J Stroke.
2021 May;23(2):244-252. 10.5853/jos.2020.03622.
Prediction of Early Recanalization after Intravenous Thrombolysis in Patients with Large-Vessel Occlusion
- Affiliations
-
- 1Department of Neurology, Yonsei University College of Medicine, Seoul, Korea
- 2Department of Neurology, Brain Research Institute, Keimyung University School of Medicine, Daegu, Korea
- 3Department of Neurology, Yongin Severance Hospital, Yonsei University College of Medicine, Yongin, Korea
- 4Department of Radiology, Yonsei University College of Medicine, Seoul, Korea
- 5Department of Neurology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 6Department of Neurology, Gangnam Severance Hospital, Severance Institute for Vascular and Metabolic Research, Yonsei University College of Medicine, Seoul, Korea
- 7Department of Neurology, Changwon Fatima Hospital, Changwon, Korea
- 8Department of Research Affairs, Biostatistics Collaboration Unit, Yonsei University College of Medicine, Seoul, Korea
- 9Department of Neurology, Chosun University College of Medicine, Gwangju, Korea
- 10Department of Neurology, Gachon University Gil Medical Center, Incheon, Korea
- 11Department of Neurology, Kyung Hee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea
- 12Department of Neurology, Pusan National University School of Medicine, Busan, Korea
- 13Department of Neurology, National Medical Center, Seoul, Korea
- 14Department of Neurology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 15Department of Neurology, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 16Department of Neurology, Wonkwang University Sanbon Hospital, Wonkwang University School of Medicine, Sanbon, Korea
- 17Department of Neurology, Yonsei University Wonju College of Medicine, Wonju, Korea
- 18Department of Neurology, Ewha Womans University Mokdong Hospital, Ewha Womans University School of Medicine, Seoul, Korea
- 19Department of Neurology, Ewha Womans University Seoul Hospital, Ewha Womans University School of Medicine, Seoul, Korea
