Clin Endosc.
2021 May;54(3):379-389. 10.5946/ce.2020.276.
Underwater Endoscopic Mucosal Resection for 10 mm or Larger Nonpedunculated Colorectal Polyps: A Systematic Review and Meta-Analysis
- Affiliations
-
- 1Department of Internal Medicine, Cleveland Clinic, Cleveland, OH, USA
- 2Department of Gastroenterology, Hepatology and Nutrition, Digestive Diseases and Surgery Institute, Cleveland Clinic, Cleveland, OH, USA
- 3Department of Gastroenterology, University of Utah, Salt Lake City, UT, USA
- 4Department of Gastroenterology and Hepatology, University of New Mexico, Albuquerque, NM, USA
- KMID: 2516318
- DOI: http://doi.org/10.5946/ce.2020.276
Abstract
- Background/Aims
Recent studies have reported the favorable outcomes of underwater endoscopic mucosal resection (UEMR) for colorectal polyps. We performed a systematic review and meta-analysis evaluating the efficacy and safety of UEMR for nonpedunculated polyps ≥10 mm.
Methods
We performed a comprehensive search of multiple databases (through May 2020) to identify studies reporting the outcomes of UEMR for ≥10 mm nonpedunculated colorectal polyps. The assessed outcomes were recurrence rate on the first follow-up, en bloc resection, incomplete resection, and adverse events after UEMR.
Results
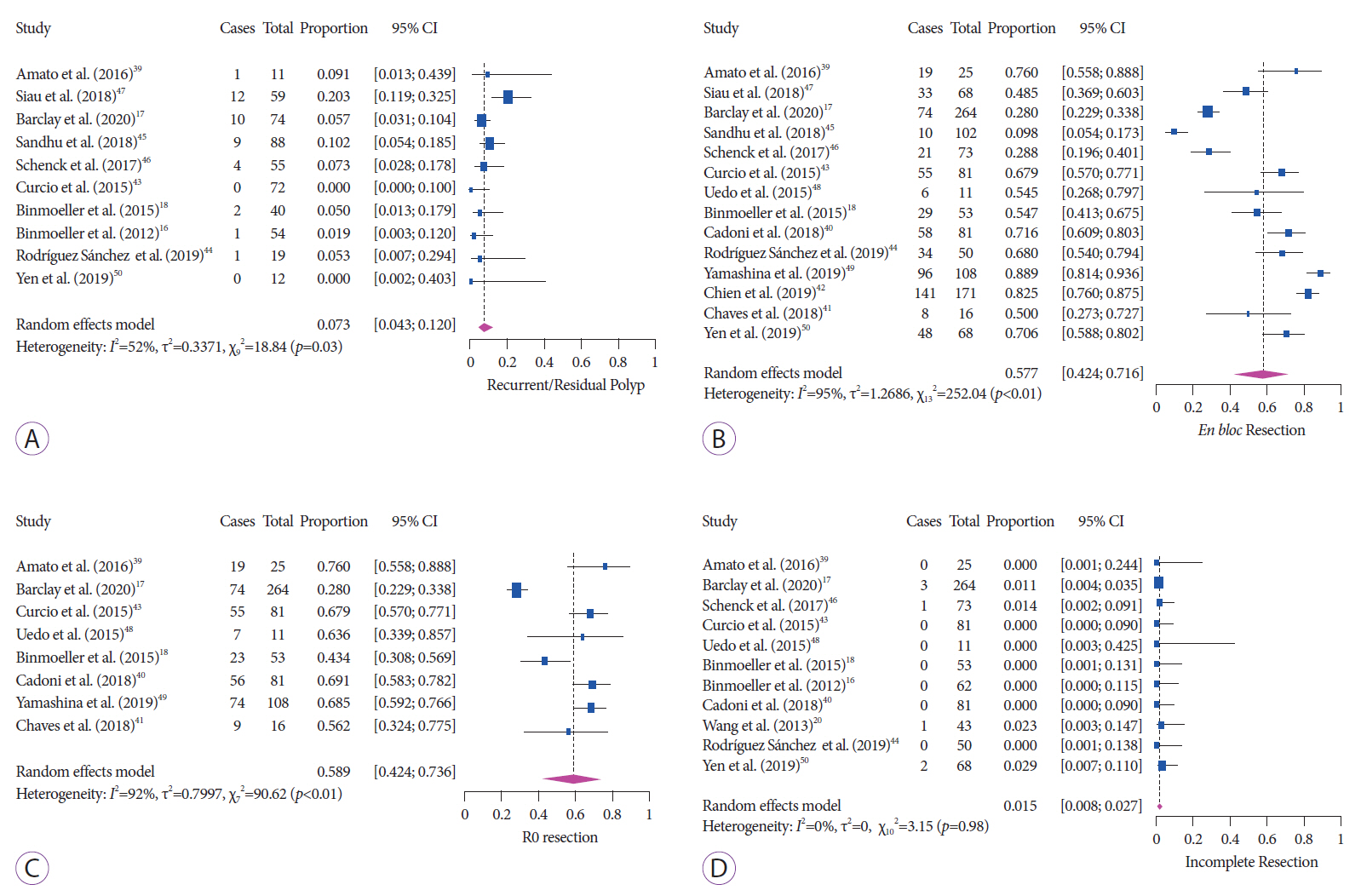
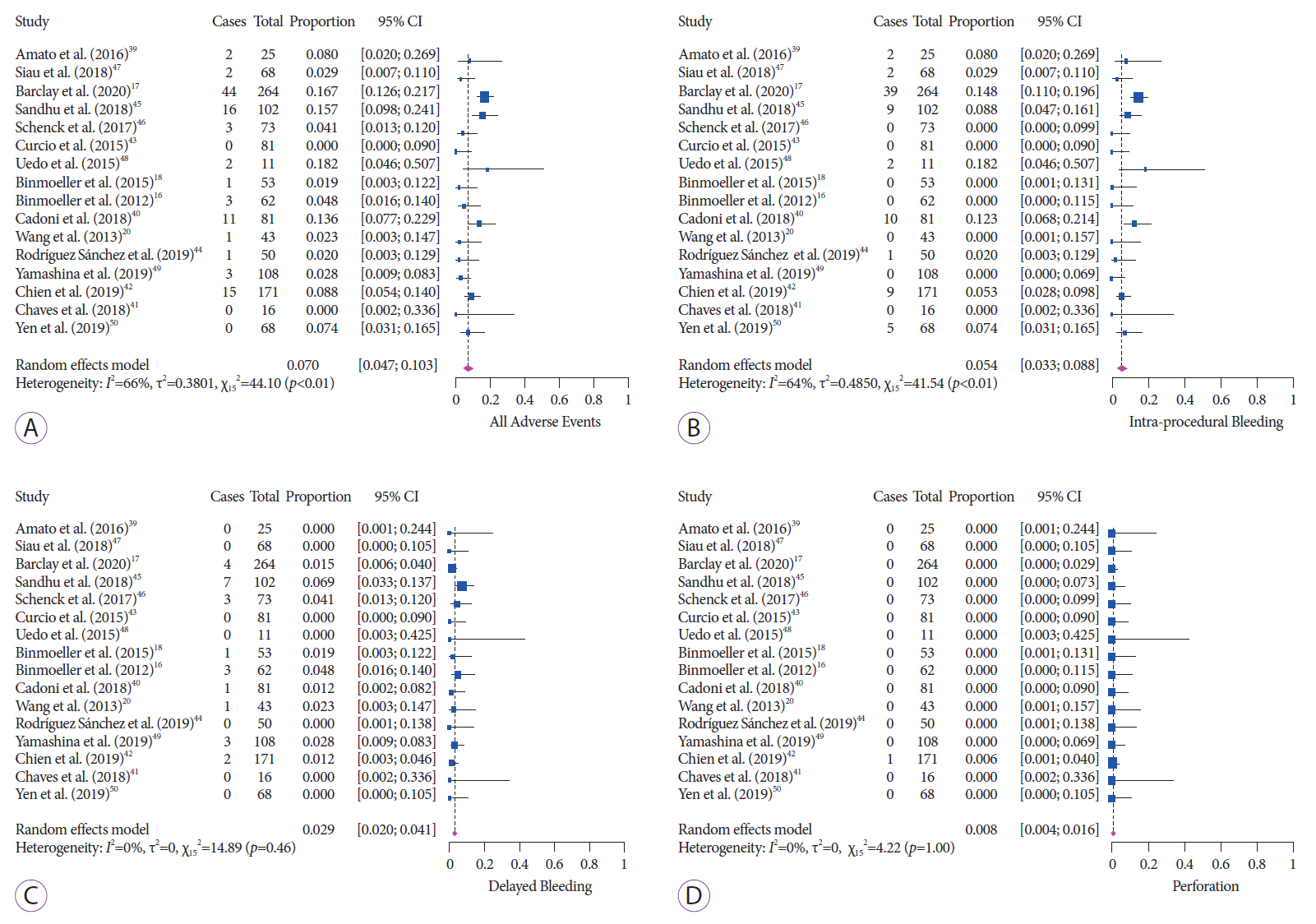
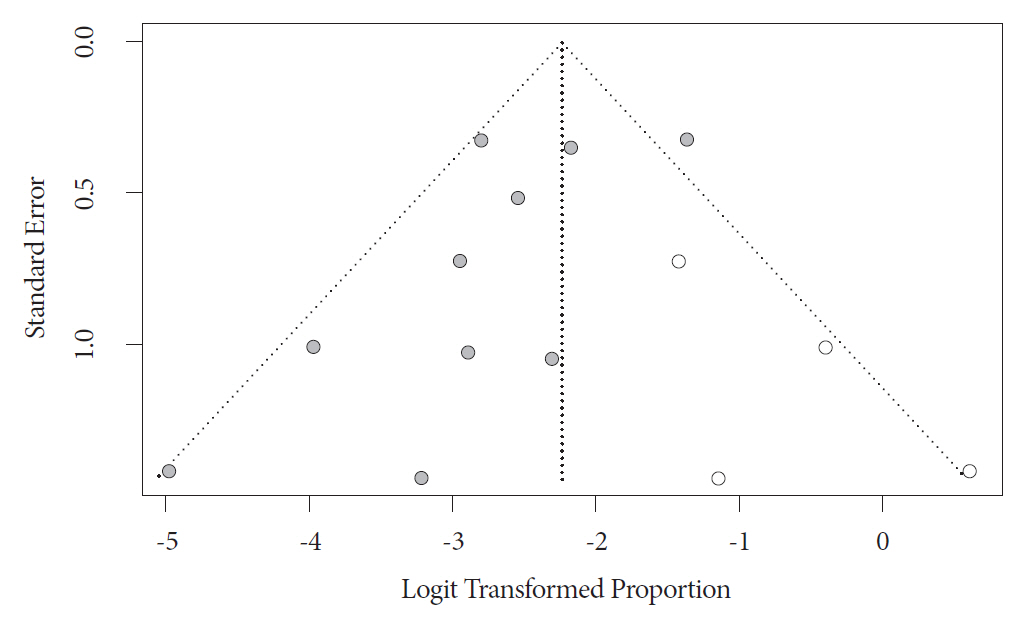
A total of 1276 polyps from 16 articles were included in our study. The recurrence rate was 7.3% (95% confidence interval [CI], 4.3–12) and 5.9% (95% CI, 3.6–9.4) for nonpedunculated polyps ≥10 and ≥20 mm, respectively. For nonpedunculated polyps ≥10 mm, the en bloc resection, R0 resection, and incomplete resection rates were 57.7% (95% CI, 42.4–71.6), 58.9% (95% CI, 42.4–73.6), and 1.5% (95% CI, 0.8–2.6), respectively. The rates of pooled adverse events, intraprocedural bleeding, and delayed bleeding were 7.0%, 5.4%, and 2.9%, respectively. The rate of perforation and postpolypectomy syndrome was 0.8%.
Conclusions
Our systematic review and meta-analysis demonstrates that UEMR for nonpedunculated colorectal polyps ≥10 mm is safe and effective with a low rate of recurrence.
Keyword
Figure
Reference
-
1. National Cancer Institute. Cancer stat facts: colorectal cancer [Internet]. Rockville (MD): SEER;c2021. [cited 2021 Mar 31]. Available from: https://seer.cancer.gov/statfacts/html/colorect.html.2. Gaglia A, Sarkar S. Evaluation and long-term outcomes of the different modalities used in colonic endoscopic mucosal resection. Ann Gastroenterol. 2017; 30:145–151.
