Korean J Transplant.
2021 Jun;35(2):77-85. 10.4285/kjt.21.0006.
A study on the performance of the Donation Improvement Program in Korea
- Affiliations
-
- 1Korea Organ Donation Agency, Seoul, Korea
- 2Department of Surgery, Seoul National University College of Medicine, Seoul, Korea
- 3Transplantation Research Institute, Medical Research Center, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2517289
- DOI: http://doi.org/10.4285/kjt.21.0006
Abstract
- Background
The Donation Improvement Program (DIP) is intended to increase organ donation at hospitals. The program includes education for healthcare professionals of participating hospitals about each step of donation as well as evaluation. The DIP consists of medical record review (MRR) and a Hospital Attitude Survey (HAS). The purpose of this study was to evaluate the DIP results for the last 7 years.
Methods
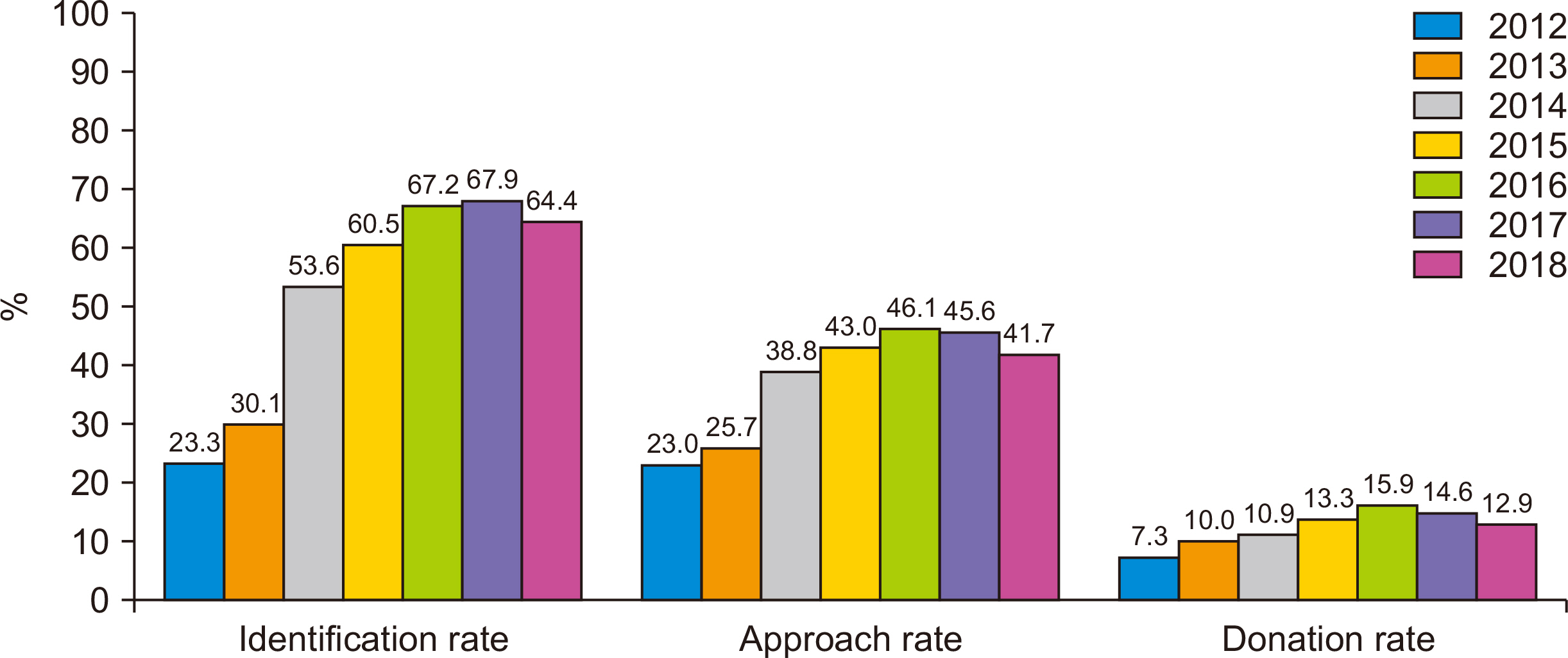
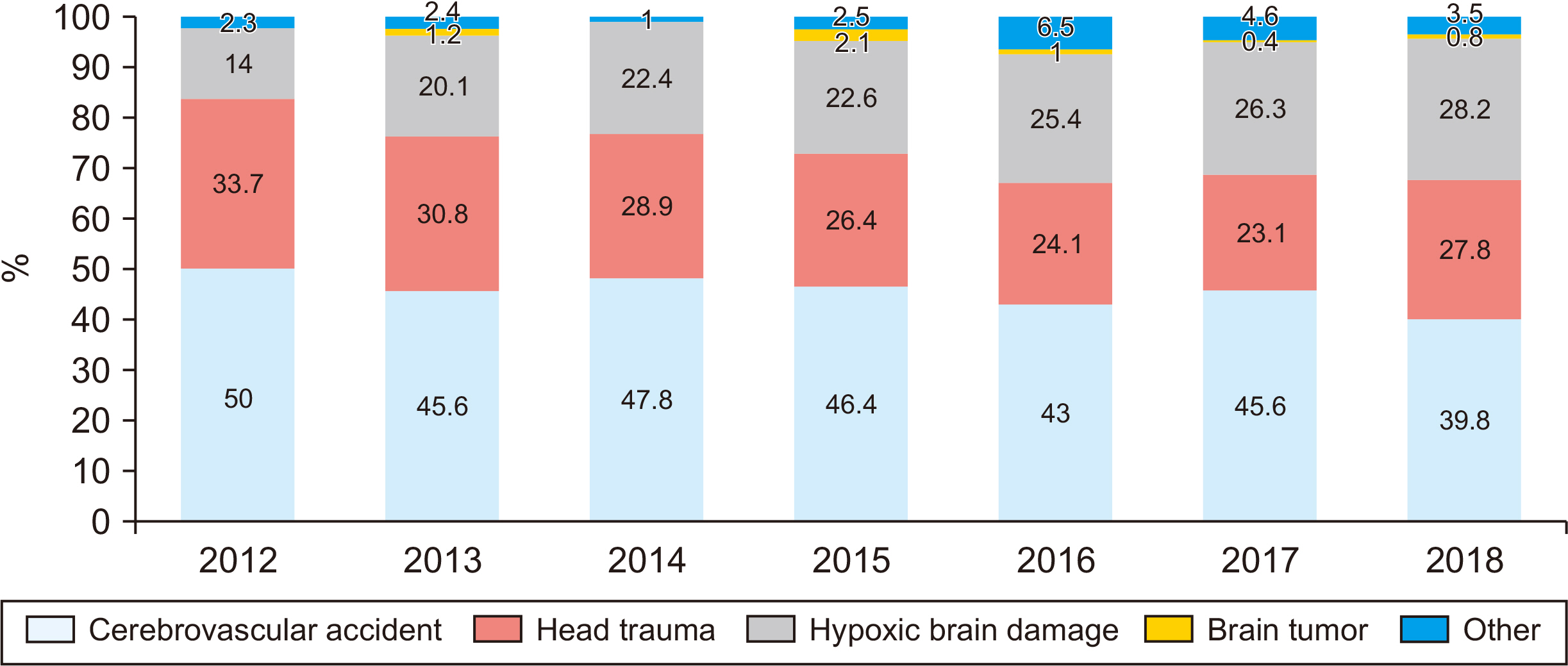
