Ann Hepatobiliary Pancreat Surg.
2021 May;25(2):287-292. 10.14701/ahbps.2021.25.2.287.
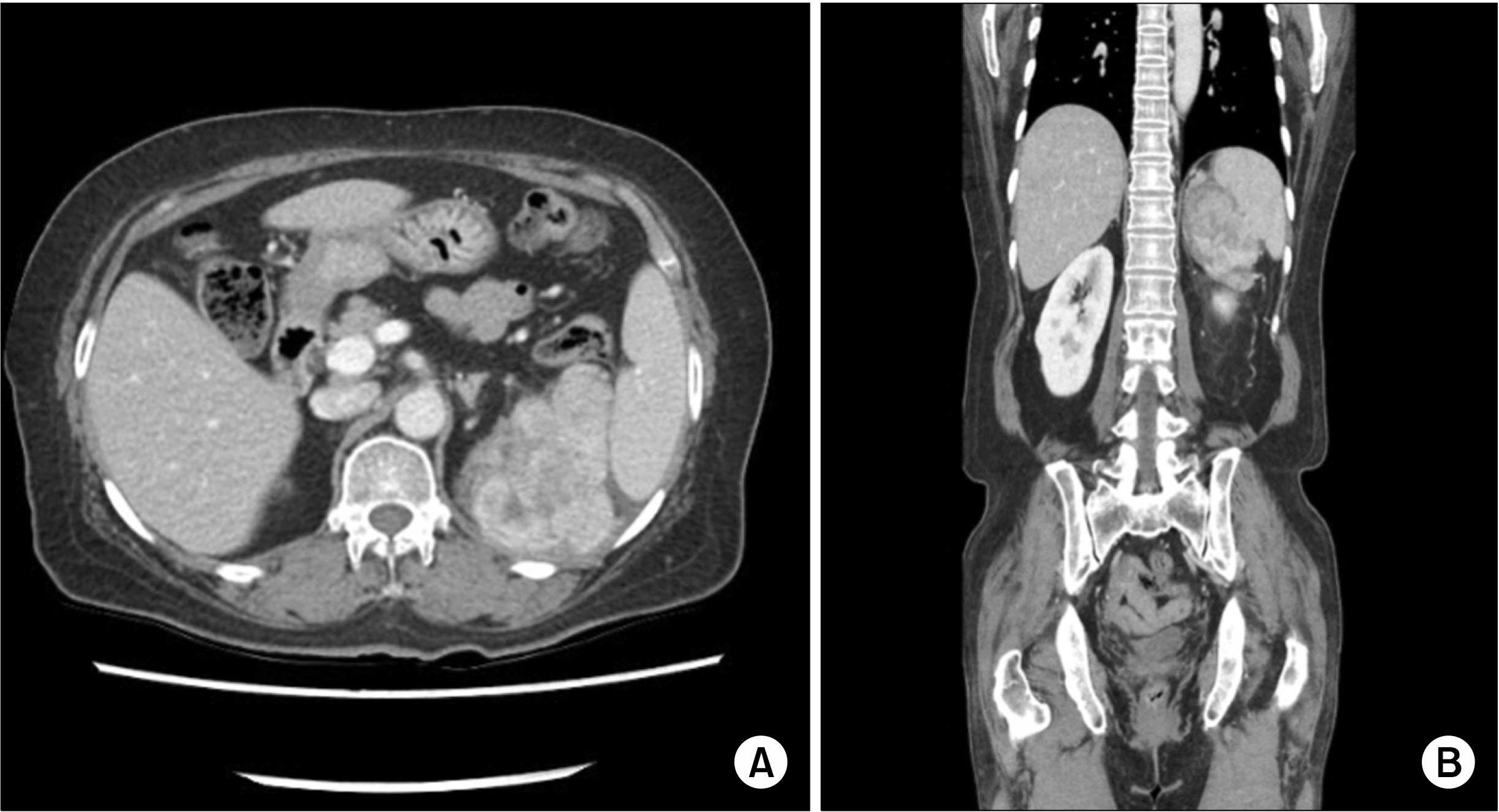
Inflammatory myofibroblastic tumors arising from pancreas head and peri-splenic area mimicking a malignancy
- Affiliations
-
- 1Departments of Surgery, Dong-A University Hospital, Dong-A University College of Medicine, Busan, Korea
- 2Departments of Pathology, Dong-A University Hospital, Dong-A University College of Medicine, Busan, Korea
- KMID: 2516331
- DOI: http://doi.org/10.14701/ahbps.2021.25.2.287
Abstract
- Inflammatory myofibroblastic tumors (IMTs) are a rare chronic inflammatory disease with unclear pathogenesis and pathological features that are not those of a malignant tumor. It is difficult to differentially diagnose them without surgical excision because of their unpredictable clinical behavior, which ranges from benign to locally invasive aggressiveness. We report two cases of IMTs that were diagnosed after surgery. In one case, the IMT originated in peri-splenic area in a 63-year-old female patient. The other case involved a 48-year-old female patient who suffered from an IMT of the head of the pancreas. Both of these cases did not require further treatment based on histological findings, and there has been no evidence of recurrence or metastasis so far. These cases show that the primary choice for the exact diagnosis and proper treatment of IMTs is complete surgical resection.