Article3. Holt BA, Bourke MJ. Wide field endoscopic resection for advanced colonic mucosal neoplasia: current status and future directions. Clin Gastroenterol Hepatol. 2012; 10:969–979.
Article4. Bourke MJ. Endoscopic resection for mucosal neoplasia: pushing the boundaries, confronting the reality. J Gastroenterol Hepatol. 2011; 26:1582–1584.
Article5. Ferlitsch M, Moss A, Hassan C, et al. Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2017; 49:270–297.
Article6. Kaltenbach T, Anderson JC, Burke CA, et al. Endoscopic removal of colorectal lesions-recommendations by the US multi-society task force on colorectal cancer. Gastroenterology. 2020; 158:1095–1129.
Article7. Binmoeller KF, Bohnacker S, Seifert H, Thonke F, Valdeyar H, Soehendra N. Endoscopic snare excision of “giant” colorectal polyps. Gastrointest Endosc. 1996; 43:183–188.
Article8. Iishi H, Tatsuta M, Iseki K, et al. Endoscopic piecemeal resection with submucosal saline injection of large sessile colorectal polyps. Gastrointest Endosc. 2000; 51:697–700.
Article9. Swan MP, Bourke MJ, Moss A, Williams SJ, Hopper A, Metz A. The target sign: an endoscopic marker for the resection of the muscularis propria and potential perforation during colonic endoscopic mucosal resection. Gastrointest Endosc. 2011; 73:79–85.
Article10. Knabe M, Pohl J, Gerges C, Ell C, Neuhaus H, Schumacher B. Standardized long-term follow-up after endoscopic resection of large, nonpedunculated colorectal lesions: a prospective two-center study. Am J Gastroenterol. 2014; 109:183–189.
Article11. Swan MP, Bourke MJ, Alexander S, Moss A, Williams SJ. Large refractory colonic polyps: is it time to change our practice? a prospective study of the clinical and economic impact of a tertiary referral colonic mucosal resection and polypectomy service (with videos). Gastrointest Endosc. 2009; 70:1128–1136.
Article12. Jayanna M, Burgess NG, Singh R, et al. Cost analysis of endoscopic mucosal resection vs surgery for large laterally spreading colorectal lesions. Clin Gastroenterol Hepatol. 2016; 14:271–278.e1-e2.13. Fukami N, Lee JH. Endoscopic treatment of large sessile and flat colorectal lesions. Curr Opin Gastroenterol. 2006; 22:54–59.
Article14. Moss A, Williams SJ, Hourigan LF, et al. Long-term adenoma recurrence following wide-field endoscopic mucosal resection (WF-EMR) for advanced colonic mucosal neoplasia is infrequent: results and risk factors in 1000 cases from the Australian Colonic EMR (ACE) study. Gut. 2015; 64:57–65.
Article15. Tanaka S, Kashida H, Saito Y, et al. JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc. 2015; 27:417–434.
Article16. Binmoeller KF, Weilert F, Shah J, Bhat Y, Kane S. “Underwater” EMR without submucosal injection for large sessile colorectal polyps (with video). Gastrointest Endosc. 2012; 75:1086–1091.
Article17. Barclay RL, Percy DB. Underwater endoscopic mucosal resection without submucosal injection (UEMR) for large colorectal polyps: a community-based series. Am J Surg. 2020; 220:693–696.
Article18. Binmoeller KF, Hamerski CM, Shah JN, Bhat YM, Kane SD. Garcia-Kennedy R Attempted underwater en bloc resection for large (2-4 cm) colorectal laterally spreading tumors (with video). Gastrointest Endosc. 2015; 81:713–718.19. Nett A, Binmoeller K. Underwater Endoscopic Mucosal Resection. Gastrointest Endosc Clin N Am. 2019; 29:659–673.
Article20. Wang AY, Flynn MM, Patrie JT, et al. Underwater endoscopic mucosal resection of colorectal neoplasia is easily learned, efficacious, and safe. Surg Endosc. 2014; 28:1348–1354.
Article21. Spadaccini M, Fuccio L, Lamonaca L, et al. Underwater EMR for colorectal lesions: a systematic review with meta-analysis (with video). Gastrointest Endosc. 2019; 89:1109–1116.e4.