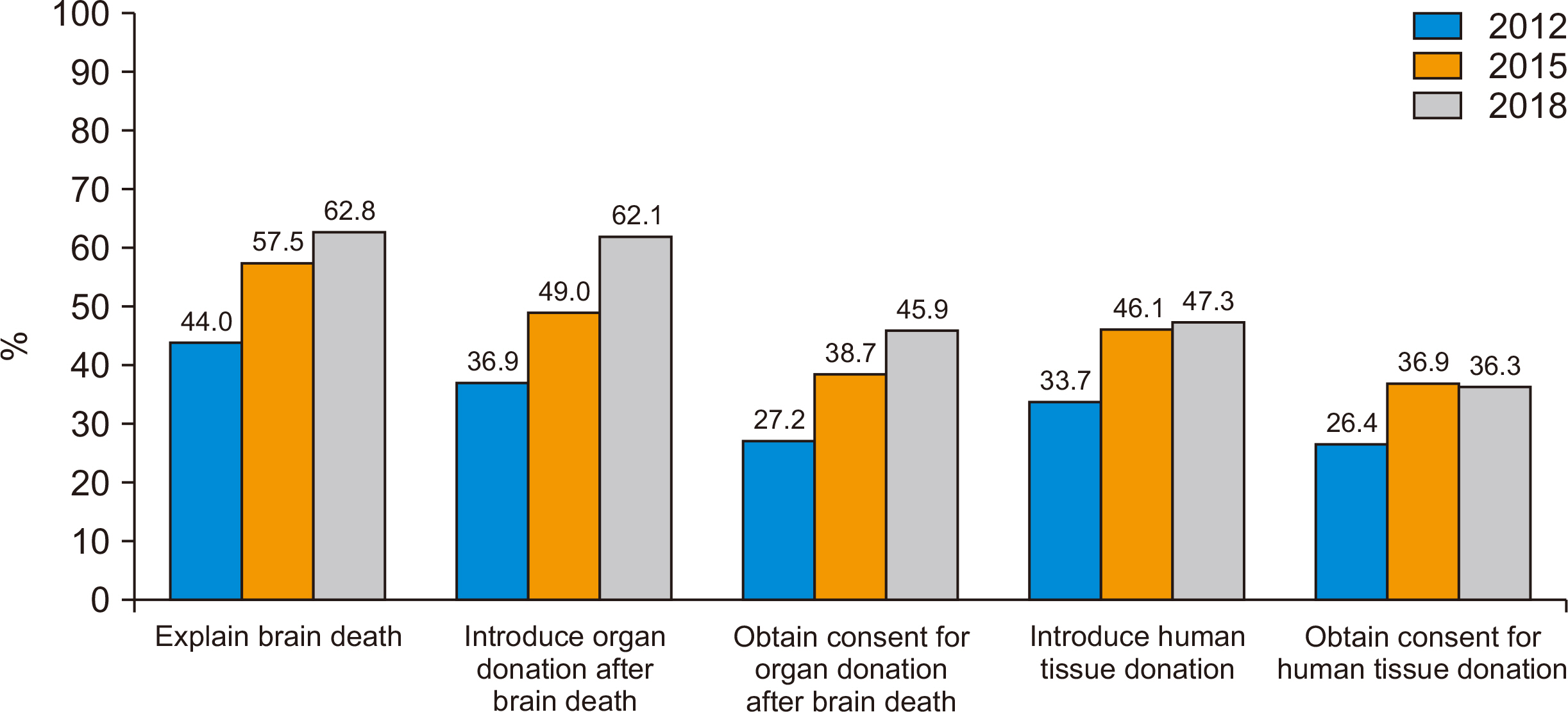
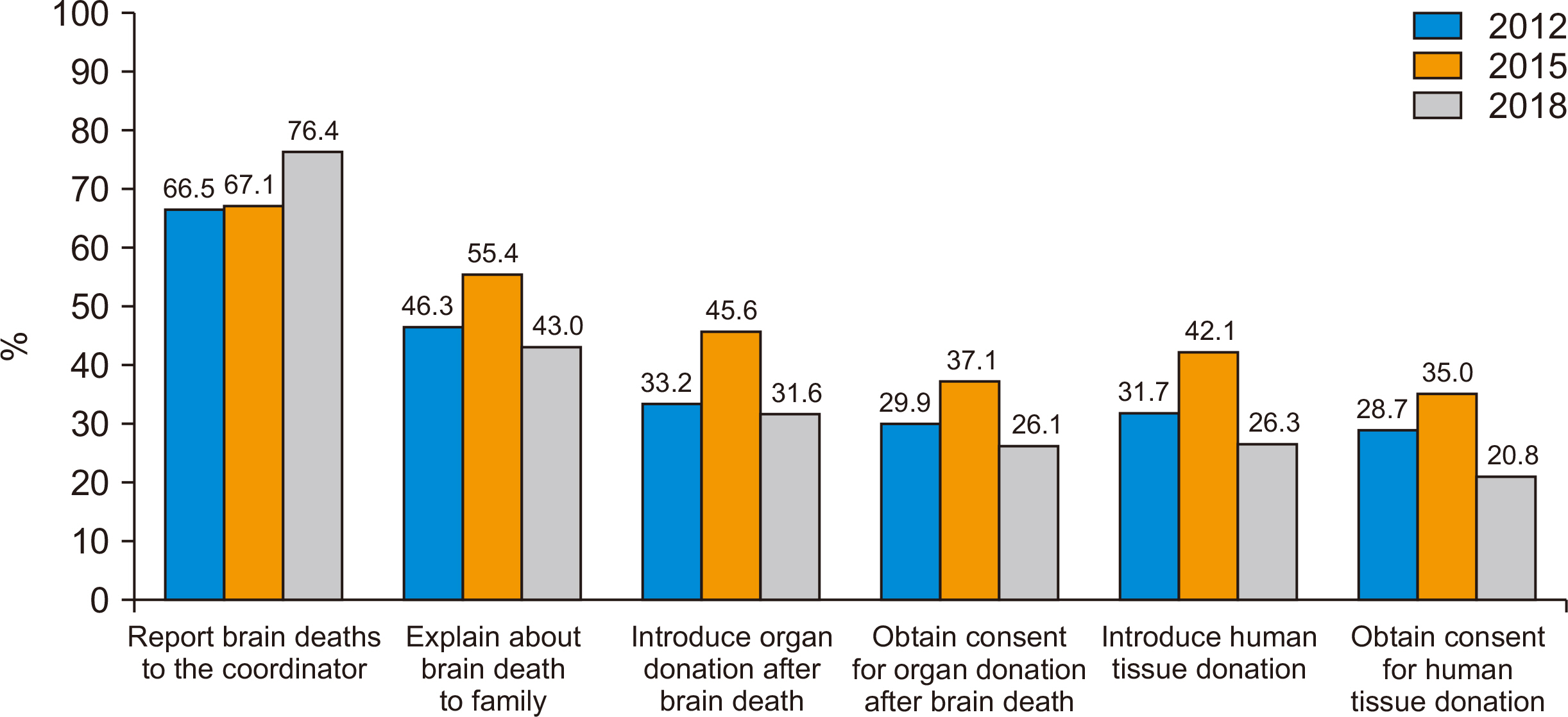
For MRR, we analyzed 58,385 cases of mortality from 77 hospitals between 2012 and 2018. The HAS data for the degree of education experience, competence, and knowledge related to brain death (BD) and donation were analyzed from 23 DIP-participating hospitals in 2012 and 51 DIP-participating hospitals in 2015 and 2018 each.
Results
The recognition rate of potential BD was 24.9%, 61.3%, and 73.2%, and donation rate was 7.5%, 11.7%, and 15.8% at 6 months before, 1–2 years after, and 4–5 years after the agreement, respectively. Hospital staff with the necessary competence or knowledge to explain BD constituted 44.0% in 2012, while this increased to 62.8% in 2018.
Conclusions
The DIP could increase the recognition of BD and the organ donation rate, and positively affect the attitudes of healthcare professionals toward organ donation. Spreading the DIP to all hospitals is urgent to increase organ donation.
