J Korean Med Sci.
2021 Jun;36(23):e151. 10.3346/jkms.2021.36.e151.
Incidence, Management, and Prognosis of Graft Failure and Autologous Reconstitution after Allogeneic Hematopoietic Stem Cell Transplantation
- Affiliations
-
- 1Department of Hematology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2516676
- DOI: http://doi.org/10.3346/jkms.2021.36.e151
Abstract
- Background
This study presents outcomes of management in graft failure (GF) after allogeneic hematopoietic stem cell transplantation (HCT) and provides prognostic information including rare cases of autologous reconstitution (AR).
Methods
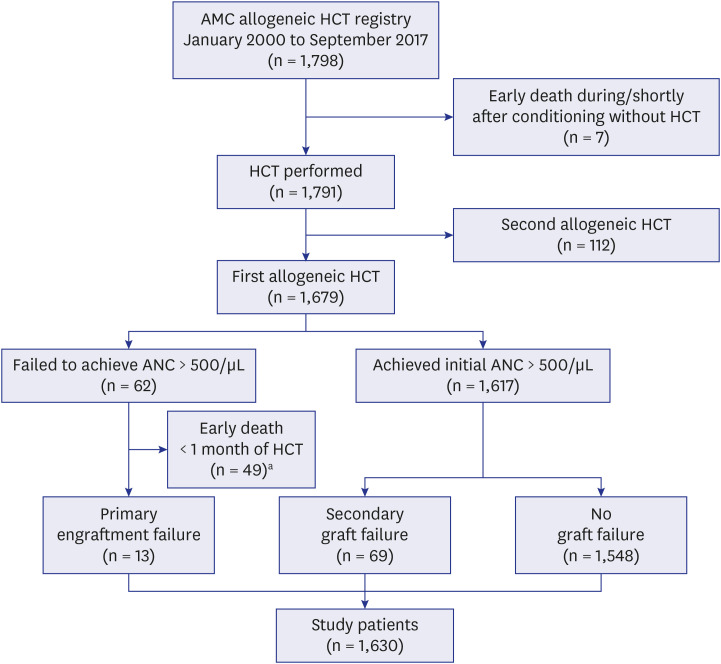
We analyzed risk factors and outcomes of primary and secondary GF, and occurrence of AR in 1,630 HCT recipients transplanted over period of 18 years (January 2000– September 2017) at our center.
Results
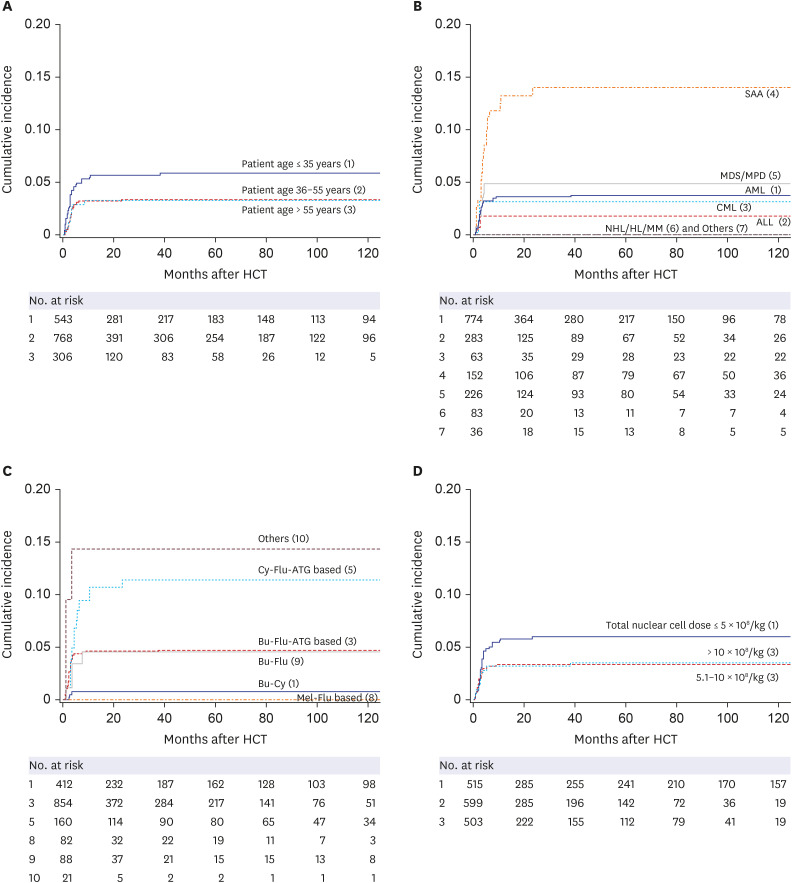
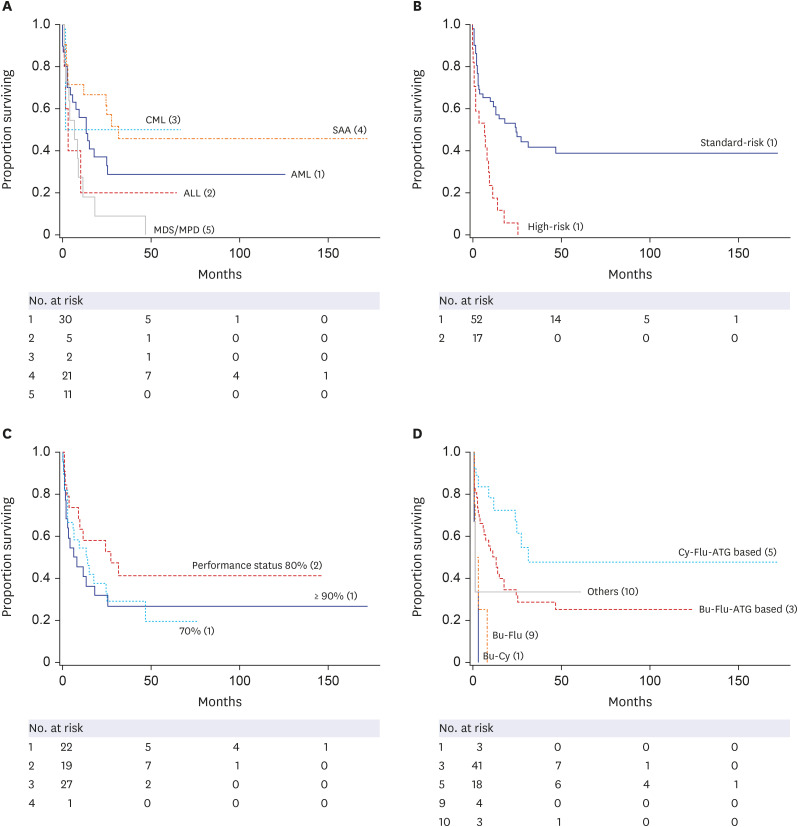
Primary and secondary GF occurred in 13 (0.80%), and 69 patients (10-year cumulative incidence, 4.5%) respectively. No peri-transplant variables predicted primary GF, whereas reduced intensity conditioning (RIC) regimen (relative risk [RR], 0.97–28.0, P < 0.001) and lower CD34 + cell dose (RR, 2.44–2.84, P = 0.002) were associated with higher risk of secondary GF in multivariate analysis. Primary GF demonstrated 100% mortality, in the secondary GF group, the 5-year Kaplan-Meier survival rate was 28.8%, relapse ensued in 18.8%, and AR was observed in 11.6% (n = 8). In survival analysis, diagnosis of aplastic anemia (AA), chronic myeloid leukemia and use of RIC had a positive impact. There were 8 patients who experienced AR, which was rarely reported after transplantation for acute leukemia. Patient shared common characteristics such as young age (median 25 years), use of RIC regimen, absence of profound neutropenia, and had advantageous survival rate of 100% during follow period without relapse.
Conclusion