Figure
Reference
-
1. Kovach SJ, Fischer AC, Katzman PJ, Salloum RM, Ettinghausen SE, Madeb R, et al. 2006; Inflammatory myofibroblastic tumors. J Surg Oncol. 94:385–391. DOI: 10.1002/jso.20516. PMID: 16967468.
Article2. Thompson LDR. 2019; Inflammatory myofibroblastic tumor. Ear Nose Throat J. doi: 10.1177/0145561319890165. [in press]. DOI: 10.1177/0145561319890165. PMID: 31760795.
Article3. Ding D, Bu X, Tian F. 2016; Inflammatory myofibroblastic tumor in the head of the pancreas with anorexia and vomiting in a 69-year-old man: a case report. Oncol Lett. 12:1546–1550. DOI: 10.3892/ol.2016.4787. PMID: 27446468. PMCID: PMC4950493.
Article4. Battal M, Kartal K, Tuncel D, Bostanci O. 2016; Inflammatory myofibroblastic pancreas tumor: a case report. Clin Case Rep. 4:1122–1124. DOI: 10.1002/ccr3.717. PMID: 27980746. PMCID: PMC5134138.
Article5. Tao YL, Wang ZJ, Han JG, Wei P. 2012; Inflammatory myofibroblastic tumor successfully treated with chemotherapy and nonsteroidals: a case report. World J Gastroenterol. 18:7100–7103. DOI: 10.3748/wjg.v18.i47.7100. PMID: 23323014. PMCID: PMC3531700.
Article6. Poves I, Alonso S, Jimeno M, Bessa X, Burdío F, Grande L. 2012; Retroperitoneal inflammatory pseudotumor presenting as a pancreatic mass. JOP. 13:308–311.7. Zanchi C, Giurici N, Martelossi S, Cheli M, Sonzogni A, Alberti D. 2015; Myofibroblastic tumor of the pancreatic head: recurrent cholangitis. J Pediatr Gastroenterol Nutr. 61:e28–e29. DOI: 10.1097/MPG.0000000000000350. PMID: 24590212.8. Panda D, Mukhopadhyay D, Datta C, Chattopadhyay BK, Chatterjee U, Shinde R. 2015; Inflammatory myofibroblastic tumor arising in the pancreatic head: a rare case report. Indian J Surg. 77:538–540. DOI: 10.1007/s12262-015-1322-8. PMID: 26884665. PMCID: PMC4744211.
Article9. Sim A, Lee MW, Nguyen GK. 2008; Inflammatory myofibroblastic tumour of the pancreas. Can J Surg. 51:E23–E24.10. Matsubayashi H, Uesaka K, Sasaki K, Shimada S, Takada K, Ishiwatari H, et al. 2019; A pancreatic inflammatory myofibroblastic tumor with spontaneous remission: a case report with a literature review. Diagnostics (Basel). 9:150. DOI: 10.3390/diagnostics9040150. PMID: 31627359. PMCID: PMC6963339.
Article11. Yamaguchi J, Sakamoto Y, Sano T, Shimada K, Kosuge T. 2007; Spontaneous regression of inflammatory pseudotumor of the liver: report of three cases. Surg Today. 37:525–529. DOI: 10.1007/s00595-006-3433-0. PMID: 17522777.
Article12. Zhao JJ, Ling JQ, Fang Y, Gao XD, Shu P, Shen KT, et al. 2014; Intra-abdominal inflammatory myofibroblastic tumor: spontaneous regression. World J Gastroenterol. 20:13625–13631. DOI: 10.3748/wjg.v20.i37.13625. PMID: 25309095. PMCID: PMC4188916.
Article13. Coffin CM, Hornick JL, Fletcher CD. 2007; Inflammatory myofibroblastic tumor: comparison of clinicopathologic, histologic, and immunohistochemical features including ALK expression in atypical and aggressive cases. Am J Surg Pathol. 31:509–520. DOI: 10.1097/01.pas.0000213393.57322.c7. PMID: 17414097.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Inflammatory Myofibroblastic Tumor of the Pancreas: A Case Report and Literature Review
- Inflammatory Myofibroblastic Tumor of Nasal Septum after Septoplasty: A Case Report
- Inflammatory Myofibroblastic Tumor of the Nasal Cavity
- Inflammatory Myofibroblastic Tumor of the Vocal Cord Mimicking Vocal Polyp
- An Inflammatory Myofibroblastic Tumor of the Ampulla of Vater Successfully Managed with Endoscopic Papillectomy: Report of a Case