Ann Hepatobiliary Pancreat Surg.
2021 May;25(2):270-275. 10.14701/ahbps.2021.25.2.270.
Therapeutic plasma exchange as an effective salvage measure for post-hepatectomy hepatic failure: A case report
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2516251
- DOI: http://doi.org/10.14701/ahbps.2021.25.2.270
Abstract
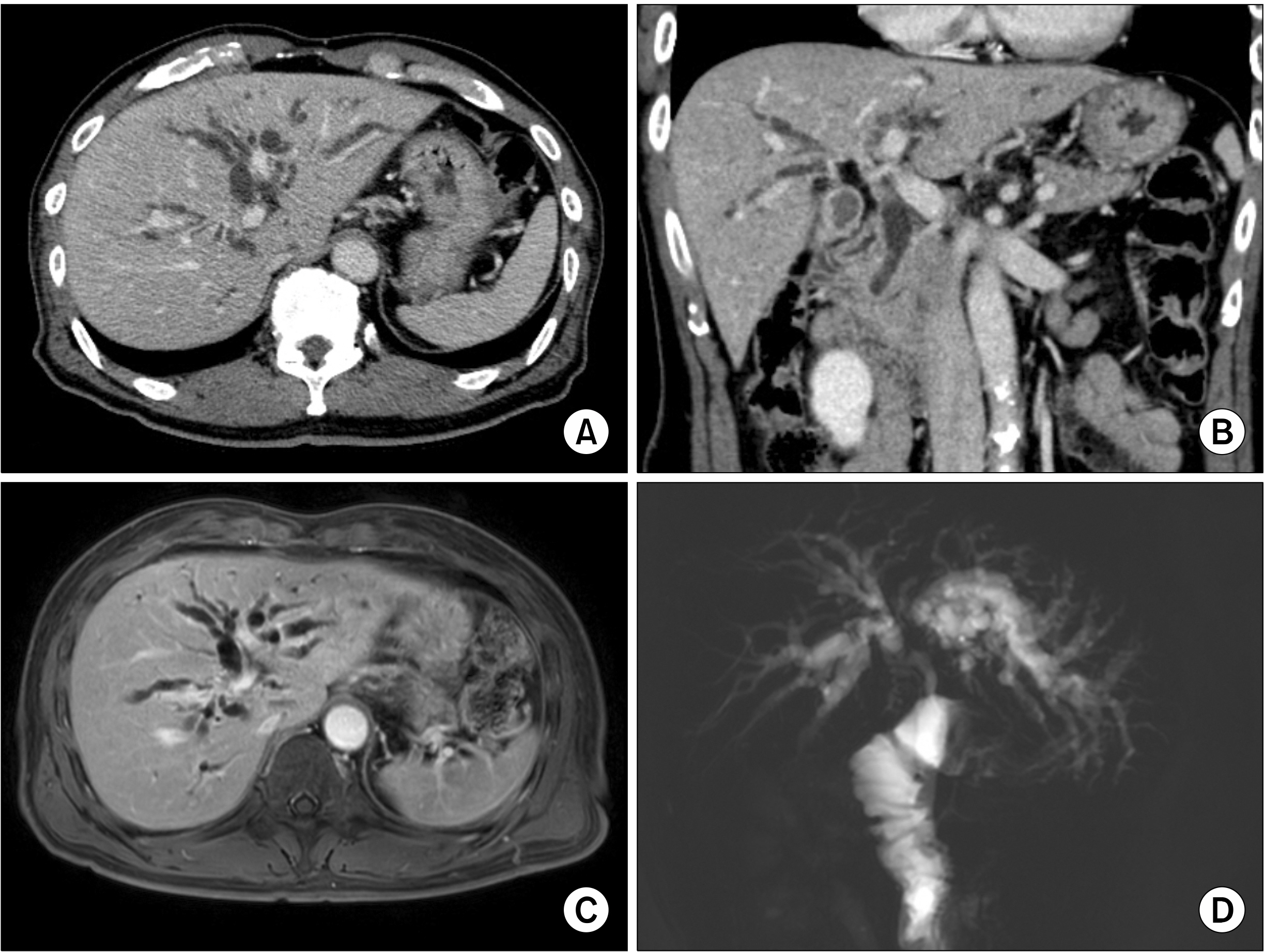
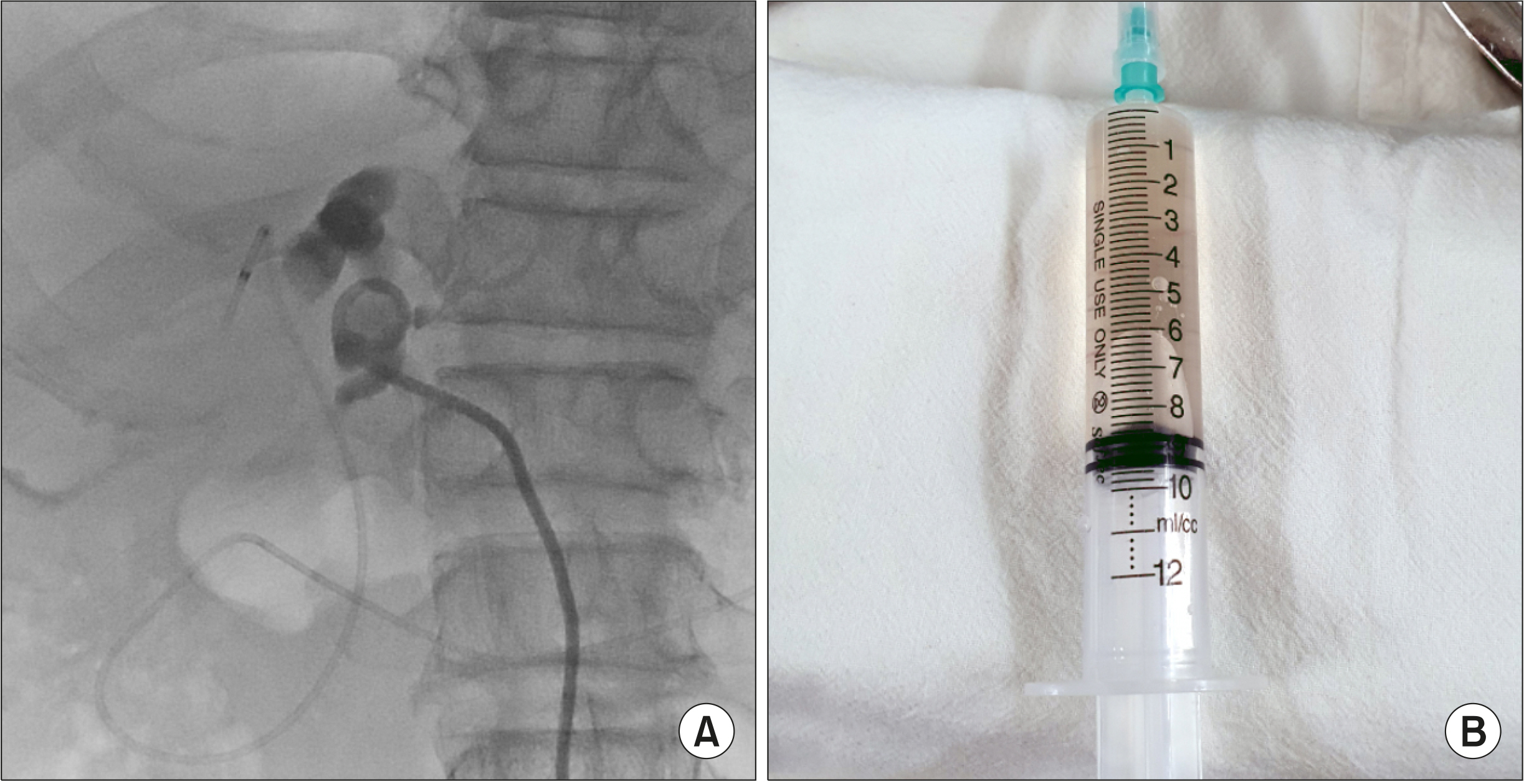
- Major hepatectomy can result in post-hepatectomy hepatic failure (PHHF) and therapeutic plasma exchange (TPE) can be used as a salvage procedure for liver support. We herein present a case of 69-year-old male patient with perihilar cholangiocarcinoma who was successfully managed with salvage TPE. Preoperative portal embolization was performed to reduce the parenchymal resection rate. The extent of surgery was right hepatectomy with partial excision of the ventral portion of the segment IV, caudate lobectomy, bile duct resection and extensive lymph node dissection. No noticeable surgical complications occurred after the operation, but serum total bilirubin level increased gradually and reached 10 mg/dl at 1 month after the operation. At postoperative day 38, total bilirubin level raised to 19.8 mg/dl and prothrombin time deteriorated significantly, thus salvage TPE was started. TPE was performed three times