Keyword
Figure
Reference
-
1. Cho WH, Kim HT, Lee HJ, Seo YM, Lee SD, Son EI, et al. 2008; Development of Korean model for independent organ procurement organization. J Korean Soc Transplant. 22:109–19.2. Park YJ, Kang H, Kim EM, Shin WY, Yi N, Suh K, et al. 2009; Establishment of active identification and management system for potential brain dead donors in life-link center. J Korean Soc Transplantation. 23:43–51.3. Kim HC, Kim HW. 2013; The issues and suggestions of organ transplant in Korea. Ewha Law J. 17:225–51.4. Gil E, Park JB. 2015; Optimal management of brain death donor. J Korean Soc Transplant. 29:89–100. DOI: 10.4285/jkstn.2015.29.3.89.
Article5. Lee YJ. 2015; Activation policy for brain-dead organ donation. Ewha Med J. 38:1–6. DOI: 10.12771/emj.2015.38.1.1.
Article6. Wight C, Cohen B, Roels L, Miranda B. 2000; Donor action: a quality assurance program for intensive care units that increases organ donation. J Intensive Care Med. 15:104–114. DOI: 10.1177/088506660001500204.
Article7. Park SJ, Yoon YC, Cho WH, Roels L, Smits J, Cohen B, et al. 2012; Preliminary results of donor Action in Korea. J Korean Soc Transplant. 26:101–11. DOI: 10.4285/jkstn.2012.26.2.101.
Article8. International Registry on Organ Donation and Transplantation (IRODaT). 2016. 2016 Newsletter [Internet]. IRODaT;Seoul: Available from: https://www.irodat.org/. cited 2021 Jun 10.9. Korea Organ Donation Agency (KODA). 2019. 2019 Annual report [Internet]. KODA;Seoul: Available from: http://koda1458.kr. cited 2021 Jun 10.10. Ghorbani F, Khoddami-Vishteh HR, Ghobadi O, Shafaghi S, Louyeh AR, Najafizadeh K. 2011; Causes of family refusal for organ donation. Transplant Proc. 43:405–6. DOI: 10.1016/j.transproceed.2011.01.031. PMID: 21440717.
Article11. Korea Organ Donation Agency (KODA). 2019. Notification of potential brain death 2013-2018. KODA;Seoul:12. Vincent A, Logan L. 2012; Consent for organ donation. Br J Anaesth. 108 Suppl 1:i80–7. DOI: 10.1093/bja/aer353. PMID: 22194436.
Article13. Kim MG, Jeong JC, Cho EJ, Huh KH, Yang J, Byeon NI, et al. 2010; Operational and regulatory system requirements for pursuing self-sufficiency in deceased donor organ transplantation program in Korea. J Korean Soc Transplant. 24:147–58. DOI: 10.4285/jkstn.2010.24.3.147.
Article14. Lenzi JA, Sarlo R, Assis A, Ponte M, Paura P, Araújo C, et al. 2014; Family informed consent to organ donation--who performs better: organ procurement organizations, in-hospital coordinators, or intensive care unit professionals? Transplant Proc. 46:1672–3. DOI: 10.1016/j.transproceed.2014.05.036. PMID: 25131009.
Article15. Rodrigue JR, Cornell DL, Howard RJ. 2006; Organ donation decision: comparison of donor and nondonor families. Am J Transplant. 6:190–8. DOI: 10.1111/j.1600-6143.2005.01130.x. PMID: 16433774. PMCID: PMC2365918.
Article16. Roels L, Spaight C, Smits J, Cohen B. 2010; Critical care staffs’ attitudes, confidence levels and educational needs correlate with countries’ donation rates: data from the Donor Action database. Transpl Int. 23:842–50. DOI: 10.1111/j.1432-2277.2010.01065.x. PMID: 20210934.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Study on the Relationship between the Awareness of Blood Program and the Blood Donation Experience
- A Study about the Directed blood donation program
- Receiving a donation call to dissection tables: various aspects of whole-body donation in northern union territory region medical college of India
- Educational Outcomes and Perception Changes in Medical Students After Visiting a Blood Donation Center
- Program to Activate the Notification of the Potential Donors