J Korean Med Sci.
2021 Jun;36(22):e149. 10.3346/jkms.2021.36.e149.
An Evaluation of the Effect of Performance Improvement and Patient Safety Program Implemented in a New Regional Trauma Center of Korea
- Affiliations
-
- 1Division of Trauma Surgery, Department of Surgery, Ajou University School of Medicine, Suwon, Korea
- 2Gyeonggi South Regional Trauma Center, Ajou University Hospital, Suwon, Korea
- KMID: 2516579
- DOI: http://doi.org/10.3346/jkms.2021.36.e149
Abstract
- Background
This study examined the impact of the performance improvement and patient safety (PIPS) program implemented in 2015 on outcomes for trauma patients in a regional trauma center established by a government-led project for a national trauma system in Korea.
Methods
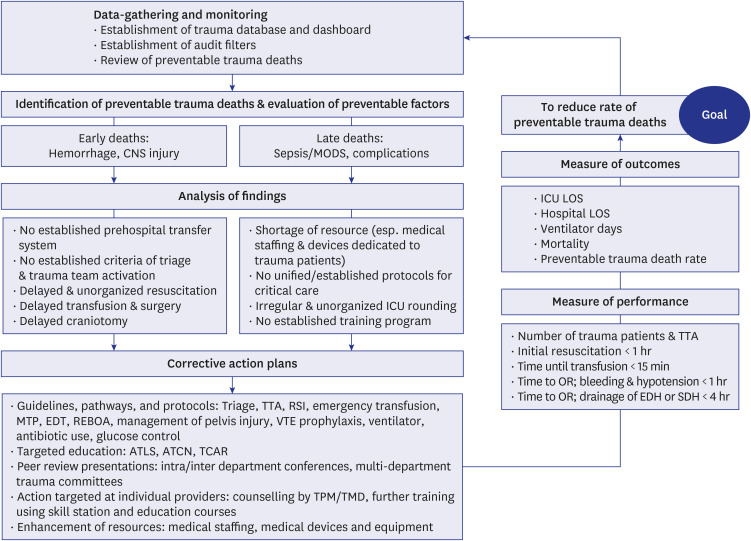
The PIPS program was based on guidelines by the World Health Organization and American College of Surgeons. The corrective strategies were proceeded according to the loop closure principle: data-gathering and monitoring, identification of preventable trauma deaths (PTDs), evaluation of preventable factors, analysis of findings, and corrective action plans. We established guidelines and protocols for trauma care, conducted targeted education and peer review presentations for problematic cases, and enhanced resources for improvement accordingly. A comparative analysis was performed on trauma outcomes over a four-year period (2015–2018) since implementing the PIPS program, including the number of trauma team activation and admissions, time factors related to resuscitation, ventilator duration, and the rate of PTDs.
Results
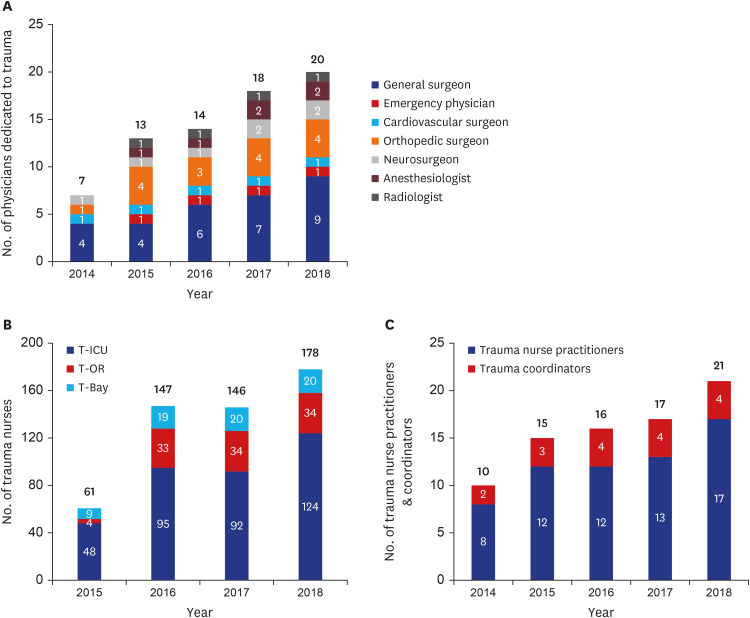
Human resources in the center significantly increased during the period; attending surgeons responsible for trauma resuscitation from 6 to 11 and trauma nurses from 85 to 218. Trauma admissions (from 2,166 to 2,786), trauma team activations (from 373 to 1,688), and severe cases (from 22.6 to 33.8%) significantly increased (all P < 0.001). Time to initial resuscitation and transfusion significantly decreased from 120 to 36 minutes (P < 0.001) and from 39 to 16 minutes (P < 0.001). Time to surgery for hemorrhage control and decompressive craniotomy improved from 99 to 54 minutes (P < 0.001) and 181 to 135 minutes (P = 0.042). Ventilator duration and rate of PTDs significantly decreased from 6 to 4 days (P = 0.001) and 22.2% to 8.4% (P = 0.008).