Primary GF exhibited high mortality rate. Secondary GF had 4.5% 10-year cumulative incidence, median onset of 3 months after HCT, and showed 5-year Kaplan-Meier survival of 28.8%. Diagnosis of severe AA and use of RIC was both associated with higher incidence and better survival rate in secondary GF group. AR occurred in 11.6% in secondary GF, exhibited excellent prognosis.
Keyword
Figure
Reference
-
1. Olsson R, Remberger M, Schaffer M, Berggren DM, Svahn BM, Mattsson J, et al. Graft failure in the modern era of allogeneic hematopoietic SCT. Bone Marrow Transplant. 2013; 48(4):537–543. PMID: 23222384.
Article2. Cluzeau T, Lambert J, Raus N, Dessaux K, Absi L, Delbos F, et al. Risk factors and outcome of graft failure after HLA matched and mismatched unrelated donor hematopoietic stem cell transplantation: a study on behalf of SFGM-TC and SFHI. Bone Marrow Transplant. 2016; 51(5):687–691. PMID: 26855158.
Article3. Piccin A, McCann S, Socié G, Oneto R, Bacigalupo A, Locasciulli A, et al. Survival of patients with documented autologous recovery after SCT for severe aplastic anemia: a study by the WPSAA of the EBMT. Bone Marrow Transplant. 2010; 45(6):1008–1013. PMID: 19915627.
Article4. Olsson RF, Logan BR, Chaudhury S, Zhu X, Akpek G, Bolwell BJ, et al. Primary graft failure after myeloablative allogeneic hematopoietic cell transplantation for hematologic malignancies. Leukemia. 2015; 29(8):1754–1762. PMID: 25772027.
Article5. Rondón G, Saliba RM, Khouri I, Giralt S, Chan K, Jabbour E, et al. Long-term follow-up of patients who experienced graft failure postallogeneic progenitor cell transplantation. Results of a single institution analysis. Biol Blood Marrow Transplant. 2008; 14(8):859–866. PMID: 18640568.
Article6. Champlin RE, Horowitz MM, van Bekkum DW, Camitta BM, Elfenbein GE, Gale RP, et al. Graft failure following bone marrow transplantation for severe aplastic anemia: risk factors and treatment results. Blood. 1989; 73(2):606–613. PMID: 2644980.
