxial arthrodesis on the pediatric cervical spine. J Orthop Sci. 14:274–278. 2009.
Article8. Jung JM, Chung CK, Kim CH, Yang SH. Clinical and radiological outcomes of C3-C6 laminoplasty with C7 dome-like laminectomy. Interdiscip Neurosurg. 15:47–52. 2019.
Article9. Kim CH, Chung CK, Choi Y, Kuo CC, Lee U, Yang SH, et al. The efficacy of ultrasonic bone scalpel for unilateral cervical open-door laminoplasty: a randomized controlled trial. Neurosurgery. 86:825–834. 2020.
Article10. Kim P, Murata H, Kurokawa R, Takaishi Y, Asakuno K, Kawamoto T. Myoarchitectonic spinolaminoplasty: efficacy in reconstituting the cervical musculature and preserving biomechanical function. J Neurosurg Spine. 7:293–304. 2007.
Article11. Kowatari K, Ueyama K, Sannohe A, Yamasaki Y. Preserving the C7 spinous process with its muscles attached: effect on axial symptoms after cervical laminoplasty. J Orthop Sci. 14:279–284. 2009.
Article12. Kudo H, Takeuchi K, Yokoyama T, Yamasaki Y, Wada K, Kumagai G, et al. Severe C8 or T1 symptoms after cervical laminoplasty and related factors: are tere any differences between C3-C6 laminoplasty and C3- C7 laminoplasty? Asian Spine J. 13:592–600. 2019.
Article13. Lafage R, Challier V, Liabaud B, Vira S, Ferrero E, Diebo BG, et al. Natural head posture in the setting of sagittal spinal deformity: validation of chin-brow vertical angle, slope of line of sight, and McGregor’s slope with health-related quality of life. Neurosurgery. 79:108–115. 2016.
Article14. Lee S, Chung CK, Kim CH. Risk factor analysis of hinge fusion failure after plate-only open-door laminoplasty. Global Spine J. 5:9–16. 2015.
Article15. Meena RK, Gurjar HK, Singh S, Aggarwal D. Absence of axis (C2) posterior elements leading to C2-C3 instability and myelopathy in young adults. Neurol India. 67:318–321. 2019.16. Muller MP, Tomlinson G, Marrie TJ, Tang P, McGeer A, Low DE, et al. Can routine laboratory tests discriminate between severe acute respiratory syndrome and other causes of community-acquired pneumonia? Clin Infect Dis. 40:1079–1086. 2005.
Article17. Ono A, Tonosaki Y, Numasawa T, Wada K, Yamasaki Y, Tanaka T, et al. The relationship between the anatomy of the nuchal ligament and postoperative axial pain after cervical laminoplasty: cadaver and clinical study. Spine (Phila Pa 1976). 37:E1607–E1613. 2012.18. Schreiber JJ, Anderson PA, Rosas HG, Buchholz AL, Au AG. Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. J Bone Joint Surg Am. 93:1057–1063. 2011.
Article19. Takeuchi K, Yokoyama T, Aburakawa S, Saito A, Numasawa T, Iwasaki T, et al. Axial symptoms after cervical laminoplasty with C3 laminectomy compared with conventional C3-C7 laminoplasty: a modified laminoplasty preserving the semispinalis cervicis inserted into axis. Spine (Phila Pa 1976). 30:2544–2549. 2005.
Article20. Tang JA, Scheer JK, Smith JS, Deviren V, Bess S, Hart RA, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery. 71:662–669. discussion 669. 2012.
Article21. Watanabe M, Sakai D, Yamamoto Y, Iwashina T, Sato M, Mochida J. Upper cervical spinal cord tumors: review of 13 cases. J Orthop Sci. 14:175–181. 2009.
Article22. Zaidi Q, Danisa OA, Cheng W. Measurement techniques and utility of hounsfield unit values for assessment of bone quality prior to spinal instrumentation: a review of current literature. Spine (Phila Pa 1976). 44:E239–E244. 2019.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of Severe Cervical Foraminal Stenosis on Contralateral C7 Nerve Transfer Outcomes
- Axial Neck Pain after Cervical Laminoplasty with Preserving C7 Spinous Process Using C7 Arcocristectomy: A Prospective Study
- The Use of Pedicle Screw-Rod System for the Posterior Fixation in Cervico-Thoracic Junction
- Unveiling and Validating a Modified Method to Assess Cervical Sagittal Alignment as an Effective Substitute for Conventional C2-7 Cobb Angle
- C7 Posterior Fixation Using Intralaminar Screws : Early Clinical and Radiographic Outcome