- 20Department of Neurology, CHA Bundang Medical Center, CHA University, Seongnam, Korea
- 21Department of Neurology, Inje University Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea
- KMID: 2516413
- DOI: http://doi.org/10.5853/jos.2020.03622
Abstract
- Background and Purpose
We aimed to develop a model predicting early recanalization after intravenous tissue plasminogen activator (t-PA) treatment in large-vessel occlusion.
Methods
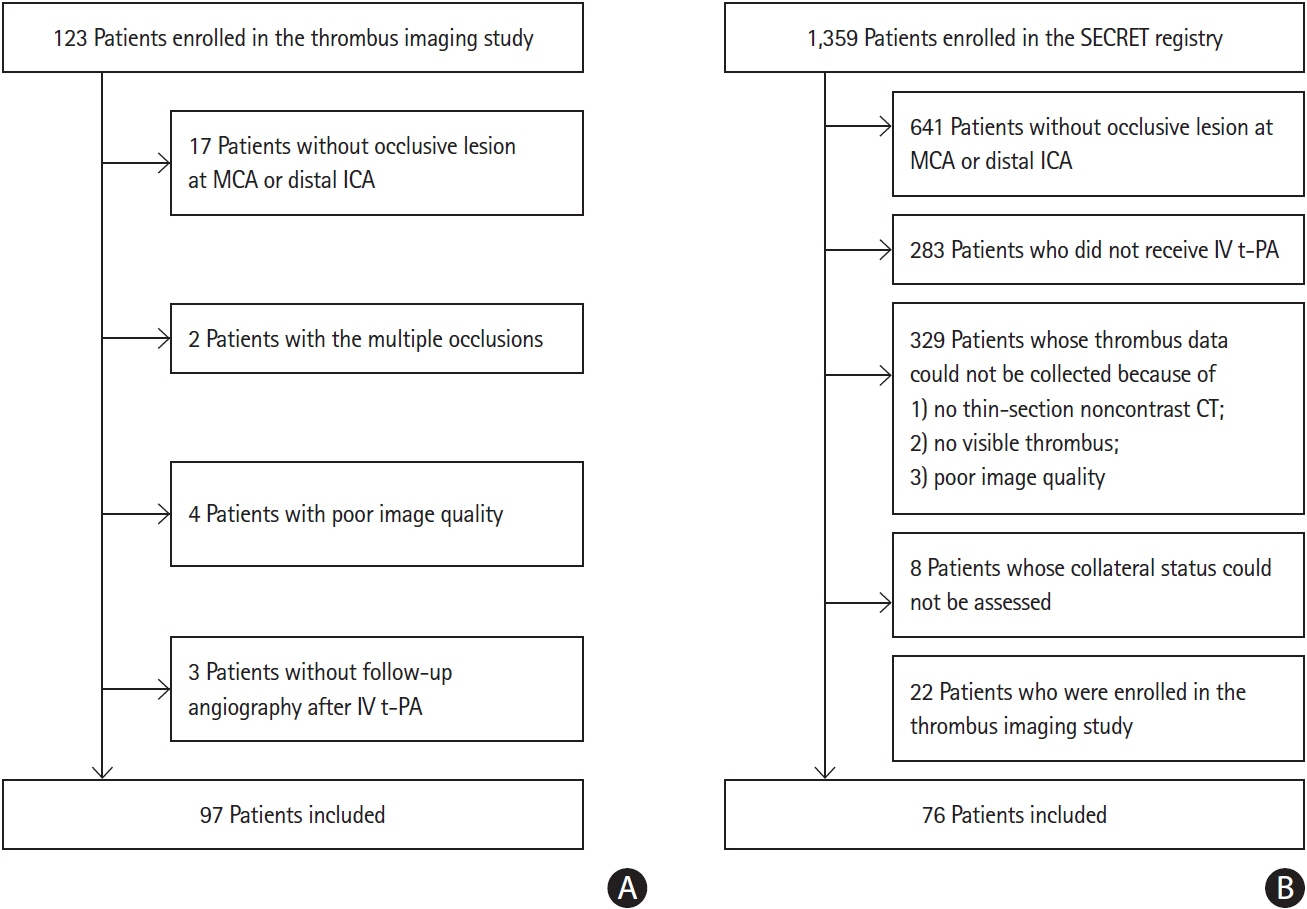
Using data from two different multicenter prospective cohorts, we determined the factors associated with early recanalization immediately after t-PA in stroke patients with large-vessel occlusion, and developed and validated a prediction model for early recanalization. Clot volume was semiautomatically measured on thin-section computed tomography using software, and the degree of collaterals was determined using the Tan score. Follow-up angiographic studies were performed immediately after t-PA treatment to assess early recanalization.
Results
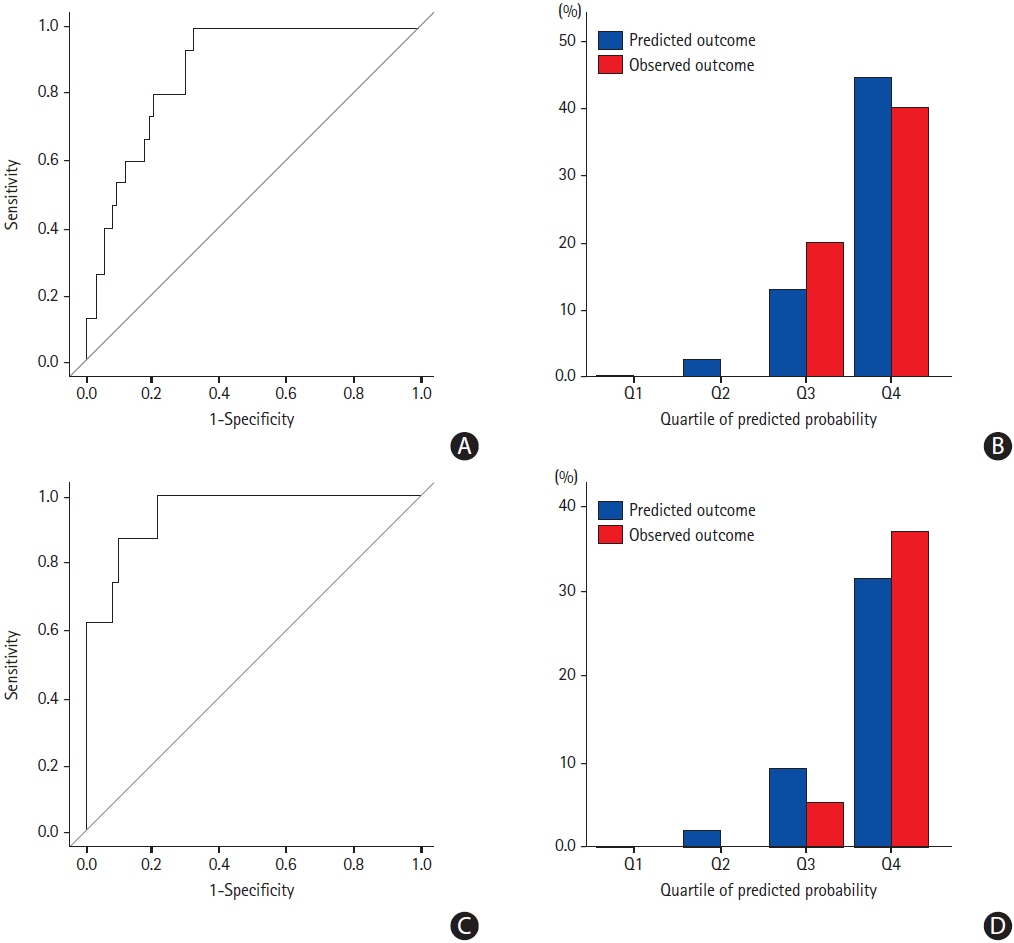
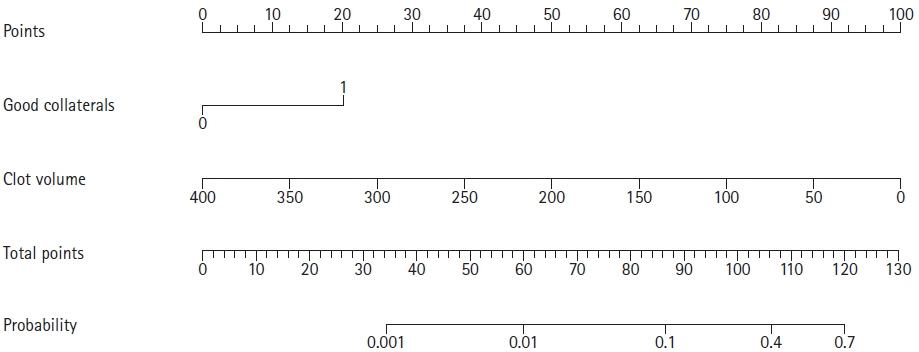
Early recanalization, assessed 61.0±44.7 minutes after t-PA bolus, was achieved in 15.5% (15/97) in the derivation cohort and in 10.5% (8/76) in the validation cohort. Clot volume (odds ratio [OR], 0.979; 95% confidence interval [CI], 0.961 to 0.997; P=0.020) and good collaterals (OR, 6.129; 95% CI, 1.592 to 23.594; P=0.008) were significant factors associated with early recanalization. The area under the curve (AUC) of the model including clot volume was 0.819 (95% CI, 0.720 to 0.917) and 0.842 (95% CI, 0.746 to 0.938) in the derivation and validation cohorts, respectively. The AUC improved when good collaterals were added (derivation cohort: AUC, 0.876; 95% CI, 0.802 to 0.950; P=0.164; validation cohort: AUC, 0.949; 95% CI, 0.886 to 1.000; P=0.036). The integrated discrimination improvement also showed significantly improved prediction (0.097; 95% CI, 0.009 to 0.185; P=0.032).
