Ann Surg Treat Res.
2021 Jun;100(6):347-355. 10.4174/astr.2021.100.6.347.
Predictive factors for conservative treatment failure of right colonic diverticulitis
- Affiliations
-
- 1Department of Surgery, Uijeongbu St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Surgery, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 3Department of Surgery, Hallym University College of Medicine, Chuncheon, Korea
- 4Department of Surgery, Ajou University School of Medicine, Suwon, Korea
- KMID: 2516228
- DOI: http://doi.org/10.4174/astr.2021.100.6.347
Abstract
- Purpose
Conservative treatment is the first-line therapy for acute colonic diverticulitis without severe complications, but treatment failure may increase hospitalization duration, medical costs, and morbidities. Usage of the modified Hinchey classification is insufficient to predict the outcome of conservative management. We aimed to investigate the clinical efficacy of the modified Hinchey classification and to evaluate predictive factors such as inflammatory markers for the failure of conservative management.
Methods
Patients diagnosed with right colonic diverticulitis undergoing conservative treatment at 3 hospitals between 2017 and 2019 were included. Patients were categorized into conservative treatment success (n = 494) or failure (n = 46) groups. Clinical characteristics and blood inflammatory markers were assessed.
Results
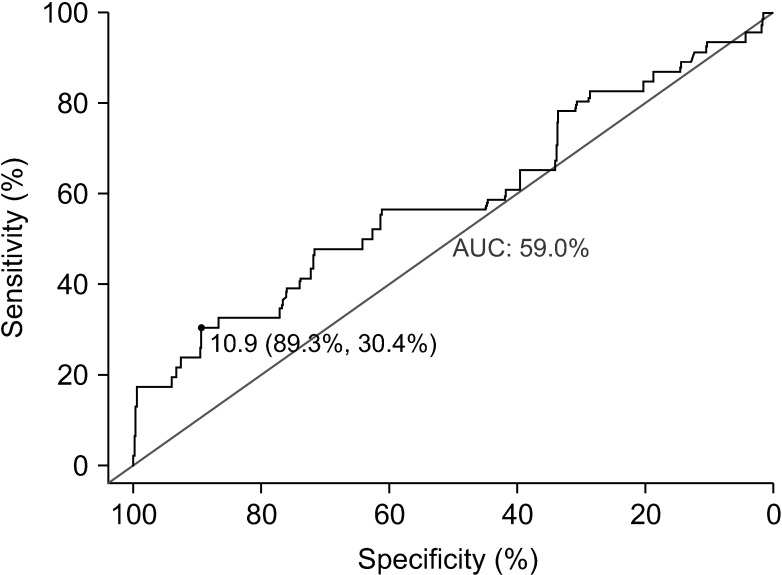
The conservative treatment failure group presented with more elderly patients (>50 years, P = 0.002), more recurrent episodes (P < 0.001), a higher lymphocyte count (P = 0.021), higher C-reactive protein (CRP) levels (P = 0.044), and higher modified Glasgow prognostic scores (P = 0.021). Multivariate analysis revealed that age of >50 years (odds ratio [OR], 2.54; 95% confidence interval [CI], 1.27–5.08; P = 0.008), recurrent episodes (OR, 4.78; 95% CI, 2.38–9.61; P < 0.001), and higher CRP levels (OR, 1.08; 95% CI, 1.03–1.12; P = 0.001) were predictive factors for conservative treatment failure, but not the modified Hinchey grade (P = 0.159).
Conclusion
Age of >50 years, recurrent episodes, and CRP levels are potential predictors for conservative management failure of patients with right-sided colonic diverticulitis. Further studies are warranted to identify candidates requiring early surgical intervention.
Keyword
Figure
Reference
-
1. Hall J, Hammerich K, Roberts P. New paradigms in the management of diverticular disease. Curr Probl Surg. 2010; 47:680–735. PMID: 20684920.
Article2. Paik PS, Yun JA. Clinical features and factors associated with surgical treatment in patients with complicated colonic diverticulitis. Ann Coloproctol. 2017; 33:178–183. PMID: 29159165.
Article3. Shin S, Kim D, Kang UR, Yang CS. Impact of CT imaging on predicting the surgical management of acute diverticulitis. Ann Surg Treat Res. 2018; 94:322–329. PMID: 29854710.
Article4. Bates DD, Fernandez MB, Ponchiardi C, von Plato M, Teich JP, Narsule C, et al. Surgical management in acute diverticulitis and its association with multi-detector CT, modified Hinchey classification, and clinical parameters. Abdom Radiol (NY). 2018; 43:2060–2065. PMID: 29204676.
Article5. Matsushima K. Management of right-sided diverticulitis: a retrospective review from a hospital in Japan. Surg Today. 2010; 40:321–325. PMID: 20339986.
Article6. van Dijk ST, Daniels L, de Korte N, Stockmann HB, Vrouenraets BC, J Consten EC, et al. Quality of life and persistent symptoms after uncomplicated acute diverticulitis. Dis Colon Rectum. 2019; 62:608–614. PMID: 30807455.