Conclusion
Implementation of the PIPS program resulted in improvements in outcomes at a regional trauma center that has just been opened in Korea. Further establishment of the PIPS program is required for optimal care of trauma patients.
Keyword
Figure
Cited by 1 articles
-
Effect of Quality Control Program in Surgical Management of Early Cervical Cancer
Ji Eun Shim, Mi-Kyung Kim, Yun Hwan Kim, Seung Cheol Kim
J Korean Med Sci. 2021;36(45):e316. doi: 10.3346/jkms.2021.36.e316.
Reference
-
1. Kim H, Jung KY, Kim SP, Kim SH, Noh H, Jang HY, et al. Changes in preventable death rates and traumatic care systems in Korea. J Korean Soc Emerg Med. 2012; 23(2):189–197.2. Yoon HD. Background and progress of regional trauma center development. J Korean Med Assoc. 2016; 59(12):919–922.
Article3. Yu B, Lee G, Lee MA, Choi K, Hyun S, Jeon Y, et al. Trauma volume and performance of a regional trauma center in Korea: initial 5-year analysis. J Trauma Inj. 2020; 33(1):31–37.
Article4. Chung S, Choi D, Cho J, Huh Y, Moon J, Kwon J, et al. Timing and associated factors for sepsis-3 in severe trauma patients: a 3-year single trauma center experience. Acute Crit Care. 2018; 33(3):130–134. PMID: 31723876.
Article5. Jung K, Kim I, Park SK, Cho H, Park CY, Yun JH, et al. Preventable trauma death rate after establishing a national trauma system in Korea. J Korean Med Sci. 2019; 34(8):e65. PMID: 30833882.
Article6. Korea JoongAng Daily. Hospitals refuse treatment ... A two-year-old boy with severe trauma from car accident died. Updated 2016. Accessed December 1, 2020. https://news.joins.com/article/20691893.7. Medipana. A patient with leg amputation died at a regional trauma center; ‘Controversy’ whether it can be a preventable trauma death. Updated 2020. Accessed December 1, 2020. http://m.medipana.com/news_viewer.asp?NewsNum=251013&vCount=12&vKind=1.8. World Health Organization. Guidelines for Trauma Quality Improvement Programmes. Geneva, Switzerland: WHO Press;2009.9. American College of Surgeons Committee on Trauma. Resources for Optimal Care of the Injured Patient. Chicago, IL, USA: American College of Surgeons;2014.10. McCoy CE, Chakravarthy B, Lotfipour S. Guidelines for field triage of injured patients: in conjunction with the morbidity and mortality weekly report published by the Center for Disease Control and Prevention. West J Emerg Med. 2013; 14(1):69–76. PMID: 23447758.11. Kang BH, Choi D, Cho J, Kwon J, Huh Y, Moon J, et al. Efficacy of uncross-matched type O packed red blood cell transfusion to traumatic shock patients: a propensity score matched study. J Korean Med Sci. 2017; 32(12):2058–2063. PMID: 29115091.12. Jung K, Matsumoto S, Smith A, Hwang K, Lee JC, Coimbra R. Analyses of clinical outcomes after severe pelvic fractures: an international study. Trauma Surg Acute Care Open. 2018; 3(1):e000238. PMID: 30539155.
Article13. Kang BH, Choi D, Huh Y, Kwon J, Jung K, Lee JC, et al. Sign of life is associated with return of spontaneous circulation after resuscitative thoracotomy: single trauma center experience of Republic of Korea. World J Surg. 2019; 43(6):1519–1524. PMID: 30737554.
Article14. Kim Y, Jung KY, Cho KH, Kim H, Ahn HC, Oh SH, et al. Preventable trauma deaths rates and management errors in emergency medical system in Korea. J Korean Soc Emerg Med. 2006; 17(5):385–394.15. Shafi S, Ahn C, Parks J, Nathens AB, Cryer HM, Gentilello LM, et al. Quality of care within a trauma center is not altered by injury type. J Trauma. 2010; 68(3):716–720. PMID: 20220425.
Article16. Davenport RA, Tai N, West A, Bouamra O, Aylwin C, Woodford M, et al. A major trauma centre is a specialty hospital not a hospital of specialties. Br J Surg. 2010; 97(1):109–117. PMID: 20013932.
Article17. DiRusso S, Holly C, Kamath R, Cuff S, Sullivan T, Scharf H, et al. Preparation and achievement of American College of Surgeons level I trauma verification raises hospital performance and improves patient outcome. J Trauma. 2001; 51(2):294–299. PMID: 11493787.
Article18. Na JY, Park JP, Park HJ, Lee BW, Choi YS, Seo JS. The statistical analysis on legal autopsy performed in Korea during 2012 year. Korean J Leg Med. 2013; 37(4):198–207.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Review of Quality Management and Improvement of Trauma Fee Schedule in Regional Trauma Center
- National evaluation program for emergency medical center
- Evaluation of the food safety training for food handlers in restaurant operations
- Organization and Roles of the Trauma Team
- An Importance-Performance Analysis of patient safety activities for inpatients in small and medium-sized hospitals