Article7. Petersdorf EW. Risk assessment in haematopoietic stem cell transplantation: histocompatibility. Best Pract Res Clin Haematol. 2007; 20(2):155–170. PMID: 17448954.
Article8. Alchalby H, Yunus DR, Zabelina T, Ayuk F, Kröger N. Incidence and risk factors of poor graft function after allogeneic stem cell transplantation for myelofibrosis. Bone Marrow Transplant. 2016; 51(9):1223–1227. PMID: 27088376.
Article9. Storb R, Prentice RL, Thomas ED. Marrow transplantation for treatment of aplastic anemia. An analysis of factors associated with graft rejection. N Engl J Med. 1977; 296(2):61–66. PMID: 136605.10. Saad A, Lamb LS. Ex vivo T-cell depletion in allogeneic hematopoietic stem cell transplant: past, present and future. Bone Marrow Transplant. 2017; 52(9):1241–1248. PMID: 28319073.
Article11. Beatty PG, Clift RA, Mickelson EM, Nisperos BB, Flournoy N, Martin PJ, et al. Marrow transplantation from related donors other than HLA-identical siblings. N Engl J Med. 1985; 313(13):765–771. PMID: 3897863.
Article12. Remberger M, Watz E, Ringdén O, Mattsson J, Shanwell A, Wikman A. Major ABO blood group mismatch increases the risk for graft failure after unrelated donor hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2007; 13(6):675–682. PMID: 17531777.
Article13. Anasetti C, Amos D, Beatty PG, Appelbaum FR, Bensinger W, Buckner CD, et al. Effect of HLA compatibility on engraftment of bone marrow transplants in patients with leukemia or lymphoma. N Engl J Med. 1989; 320(4):197–204. PMID: 2643045.
Article14. Gaziev J, Sodani P, Lucarelli G, Polchi P, Marktel S, Paciaroni K, et al. Second hematopoietic SCT in patients with thalassemia recurrence following rejection of the first graft. Bone Marrow Transplant. 2008; 42(6):397–404. PMID: 18574445.
Article15. Massenkeil G, Nagy M, Neuburger S, Tamm I, Lutz C, le Coutre P, et al. Survival after reduced-intensity conditioning is not inferior to standard high-dose conditioning before allogeneic haematopoietic cell transplantation in acute leukaemias. Bone Marrow Transplant. 2005; 36(8):683–689. PMID: 16113673.
Article16. Brunstein CG, Hirsch BA, Miller JS, McGlennen RC, Verfaillie CM, McGlave PB, et al. Non-leukemic autologous reconstitution after allogeneic bone marrow transplantation for Ph-positive chronic myelogenous leukemia: extended remission preceding eventual relapse. Bone Marrow Transplant. 2000; 26(11):1173–1177. PMID: 11149727.
Article17. Scrucca L, Santucci A, Aversa F. Competing risk analysis using R: an easy guide for clinicians. Bone Marrow Transplant. 2007; 40(4):381–387. PMID: 17563735.
Article18. Klein JP, Moeschberger ML, editors. Survival Analysis: Techniques for Censored and Truncated Data. Berlin, Germany: Springer Science & Business Media;2006.19. Bradburn MJ, Clark TG, Love SB, Altman DG. Survival analysis part II: multivariate data analysis--an introduction to concepts and methods. Br J Cancer. 2003; 89(3):431–436. PMID: 12888808.20. Schriber J, Agovi MA, Ho V, Ballen KK, Bacigalupo A, Lazarus HM, et al. Second unrelated donor hematopoietic cell transplantation for primary graft failure. Biol Blood Marrow Transplant. 2010; 16(8):1099–1106. PMID: 20172038.
Article21. Rubio MT, Savani BN, Labopin M, Polge E, Niederwieser D, Ganser A, et al. The impact of HLA-matching on reduced intensity conditioning regimen unrelated donor allogeneic stem cell transplantation for acute myeloid leukemia in patients above 50 years-a report from the EBMT acute leukemia working party. J Hematol Oncol. 2016; 9(1):65. PMID: 27488518.
Article22. Harada K, Fuji S, Seo S, Kanda J, Ueki T, Kimura F, et al. Comparison of the outcomes after haploidentical and cord blood salvage transplantations for graft failure following allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 2020; 55(9):1784–1795. PMID: 32051535.
Article23. Rudakova T, Kulagin A, Moiseev I, Bykova T, Bondarenko S, Barabanshikova M, et al. Thrombopoietin receptor agonists for treatment of poor graft function after allogeneic hematopoietic stem cell transplantation in adults. Cell Ther Transplant. 2019; 8(2):38–44.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Quality of Life of Autologous and Allogeneic Hematopoietic Stem Cell Transplantation Recipients
- A case of pneumomediastinum combined with chronic graft-versus-host disease following allogeneic hematopoietic stem cell transplantation
- Clinical Correlation of CD4+CD25+ Regulatory T Cells in Early Immune Reconstitution after Myeloablative Allogeneic Stem Cell Transplantation
- Hematopoietic stem cell transplantation: overview for general pediatrician
- Factors influencing lymphocyte reconstitution after allogeneic hematopoietic stem cell transplantation in children