J Korean Med Sci.
2021 Jun;36(24):e179. 10.3346/jkms.2021.36.e179.
Source Analysis and Effective Control of a COVID-19 Outbreak in a University Teaching Hospital during a Period of Increasing Community Prevalence of COVID-19
- Affiliations
-
- 1Department of Infection Control Unit, Chonnam National University Hospital, Gwangju, Korea
- 2Department of Infectious Diseases, Chonnam National University Hospital, Gwangju, Korea
- 3Department of Laboratory Medicine, Chonnam National University Hospital, Gwangju, Korea
- 4Department of Infectious Diseases, Chonnam National University Medical School, Gwangju, Korea
- KMID: 2516768
- DOI: http://doi.org/10.3346/jkms.2021.36.e179
Abstract
- Background
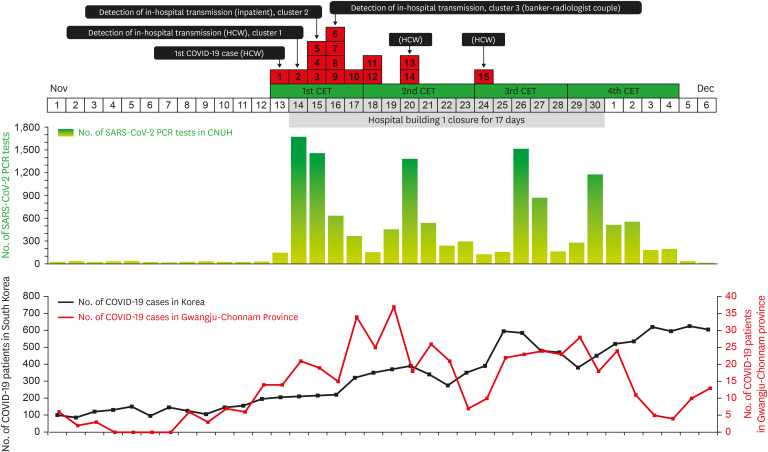
South Korea has been experiencing a third wave of coronavirus disease 2019 (COVID-19) since mid-November 2020. Our hospital in Gwangju metropolitan city experienced a healthcare-associated COVID-19 outbreak early in the third wave. The first confirmed COVID-19 patient was a symptomatic neurosurgery resident with high mobility throughout the hospital. We analyzed the transmission routes of nosocomial COVID-19 and discussed infection control strategies.
Methods
We retrospectively analyzed the severe acute respiratory syndrome coronavirus 2 reverse transcription-polymerase chain reaction (RT-PCR) testing results according to time point and evaluated transmission routes.
Results
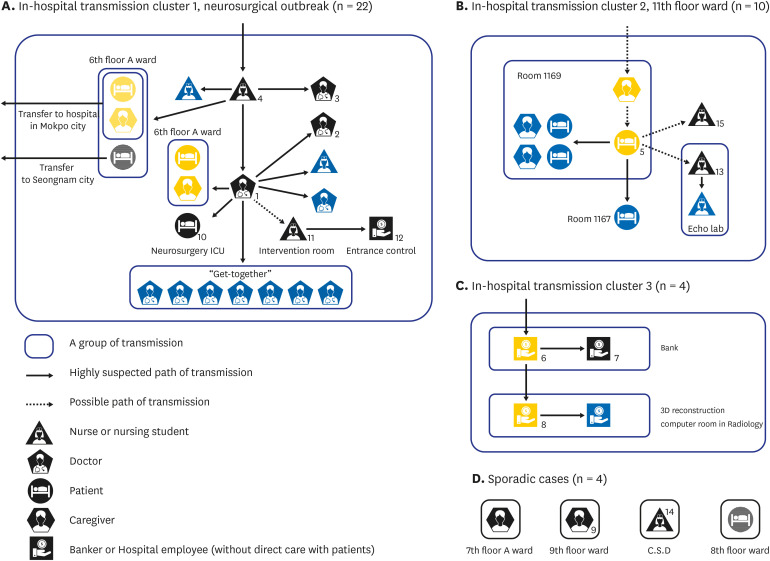
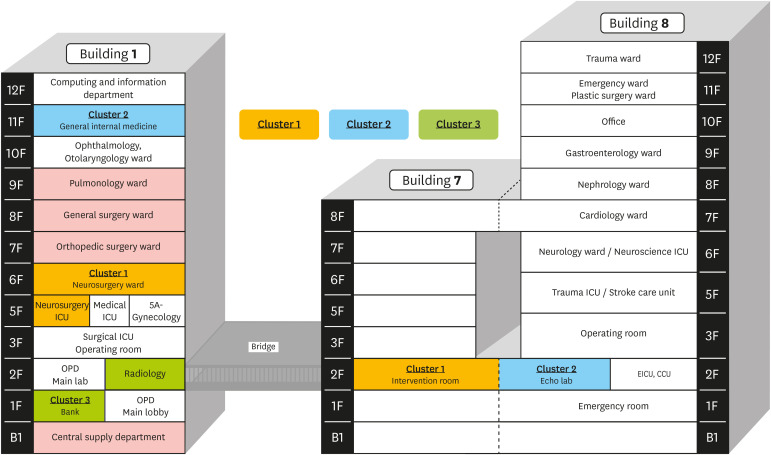
Since COVID-19 was first confirmed in a healthcare worker (HCW) on 11/13/2020, we performed RT-PCR tests for all patients and caregivers and four complete enumeration surveys for all HCWs. We detected three clusters of nosocomial spread and several sporadic cases. The first cluster originated from the community outbreak spot, where an asymptomatic HCW visited, which led to a total of 22 cases. The second cluster, which included patient-to-patient transmission, originated from a COVID-19 positive caregiver before diagnosis and the third cluster involved a radiologist and a banker. We took measures to isolate Building 1 of the hospital for 17 days and controlled the outbreak during a period of increasing community COVID-19 prevalence. Universal screening of all inpatients upon admission and resident caregivers was made mandatory and hospital-related employees are now screened monthly.