per week for 2 weeks; consequently, the total bilirubin level was maintained below 10 mg/dl. A few days later, a rebound of total bilirubin occurred; accordingly, 2 sessions of TPE were performed additionally. Overall, a total of 8 sessions of TPE were performed. The patient was discharged at 84 days after operation. The total bilirubin level returned to normal at 5 months after operation. This patient is doing well for past 9 months. In Korea, TPE for liver support has been approved by the social health insurance since August 2020. In conclusion, salvage TPE is an effective liver support measure for PHHF, thus we suggest starting TPE if serum total bilirubin level reaches 10 mg/dl after hepatectomy.
Keyword
Figure
Reference
-
1. Lee SG, Hwang S. 2005; How I do it: assessment of hepatic functional reserve for indication of hepatic resection. J Hepatobiliary Pancreat Surg. 12:38–43. DOI: 10.1007/s00534-004-0949-9. PMID: 15754098.
Article2. Shirabe K, Shimada M, Gion T, Hasegawa H, Takenaka K, Utsunomiya T, et al. 1999; Postoperative liver failure after major hepatic resection for hepatocellular carcinoma in the modern era with special reference to remnant liver volume. J Am Coll Surg. 188:304–309. DOI: 10.1016/S1072-7515(98)00301-9.
Article3. Hwang S, Ha TY, Song GW, Jung DH, Ahn CS, Moon DB, et al. 2015; Quantified risk assessment for major hepatectomy via the indocyanine green clearance rate and liver volumetry combined with standard liver volume. J Gastrointest Surg. 19:1305–1314. DOI: 10.1007/s11605-015-2846-8. PMID: 25947549.
Article4. Hwang S, Ha TY, Ahn CS, Kim KH, Lee SG. 2007; Reappraisal of plasmapheresis as a supportive measure in a patient with hepatic failure after major hepatectomy. Case Rep Gastroenterol. 1:162–167. DOI: 10.1159/000107510. PMID: 21487563. PMCID: PMC3073805.
Article5. Choe W, Kwon SW, Kim SS, Hwang S, Song GW, Lee SG. 2017; Effects of therapeutic plasma exchange on early allograft dysfunction after liver transplantation. J Clin Apher. 32:147–153. DOI: 10.1002/jca.21472. PMID: 27306278.
Article6. Park CS, Hwang S, Park HW, Park YH, Lee HJ, Namgoong JM, et al. 2012; Role of plasmapheresis as liver support for early graft dysfunction following adult living donor liver transplantation. Transplant Proc. 44:749–751. DOI: 10.1016/j.transproceed.2012.01.054. PMID: 22483485.
Article7. Lee JY, Kim SB, Chang JW, Park SK, Kwon SW, Song KW, et al. 2010; Comparison of the molecular adsorbent recirculating system and plasmapheresis for patients with graft dysfunction after liver transplantation. Transplant Proc. 42:2625–2630. DOI: 10.1016/j.transproceed.2010.04.070. PMID: 20832557.
