Blood Res.
2021 Jun;56(2):72-78. 10.5045/br.2021.2020328.
Clinical impact of lymphatic spread in patients with limited-stage upper aerodigestive tract NK/T cell lymphoma
- Affiliations
-
- 1Department of Hematology, Hanyang University Hanmaeum Changwon Hospital, Changwon, Busan, Korea
- 2Department of Hematology-Oncology, Pusan National University Hospital Medical Research Institute, Busan, Korea
- 3Department of Oncology, Dong-A University Hospital, Busan, Korea
- 4Department of Hematology, Busan Haeundae Paik Hospital, Busan, Korea
- 5Department of Hematology, Busan Paik Hospital, Busan, Korea
- KMID: 2517003
- DOI: http://doi.org/10.5045/br.2021.2020328
Abstract
- Background
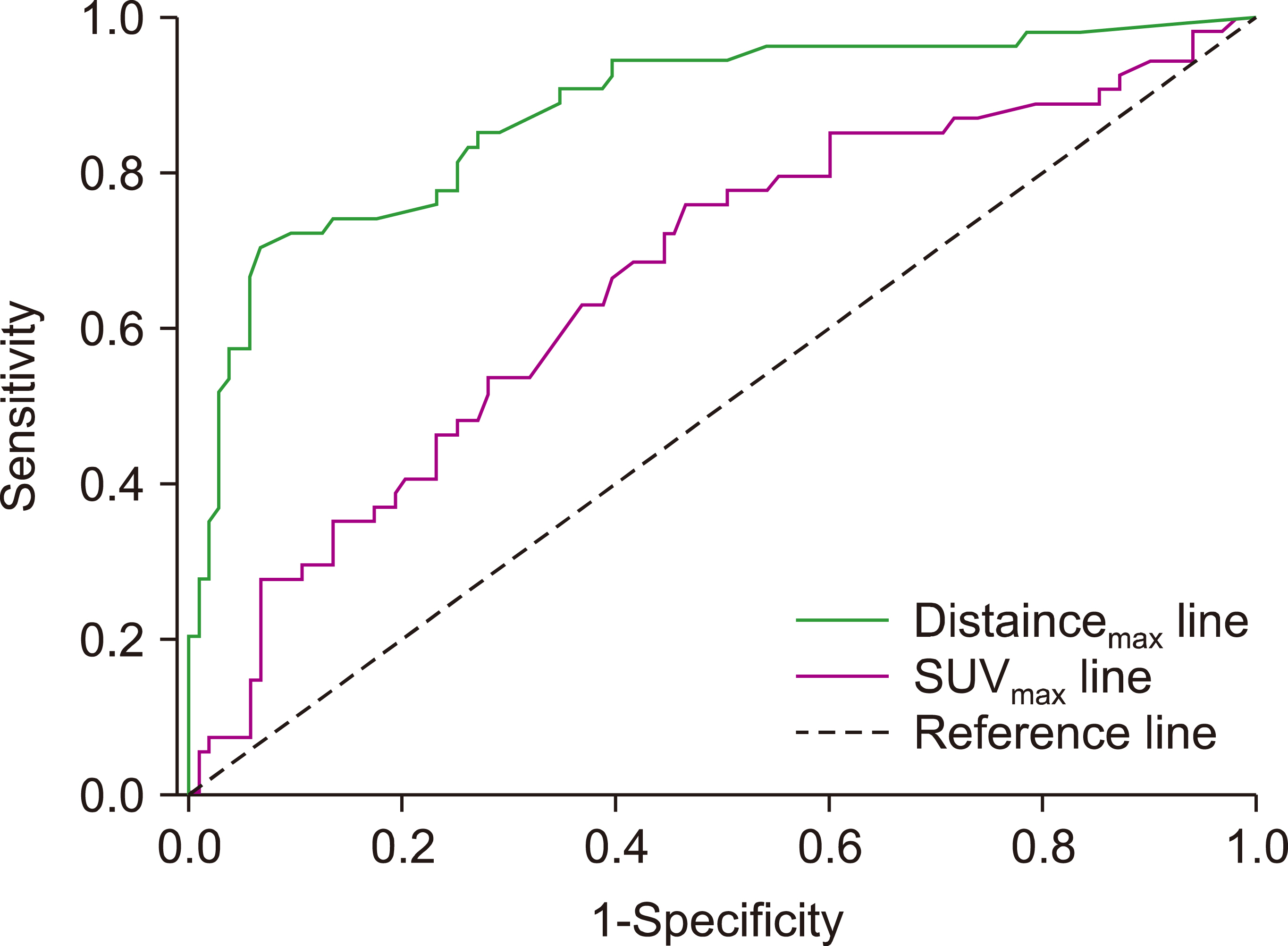
We investigated whether distance max , that is, the degree of distance between the upper aerodigestive tract (UAT) mass and the farthest pathologic lymph node, was significantly associated with survival in patients with limited-stage UAT natural killer/T cell lymphoma (NKTCL).