Conclusion
Infection control strategies to prevent the nosocomial transmission of emerging infectious diseases must correspond with community disease prevalence. Our data reinforce the importance of multi-time point surveillance of asymptomatic HCWs and routine surveillance of patients and caregivers during an epidemic.
Figure
Cited by 2 articles
-
Risk of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Transmission Among Healthcare Workers Dining in Hospital Staff Cafeterias
Jiwon Jung, Young-Ju Lim, Eun Ok Kim, Sung-Han Kim
J Korean Med Sci. 2021;37(2):e14. doi: 10.3346/jkms.2022.37.e14.Guidelines for Infection and Burnout Prevention in COVID-19 Healthcare Workers
Se Yoon Park, Hae Suk Cheong, Ki Tae Kwon, Kyung Mok Sohn, Sang Taek Heo, Shinwon Lee, Un Sun Chung, So Hee Lee
Korean J Healthc Assoc Infect Control Prev. 2023;28(1):50-63. doi: 10.14192/kjicp.2023.28.1.50.
Reference
-
1. Keeley AJ, Evans C, Colton H, Ankcorn M, Cope A, State A, et al. Roll-out of SARS-CoV-2 testing for healthcare workers at a large NHS Foundation Trust in the United Kingdom, March 2020. Euro Surveill. 2020; 25(14):2000433.
Article2. Wong SC, Kwong RT, Wu TC, Chan JW, Chu MY, Lee SY, et al. Risk of nosocomial transmission of coronavirus disease 2019: an experience in a general ward setting in Hong Kong. J Hosp Infect. 2020; 105(2):119–127. PMID: 32259546.
Article3. Kim SW, Jo SJ, Lee H, Oh JH, Lim J, Lee SH, et al. Containment of a healthcare-associated COVID-19 outbreak in a university hospital in Seoul, Korea: a single-center experience. PLoS One. 2020; 15(8):e0237692. PMID: 32797094.
Article4. Schlosser M, Signorelli H, Gregg W, Korwek K, Sands K. COVID-19 testing processes and patient protections for resumption of elective surgery. Am J Surg. 2021; 221(1):49–52. PMID: 32736801.
Article5. World Health Organization. Contact tracing in the context of COVID-19. Updated 2021. Accessed May 6, 2021. https://www.who.int/publications/i/item/contact-tracing-in-the-context-of-covid-19.6. Kronbichler A, Kresse D, Yoon S, Lee KH, Effenberger M, Shin JI. Asymptomatic patients as a source of COVID-19 infections: a systematic review and meta-analysis. Int J Infect Dis. 2020; 98:180–186. PMID: 32562846.
Article7. Black JR, Bailey C, Przewrocka J, Dijkstra KK, Swanton C. COVID-19: the case for health-care worker screening to prevent hospital transmission. Lancet. 2020; 395(10234):1418–1420. PMID: 32305073.
Article8. Fennelly K, Whalen CC. Asymptomatic health-care worker screening during the COVID-19 pandemic. Lancet. 2020; 396(10260):1393.
Article9. Htun HL, Lim DW, Kyaw WM, Loh WJ, Lee LT, Ang B, et al. Responding to the COVID-19 outbreak in Singapore: staff protection and staff temperature and sickness surveillance systems. Clin Infect Dis. 2020; 71(8):1947–1952. PMID: 32315026.
Article10. Alshehari AA, Park S, Rashid H. Strategies to improve hand hygiene compliance among healthcare workers in adult intensive care units: a mini systematic review. J Hosp Infect. 2018; 100(2):152–158. PMID: 29559231.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cardiovascular Imaging Asia in the Era of the COVID-19 Outbreak
- Changes in the prevalence of metabolic syndrome in Korean adults after the COVID-19 outbreak
- Assessment and Management of Dysphagia during the COVID-19 Pandemic
- Hospital Infection Control Practice in the COVID-19 Era: An Experience of University Affiliated Hospital
- COVID-19 and Fungal Infection