Article22. Li DF, Lai MG, Yang MF, et al. The efficacy and safety of underwater endoscopic mucosal resection for ≥10-mm colorectal polyps: systematic review and meta-analysis. Endoscopy. 2020; Aug. 6. [Epub]. https://doi.org/10.1055/a-1234-8918.
Article23. Li P, Ma B, Gong S, Zhang X, Li W. Underwater endoscopic mucosal resection for colorectal lesions: a meta-analysis. Surg Endosc. 2020; Jun. 23. [Epub]. https://doi.org/10.1007/s00464-020-07745-8.
Article24. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann Intern Med. 2009; 151:264–269.W64.
Article25. Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000; 283:2008–2012.26. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010; 25:603–605.
Article27. Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996; 17:1–12.
Article28. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986; 7:177–188.
Article29. Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F. Methods for meta-analysis in medical research. Hoboken (NJ): John Wiley & Sons;2000. p. 205–228.30. Higgins JPT, Thompson SG, Spiegelhalter DJ. A re-evaluation of random-effects meta-analysis. J R Stat Soc Ser A Stat Soc. 2009; 172:137–159.
Article31. Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. 2011; 342:d549.
Article32. Mohan BP, Adler DG. Heterogeneity in systematic review and meta-analysis: how to read between the numbers. Gastrointest Endosc. 2019; 89:902–903.
Article33. Kanwal F, White D. “Systematic Reviews and Meta-analyses” in Clinical Gastroenterology and Hepatology. Clin Gastroenterol Hepatol. 2012; 10:1184–1186.
Article34. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327:557–560.
Article35. Guyatt GH, , Oxman AD, Kunz R, et al. GRADE guidelines: 7. Rating the quality of evidence--inconsistency. J Clin Epidemiol. 2011; 64:1294–1302.
Article36. Easterbrook PJ, Berlin JA, Gopalan R, Matthews DR. Publication bias in clinical research. Lancet. 1991; 337:867–872.
Article37. Duval S, Tweedie R. Trim and fill: a simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000; 56:455–463.
Article38. Rothstein HR, Sutton AJ, Borenstein M. Publication bias in meta-analysis: Prevention, assessment and adjustments. Hoboken (NJ): John Wiley & Sons;2006.39. Amato A, Radaelli F, Spinzi G. Underwater endoscopic mucosal resection: The third way for en bloc resection of colonic lesions? United European Gastroenterol J. 2016; 4:595–598.
Article40. Cadoni S, Liggi M, Gallittu P, et al. Underwater endoscopic colorectal polyp resection: feasibility in everyday clinical practice. United European Gastroenterol J. 2018; 6:454–462.
Article41. Chaves DM, Brito HP, Chaves LT, Rodrigues RA, Sugai BM. Underwater endoscopic mucosal resection of serrated adenomas. Clinics (Sao Paulo). 2018; 73:e339.
Article42. Chien H-C, Uedo N, Hsieh P-H. Comparison of underwater and conventional endoscopic mucosal resection for removing sessile colorectal polyps: a propensity-score matched cohort study. Endosc Int Open. 2019; 07:E1528–E1536.
Article43. Curcio G, Granata A, Ligresti D, et al. Underwater colorectal EMR: remodeling endoscopic mucosal resection. Gastrointest Endosc. 2015; 81:1238–1242.
Article44. Rodriguez Sanchez J, Uchima Koecklin H, Gonzalez Lopez L, et al. Short and long-term outcomes of underwater EMR compared to the traditional procedure in the real clinical practice. Rev Esp Enferm Dig. 2019; 111:543–549.
Article45. Sandhu DS, Lee YJ, Gerke H. Underwater endoscopic mucosal resection: an alternative treatment for large colorectal polyp removal. Minerva Gastroenterol Dietol. 2018; 64:106–110.
Article46. Schenck RJ, Jahann DA, Patrie JT, et al. Underwater endoscopic mucosal resection is associated with fewer recurrences and earlier curative resections compared to conventional endoscopic mucosal resection for large colorectal polyps. Surg Endosc. 2017; 31:4174–4183.