Methods
A total of 157 patients who received chemotherapy (CTx) with/without radiotherapy (RTx) were enrolled.
Results
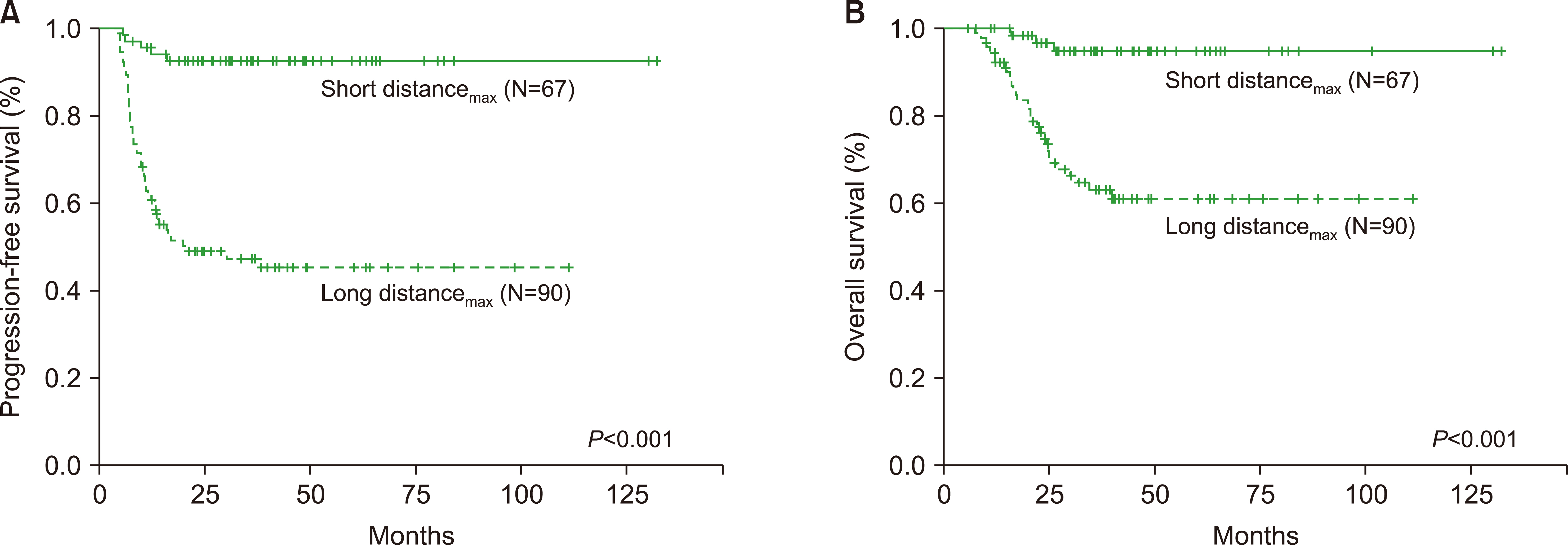
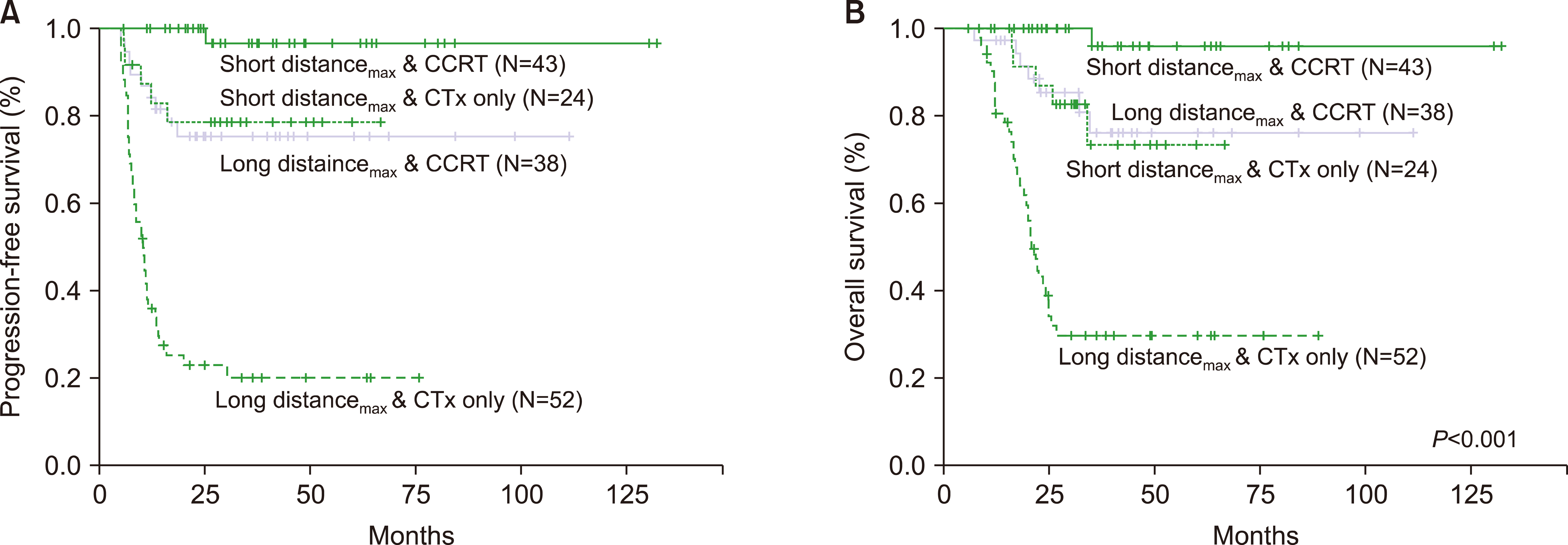
In the survival analysis, an elevated lactate dehydrogenase level [progression-free survival (PFS): hazard ratio (HR), 2.948; 95% confidence interval (CI), 1.606‒5.404; P <0.001; overall survival (OS): HR, 2.619; 95% CI, 1.594‒4.822; P =0.003], short distance max (PFS: HR, 0.170; 95% CI, 0.071‒0.410; P <0.001; OS: HR, 0.142; 95% CI, 0.050‒0.402; P < 0.001), and CTx combined with RTx (HR, 0.168; 95%CI, 0.079‒0.380; P < 0.001; OS: HR, 0.193; 95% CI, 0.087‒0.429; P <0.001) had an independent predictive value for PFS and OS.
Conclusion
The evaluation of the degree of lymphatic spread and local control by CTx combined with RTx is essential in patients with limited-stage UAT NKTCL.