Conclusions
The model using clot volume and collaterals predicted early recanalization after intravenous t-PA and had a high performance. This model may aid in determining the recanalization treatment strategy in stroke patients with large-vessel occlusion.
Keyword
Figure
Reference
-
References
1. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016; 387:1723–1731.
Article2. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke. A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; 50:e344–e418.
Article3. Lee KY, Han SW, Kim SH, Nam HS, Ahn SW, Kim DJ, et al. Early recanalization after intravenous administration of recombinant tissue plasminogen activator as assessed by preand post-thrombolytic angiography in acute ischemic stroke patients. Stroke. 2007; 38:192–193.4. Campbell BCV, Mitchell PJ, Churilov L, Yassi N, Kleinig TJ, Dowling RJ, et al. Tenecteplase versus alteplase before thrombectomy for ischemic stroke. N Engl J Med. 2018; 378:1573–1582.5. Yoo J, Baek JH, Park H, Song D, Kim K, Hwang IG, et al. Thrombus volume as a predictor of nonrecanalization after intravenous thrombolysis in acute stroke. Stroke. 2018; 49:2108–2115.
Article6. Fischer U, Kaesmacher J, Mendes Pereira V, Chapot R, Siddiqui AH, Froehler MT, et al. Direct mechanical thrombectomy versus combined intravenous and mechanical thrombectomy in large-artery anterior circulation stroke: a topical review. Stroke. 2017; 48:2912–2918.7. Tsivgoulis G, Saqqur M, Sharma VK, Brunser A, Eggers J, Mikulik R, et al. Timing of recanalization and functional recovery in acute ischemic stroke. J Stroke. 2020; 22:130–140.
Article8. Albers GW. Thrombolysis before thrombectomy: to be or DIRECT- MT? N Engl J Med. 2020; 382:2045–2046.9. Zhu G, Michel P, Jovin T, Patrie JT, Xin W, Eskandari A, et al. Prediction of recanalization in acute stroke patients receiving intravenous and endovascular revascularization therapy. Int J Stroke. 2015; 10:28–36.