Article8. Lafaro K, Buettner S, Maqsood H, Wagner D, Bagante F, Spolverato G, et al. 2015; Defining post hepatectomy liver insufficiency: where do we stand? J Gastrointest Surg. 19:2079–2092. DOI: 10.1007/s11605-015-2872-6. PMID: 26063080.
Article9. Kauffmann R, Fong Y. 2014; Post-hepatectomy liver failure. Hepatobiliary Surg Nutr. 3:238–246.10. Naruse K, Nagashima H, Sakai Y, Kokudo N, Makuuchi M. 2005; Development and perspectives of perfusion treatment for liver failure. Surg Today. 35:507–517. DOI: 10.1007/s00595-004-2980-5. PMID: 15976945.
Article11. Wells CL, Maddaus MA, Simmons RL. 1988; Proposed mechanisms for the translocation of intestinal bacteria. Rev Infect Dis. 10:958–979. DOI: 10.1093/clinids/10.5.958. PMID: 3055194.
Article12. Mandal AK, King KE, Humphreys SL, Maley WR, Burdick JF, Klein AS. 2000; Plasmapheresis: an effective therapy for primary allograft nonfunction after liver transplantation. Transplantation. 70:216–220.13. Ozdemir FN, Tutal E, Sezer S, Gür G, Bilgic A, Haberal M. 2006; Effect of supportive extracorporeal treatment in liver transplantation recipients and advanced liver failure patients. Hemodial Int. 10 Suppl 2:S28–S32. DOI: 10.1111/j.1542-4758.2006.00113.x. PMID: 17022748.
Article14. Inayat F, Hussain Q, Tasleem SH, Farooq S, Hurairah A. 2016; Salvage plasmapheresis for post-hepatectomy liver failure. Cureus. 8:e884. DOI: 10.7759/cureus.884.
Article15. Gui D, Spada PL, De Gaetano A, Pacelli F. 1996; Hypocholesterolemia and risk of death in the critically ill surgical patient. Intensive Care Med. 22:790–794. DOI: 10.1007/BF01709522. PMID: 8880248.
Article16. Giovannini I, Boldrini G, Chiarla C, Giuliante F, Vellone M, Nuzzo G. 1999; Pathophysiologic correlates of hypocholesterolemia in critically ill surgical patients. Intensive Care Med. 25:748–751. DOI: 10.1007/s001340050940. PMID: 10470581.
Article17. Chen J, Song W, Redinger RN. 1996; Effects of dietary cholesterol on hepatic production of lipids and lipoproteins in isolated hamster liver. Hepatology. 24:424–434. DOI: 10.1002/hep.510240222. PMID: 8690415.
Article18. Kaul V, Munoz SJ. 2000; Coagulopathy of liver disease. Curr Treat Options Gastroenterol. 3:433–438. DOI: 10.1007/s11938-000-0030-y. PMID: 11096602.
Article19. Larsen FS, Schmidt LE, Bernsmeier C, Rasmussen A, Isoniemi H, Patel VC, et al. 2016; High-volume plasma exchange in patients with acute liver failure: an open randomised controlled trial. J Hepatol. 64:69–78. DOI: 10.1016/j.jhep.2015.08.018. PMID: 26325537.
Article20. Yamamoto R, Nagasawa Y, Marubashi S, Furumatsu Y, Iwatani H, Iio K, et al. 2009; Early plasma exchange for progressive liver failure in recipients of adult-to-adult living-related liver transplants. Blood Purif. 28:40–46. DOI: 10.1159/000210036. PMID: 19325238.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hemolytic Crisis Recovered by Exchange Transfusion in a Child with Fulminant Wilson's Disease
- A Case of Exertional Heat Stroke with Acute Hepatic Failure Treated with Plasma Exchange: A Case Report
- High-dose Immunoglobulin Infusion for Thrombotic Thrombocytopenic Purpura Refractory to Plasma Exchange and Steroid Therapy
- Plasma Exchange in a Patient with Post-abortion Hemolytic Uremic Syndrome
- Salvage dual graft living donor liver transplantation after major hepatectomy