Figure
Reference
-
1. Au WY, Weisenburger DD, Intragumtornchai T, et al. 2009; Clinical differences between nasal and extranasal natural killer/T-cell lymphoma: a study of 136 cases from the International Peripheral T-Cell Lymphoma Project. Blood. 113:3931–7. DOI: 10.1182/blood-2008-10-185256. PMID: 19029440.
Article2. Suzuki R, Suzumiya J, Yamaguchi M, et al. 2010; Prognostic factors for mature natural killer (NK) cell neoplasms: aggressive NK cell leukemia and extranodal NK cell lymphoma, nasal type. Ann Oncol. 21:1032–40. DOI: 10.1093/annonc/mdp418. PMID: 19850638.
Article3. Kim TM, Lee SY, Jeon YK, et al. 2008; Clinical heterogeneity of extranodal NK/T-cell lymphoma, nasal type: a national survey of the Korean Cancer Study Group. Ann Oncol. 19:1477–84. DOI: 10.1093/annonc/mdn147. PMID: 18385201.
Article4. Chan JY, Lim ST. 2018; Novel findings from the Asian Lymphoma Study Group: focus on T and NK-cell lymphomas. Int J Hematol. 107:413–9. DOI: 10.1007/s12185-018-2406-6. PMID: 29380182.
Article5. Jo JC, Yoon DH, Kim S, et al. 2012; Clinical features and prognostic model for extranasal NK/T-cell lymphoma. Eur J Haematol. 89:103–10. DOI: 10.1111/j.1600-0609.2012.01796.x. PMID: 22553935.
Article6. Avilés A, Díaz NR, Neri N, Cleto S, Talavera A. 2000; Angiocentric nasal T/natural killer cell lymphoma: a single centre study of prognostic factors in 108 patients. Clin Lab Haematol. 22:215–20. DOI: 10.1046/j.1365-2257.2000.00307.x. PMID: 11012633.
Article7. Li CC, Tien HF, Tang JL, et al. 2004; Treatment outcome and pattern of failure in 77 patients with sinonasal natural killer/T-cell or T-cell lymphoma. Cancer. 100:366–75. DOI: 10.1002/cncr.11908. PMID: 14716773.
Article8. Ko YH, Cho EY, Kim JE, et al. 2004; NK and NK-like T-cell lymphoma in extranasal sites: a comparative clinicopathological study according to site and EBV status. Histopathology. 44:480–9. DOI: 10.1111/j.1365-2559.2004.01867.x. PMID: 15139996.
Article9. Cheung MM, Chan JK, Lau WH, et al. 1998; Primary non-Hodgkin's lymphoma of the nose and nasopharynx: clinical features, tumor immunophenotype, and treatment outcome in 113 patients. J Clin Oncol. 16:70–7. DOI: 10.1200/JCO.1998.16.1.70. PMID: 9440725.
Article10. Cheung MM, Chan JK, Lau WH, Ngan RK, Foo WW. 2002; Early stage nasal NK/T-cell lymphoma: clinical outcome, prognostic factors, and the effect of treatment modality. Int J Radiat Oncol Biol Phys. 54:182–90. DOI: 10.1016/S0360-3016(02)02916-4. PMID: 12182990.
Article11. Chim CS, Ma SY, Au WY, et al. 2004; Primary nasal natural killer cell lymphoma: long-term treatment outcome and relationship with the International Prognostic Index. Blood. 103:216–21. DOI: 10.1182/blood-2003-05-1401. PMID: 12933580.
Article12. You JY, Chi KH, Yang MH, et al. 2004; Radiation therapy versus chemotherapy as initial treatment for localized nasal natural killer (NK)/T-cell lymphoma: a single institute survey in Taiwan. Ann Oncol. 15:618–25. DOI: 10.1093/annonc/mdh143. PMID: 15033670.13. Kim K, Kim WS, Jung CW, et al. 2002; Clinical features of peripheral T-cell lymphomas in 78 patients diagnosed according to the Revised European-American lymphoma (REAL) classification. Eur J Cancer. 38:75–81. DOI: 10.1016/S0959-8049(01)00344-6. PMID: 11750843.