Article10. Rohan V, Baxa J, Tupy R, Cerna L, Sevcik P, Friesl M, et al. Length of occlusion predicts recanalization and outcome after intravenous thrombolysis in middle cerebral artery stroke. Stroke. 2014; 45:2010–2017.
Article11. Tan IY, Demchuk AM, Hopyan J, Zhang L, Gladstone D, Wong K, et al. CT angiography clot burden score and collateral score: correlation with clinical and radiologic outcomes in acute middle cerebral artery infarct. AJNR Am J Neuroradiol. 2009; 30:525–531.
Article12. Heo JH, Kim K, Yoo J, Kim YD, Nam HS, Kim EY. Computed tomography-based thrombus imaging for the prediction of recanalization after reperfusion therapy in stroke. J Stroke. 2017; 19:40–49.
Article13. Behrens L, Möhlenbruch M, Stampfl S, Ringleb PA, Hametner C, Kellert L, et al. Effect of thrombus size on recanalization by bridging intravenous thrombolysis. Eur J Neurol. 2014; 21:1406–1410.
Article14. Seners P, Roca P, Legrand L, Turc G, Cottier JP, Cho TH, et al. Better collaterals are independently associated with post-thrombolysis recanalization before thrombectomy. Stroke. 2019; 50:867–872.
Article15. Derraz I, Bourcier R, Soudant M, Soize S, Hassen WB, Hossu G, et al. Does clot burden score on baseline T2*-MRI impact clinical outcome in acute ischemic stroke treated with mechanical thrombectomy? J Stroke. 2019; 21:91–100.
Article16. Bang OY, Goyal M, Liebeskind DS. Collateral circulation in ischemic stroke: assessment tools and therapeutic strategies. Stroke. 2015; 46:3302–3309.17. Kim YD, Heo JH, Yoo J, Park H, Kim BM, Bang OY, et al. Improving the clinical outcome in stroke patients receiving thrombolytic or endovascular treatment in Korea: from the SECRET Study. J Clin Med. 2020; 9:717.
Article18. Kim EY, Lee SK, Kim DJ, Suh SH, Kim J, Heo JH, et al. Detection of thrombus in acute ischemic stroke: value of thin-section noncontrast-computed tomography. Stroke. 2005; 36:2745–2747.19. Kim YD, Nam HS, Kim SH, Kim EY, Song D, Kwon I, et al. Time-dependent thrombus resolution after tissue-type plasminogen activator in patients with stroke and mice. Stroke. 2015; 46:1877–1882.
Article20. Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, et al. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke. 2003; 34:e109–e137.
Article21. Seners P, Caroff J, Chausson N, Turc G, Denier C, Piotin M, et al. Recanalization before thrombectomy in tenecteplase vs. alteplase-treated drip-and-ship patients. J Stroke. 2019; 21:105–107.
Article22. Yang P, Zhang Y, Zhang L, Zhang Y, Treurniet KM, Chen W, et al. Endovascular thrombectomy with or without intravenous alteplase in acute stroke. N Engl J Med. 2020; 382:1981–1993.
Article23. Katsanos AH, Malhotra K, Goyal N, Arthur A, Schellinger PD, Köhrmann M, et al. Intravenous thrombolysis prior to mechanical thrombectomy in large vessel occlusions. Ann Neurol. 2019; 86:395–406.
Article24. Suzuki K, Kimura K, Takeuchi M, Morimoto M, Kanazawa R, Kamiya Y, et al. The randomized study of endovascular therapy with versus without intravenous tissue plasminogen activator in acute stroke with ICA and M1 occlusion (SKIP study). Int J Stroke. 2019; 14:752–755.
Article25. Zhang S, Zhang X, Yan S, Lai Y, Han Q, Sun J, et al. The velocity of collateral filling predicts recanalization in acute ischemic stroke after intravenous thrombolysis. Sci Rep. 2016; 6:27880.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Previous and Recent Evidence of Endovascular Therapy in Acute Ischemic Stroke
- Recanalization Rate and its Associated Factors after Intravenous Tissue Plasminogen Activator Thrombolysis for Acute Major Cerebral Arterial Occlusion
- Intravenous Thrombolysis and Endovascular Thrombectomy in Acute Ischemic Stroke with Minor Symptom
- Recanalization Rate and Clinical Outcomes of Intravenous Tissue Plasminogen Activator Administration for Large Vessel Occlusion Stroke Patients
- Evolution of Endovascular Therapy in Acute Stroke: Implications of Device Development