Article7. Bolkenstein HE, Consten ECJ, van der Palen J, van de Wall BJ, Broeders IA, Bemelman WA, et al. Long-term outcome of surgery versus conservative management for recurrent and ongoing complaints after an episode of diverticulitis: 5-year follow-up results of a multicenter randomized controlled trial (DIRECT-Trial). Ann Surg. 2019; 269:612–620. PMID: 30247329.8. Jaffer U, Moin T. Perforated sigmoid diverticular disease: a management protocol. JSLS. 2008; 12:188–193. PMID: 18435896.9. Coebergh JW, Janssen-Heijnen ML, Post PN, Razenberg PP. Serious co-morbidity among unselected cancer patients newly diagnosed in the southeastern part of The Netherlands in 1993–1996. J Clin Epidemiol. 1999; 52:1131–1136. PMID: 10580775.
Article10. Kaiser AM, Jiang JK, Lake JP, Ault G, Artinyan A, Gonzalez-Ruiz C, et al. The management of complicated diverticulitis and the role of computed tomography. Am J Gastroenterol. 2005; 100:910–917. PMID: 15784040.
Article11. Huang YQ, Gou R, Diao YS, Yin QH, Fan WX, Liang YP, et al. Charlson comorbidity index helps predict the risk of mortality for patients with type 2 diabetic nephropathy. J Zhejiang Univ Sci B. 2014; 15:58–66. PMID: 24390745.
Article12. Chen JH, Zhai ET, Yuan YJ, Wu KM, Xu JB, Peng JJ, et al. Systemic immune-inflammation index for predicting prognosis of colorectal cancer. World J Gastroenterol. 2017; 23:6261–6272. PMID: 28974892.
Article13. Kishiki T, Masaki T, Matsuoka H, Kobayashi T, Suzuki Y, Abe N, et al. Modified Glasgow prognostic score in patients with incurable stage IV colorectal cancer. Am J Surg. 2013; 206:234–240. PMID: 23827511.
Article14. Hu P, Shen H, Wang G, Zhang P, Liu Q, Du J. Prognostic significance of systemic inf lammation-based lymphocyte- monocyte ratio in patients with lung cancer: based on a large cohort study. PLoS One. 2014; 9:e108062. PMID: 25275631.15. Ranzani OT, Zampieri FG, Forte DN, Azevedo LC, Park M. C-reactive protein/albumin ratio predicts 90-day mortality of septic patients. PLoS One. 2013; 8:e59321. PMID: 23555017.
Article16. Hall JF, Roberts PL, Ricciardi R, Read T, Scheirey C, Wald C, et al. Long-term followup after an initial episode of diverticulitis: what are the predictors of recurrence? Dis Colon Rectum. 2011; 54:283–288. PMID: 21304297.
Article17. Strassle PD, Kinlaw AC, Chaumont N, Angle HL, Lumpkin ST, Koruda MJ, et al. Rates of elective colectomy for diverticulitis continued to increase after 2006 guideline change. Gastroenterology. 2019; 157:1679–1681. PMID: 31499038.
Article18. El-Sayed C, Radley S, Mytton J, Evison F, Ward ST. Risk of recurrent disease and surgery following an admission for acute diverticulitis. Dis Colon Rectum. 2018; 61:382–389. PMID: 29420430.
Article19. Feingold D, Steele SR, Lee S, Kaiser A, Boushey R, Buie WD, et al. Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum. 2014; 57:284–294. PMID: 24509449.
Article20. Hupfeld L, Burcharth J, Pommergaard HC, Rosenberg J. Risk factors for recurrence after acute colonic diverticulitis: a systematic review. Int J Colorectal Dis. 2017; 32:611–622. PMID: 28110383.
Article21. Chapman JR, Dozois EJ, Wolff BG, Gullerud RE, Larson DR. Diverticulitis: a progressive disease? Do multiple recurrences predict less favorable outcomes? Ann Surg. 2006; 243:876–830. PMID: 16772791.22. Ho VP, Nash GM, Milsom JW, Lee SW. Identification of diverticulitis patients at high risk for recurrence and poor outcomes. J Trauma Acute Care Surg. 2015; 78:112–119. PMID: 25539211.
Article23. Salem L, Anaya DA, Flum DR. Temporal changes in the management of diverticulitis. J Surg Res. 2005; 124:318–323. PMID: 15820264.
Article24. Richards RJ, Hammitt JK. Timing of prophylactic surgery in prevention of diverticulitis recurrence: a cost-effectiveness analysis. Dig Dis Sci. 2002; 47:1903–1908. PMID: 12353827.25. Mari A, Khoury T, Lubany A, Safadi M, Farraj M, Farah A, et al. Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios are correlated with complicated diverticulitis and hinchey classification: a simple tool to assess disease severity in the emergency department. Emerg Med Int. 2019; 2019:6321060. PMID: 31485352.
Article26. Reynolds IS, Heaney RM, Khan W, Khan IZ, Waldron R, Barry K. The utility of neutrophil to lymphocyte ratio as a predictor of intervention in acute diverticulitis. Dig Surg. 2017; 34:227–232. PMID: 27941316.
Article27. Kang HS, Cha YS, Park KH, Hwang SO. Delta neutrophil index as a promising prognostic marker of emergent surgical intervention for acute diverticulitis in the emergency department. PLoS One. 2017; 12:e0187629. PMID: 29091955.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Right Colonic Diverticulitis: The Role of Nonoperative Treatment
- Diverticulitis: Focused on Clinical Course and Relapse
- Management of Colonic Diverticulitis Tailored to Location and Severity: Comparison of the Right and the Left Colon
- Clinical Features and Factors Associated With Surgical Treatment in Patients With Complicated Colonic Diverticulitis
- Comparative Study of the Clinical Features and Treatment for Right and Left Colonic Diverticulitis