Article14. Lee J, Park YH, Kim WS, et al. 2005; Extranodal nasal type NK/T-cell lymphoma: elucidating clinical prognostic factors for risk-based stratification of therapy. Eur J Cancer. 41:1402–8. DOI: 10.1016/j.ejca.2005.03.010. PMID: 15963893.
Article15. Kim TM, Park YH, Lee SY, et al. 2005; Local tumor invasiveness is more predictive of survival than International Prognostic Index in stage I(E)/II(E) extranodal NK/T-cell lymphoma, nasal type. Blood. 106:3785–90. DOI: 10.1182/blood-2005-05-2056. PMID: 16109779.
Article16. Lee J, Suh C, Park YH, et al. 2006; Extranodal natural killer T-cell lymphoma, nasal-type: a prognostic model from a retrospective multicenter study. J Clin Oncol. 24:612–8. DOI: 10.1200/JCO.2005.04.1384. PMID: 16380410.
Article17. Yan Z, Huang HQ, Wang XX, et al. 2015; A TNM staging system for nasal NK/T-cell lymphoma. PLoS One. 10:e0130984. DOI: 10.1371/journal.pone.0130984. PMID: 26098892. PMCID: PMC4476596.
Article18. Kim SJ, Yoon DH, Jaccard A, et al. 2016; A prognostic index for natural killer cell lymphoma after non-anthracycline-based treatment: a multicentre, retrospective analysis. Lancet Oncol. 17:389–400. DOI: 10.1016/S1470-2045(15)00533-1. PMID: 26873565.
Article19. Cheson BD, Horning SJ, Coiffier B, et al. 1999; Report of an international workshop to standardize response criteria for non-Hodgkin's lymphomas. NCI Sponsored International Working Group. J Clin Oncol. 17:1244. DOI: 10.1200/JCO.1999.17.4.1244. PMID: 10561185.20. Robbins KT, Fuller LM, Vlasak M, et al. 1985; Primary lymphomas of the nasal cavity and paranasal sinuses. Cancer. 56:814–9. DOI: 10.1002/1097-0142(19850815)56:4<814::AID-CNCR2820560419>3.0.CO;2-P. PMID: 4016673.
Article21. Logsdon MD, Ha CS, Kavadi VS, Cabanillas F, Hess MA, Cox JD. 1997; Lymphoma of the nasal cavity and paranasal sinuses: improved outcome and altered prognostic factors with combined modality therapy. Cancer. 80:477–88. DOI: 10.1002/(SICI)1097-0142(19970801)80:3<477::AID-CNCR16>3.0.CO;2-U. PMID: 9241082.22. Li YX, Fang H, Liu QF, et al. 2008; Clinical features and treatment outcome of nasal-type NK/T-cell lymphoma of Waldeyer ring. Blood. 112:3057–64. DOI: 10.1182/blood-2008-05-160176. PMID: 18676879.
Article23. Li YX, Liu QF, Fang H, et al. 2009; Variable clinical presentations of nasal and Waldeyer ring natural killer/T-cell lymphoma. Clin Cancer Res. 15:2905–12. DOI: 10.1158/1078-0432.CCR-08-2914. PMID: 19318493.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epstein-Barr Viral RNA(EBERs) Expression in Conventional Malignant Lymphoma and Polymorphic Reticulosis of Upper Aerodigestive Tract
- A Case of Primary CD56+ T/NK Cell Lymphoma of the Colon
- Characteristics, Prognostic Factors, and Survival of Patients with NK/T-Cell Lymphoma of Non-upper Aerodigestive Tract: A 17-Year Single-Center Experience
- Therapeutic Outcome of Epstein-Barr Virus Positive T/NK Cell Lymphoma in the Upper Aerodigestive Tract
- A Case of Extranodall NK/T-cell Lymphoma, Nasal type