Article47. Siau K, Ishaq S, Cadoni S, Kuwai T, Yusuf A, Suzuki N. Feasibility and outcomes of underwater endoscopic mucosal resection for ≥10 mm colorectal polyps. Surg Endosc. 2018; 32:2656–2663.48. Uedo N, Nemeth A, Johansson GW, Toth E, Thorlacius H. Underwater endoscopic mucosal resection of large colorectal lesions. Endoscopy. 2015; 47:172–174.
Article49. Yamashina T, Uedo N, Akasaka T, et al. Comparison of underwater vs conventional endoscopic mucosal resection of intermediate-size colorectal polyps. Gastroenterology. 2019; 157:451–461.e2.
Article50. Yen AW, Leung JW, Wilson MD, Leung FW. Underwater versus conventional endoscopic resection of nondiminutive nonpedunculated colorectal lesions: a prospective randomized controlled trial (with video). Gastrointest Endosc. 2020; 91:643–654.e2.
Article51. Kim HG, Thosani N, Banerjee S, Chen A, Friedland S. Underwater endoscopic mucosal resection for recurrences after previous piecemeal resection of colorectal polyps (with video). Gastrointest Endosc. 2014; 80:1094–1102.52. Binmoeller KF, Hamerski CM, Shah JN, Bhat YM, Kane SD. Underwater EMR of adenomas of the appendiceal orifice (with video). Gastrointest Endosc. 2016; 83:638–642.53. Kawamura T, Sakai H, Ogawa T, et al. Feasibility of underwater endoscopic mucosal resection for colorectal lesions: a single center study in Japan. Gastroenterology Res. 2018; 11:274–279.
Article54. Fujiya M, Tanaka K, Dokoshi T, et al. Efficacy and adverse events of EMR and endoscopic submucosal dissection for the treatment of colon neoplasms: a meta-analysis of studies comparing EMR and endoscopic submucosal dissection. Gastrointest Endosc. 2015; 81:583–595.
Article55. Hassan C, Repici A, Sharma P, et al. Efficacy and safety of endoscopic resection of large colorectal polyps: a systematic review and meta-analysis. Gut. 2016; 65:806–820.
Article56. Belderbos TDG, Leenders M, Moons LMG, Siersema PD. Local recurrence after endoscopic mucosal resection of nonpedunculated colorectal lesions: systematic review and meta-analysis. Endoscopy. 2014; 46:388–402.
Article57. Kandel P, Wallace MB. Colorectal endoscopic mucosal resection (EMR). Best Pract Res Clin Gastroenterol. 2017; 31:455–471.
Article58. Klein A, Tate DJ, Jayasekeran V, et al. Thermal ablation of mucosal defect margins reduces adenoma recurrence after colonic endoscopic mucosal resection. Gastroenterology. 2019; 156:604–613.e3.
Article59. Levy I, Hamerski CM, Nett AS, Calitis J, Binmoeller KF. Su1618 underwater endoscopic mucosal resection (UEMR) of laterally spreading tumors involving the ileocecal valve. Gastrointestinal Endoscopy. 2017; 85:AB366.
Article60. Nakajima T, Saito Y, Tanaka S, et al. Current status of endoscopic resection strategy for large, early colorectal neoplasia in Japan. Surg Endosc. 2013; 27:3262–3270.
Article61. Saito Y, Uraoka T, Yamaguchi Y, et al. A prospective, multicenter study of 1111 colorectal endoscopic submucosal dissections (with video). Gastrointest Endosc. 2010; 72:1217–1225.
Article62. Uraoka T, Parra-Blanco A, Yahagi N. Colorectal endoscopic submucosal dissection: is it suitable in western countries? J Gastroenterol Hepatol. 2013; 28:406–414.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cold snare polypectomy versus cold endoscopic mucosal resection for small colorectal polyps: a meta-analysis of randomized controlled trials
- Endoscopic Treatment for Superficial Nonampullary Duodenal Tumors
- Risk of Delayed Bleeding after a Colorectal Endoscopic Mucosal Resection without Prophylactic Clipping: Single Center, Observational Study
- The Pathological Differences of Colorectal Polyps Examined between the Use of a Forcep Biopsy and Endoscopic Resection
- Endoscopic Mucosal Resection with Circumferential Incision for the Treatment of Large Sessile Polyps and Laterally Spreading Tumors of the Colorectum