Ann Surg Treat Res.
2021 Jun;100(6):320-328. 10.4174/astr.2021.100.6.320.
Comparison of perioperative short-term outcomes and oncologic long-term outcomes between open and laparoscopic distal pancreatectomy in patients with pancreatic ductal adenocarcinoma
- Affiliations
-
- 1Department of Surgery and Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2516225
- DOI: http://doi.org/10.4174/astr.2021.100.6.320
Abstract
- Purpose
Laparoscopic distal pancreatectomy (LDP) is widely performed but its efficacy and safety are not established for malignant lesions. This study was aimed to compare outcomes of LDP and open distal pancreatectomy (ODP) in pancreatic ductal adenocarcinoma (PDAC).
Methods
Patients who underwent distal pancreatectomy for PDAC between 2009 and 2017 were enrolled. The preoperative clinical stage was evaluated and propensity score matching (PSM) was performed using age, sex, The American Joint Committee on Cancer 8th clinical T stage, and other organ involvement.
Results
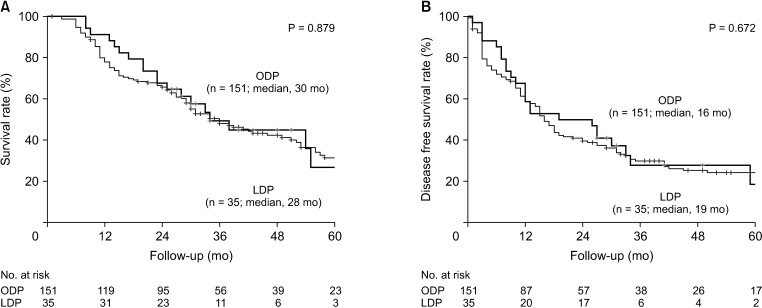
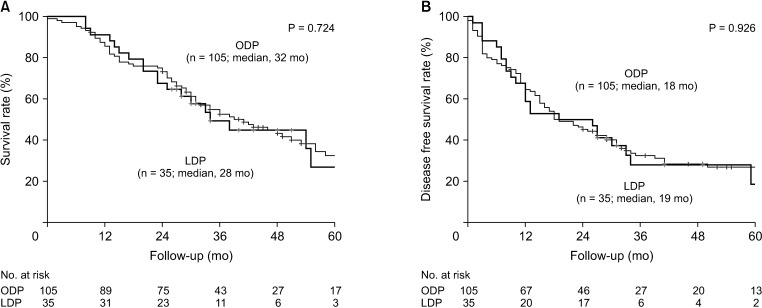
In 186 patients enrolled, 35 (18.8%) received LDP. The ODP group showed larger tumor size and frequent involvement of other organs in preoperative images. However, after PSM, these differences were balanced. R0 resection (90.5% vs. 94.3%, P = 0.730), harvested lymph nodes (14.3 vs. 12.6, P = 0.380) and pathologic T stage (P = 0.474) were comparable between ODP and LDP groups, respectively. LDP demonstrated shorter operation time, less postoperative pain, and shorter hospitalization (14.4 days vs. 11.1 days, P = 0.026). In terms of long-term oncologic outcomes, median overall survival (32 months vs. 28 months, P = 0.724) and disease-free survival (18 months vs. 19 months, P = 0.926) were comparable.
Conclusion
LDP demonstrated better short-term outcomes and comparable long-term outcomes compared with ODP.LDP is a safe and feasible procedure for PDAC.
Figure
Reference
-
1. Kim HH, Hyung WJ, Cho GS, Kim MC, Han SU, Kim W, et al. Morbidity and mortality of laparoscopic gastrectomy versus open gastrectomy for gastric cancer: an interim report. A phase III multicenter, prospective, randomized trial (KLASS Trial). Ann Surg. 2010; 251:417–420. PMID: 20160637.2. Viñuela EF, Gonen M, Brennan MF, Coit DG, Strong VE. Laparoscopic versus open distal gastrectomy for gastric cancer: a meta-analysis of randomized controlled trials and high-quality nonrandomized studies. Ann Surg. 2012; 255:446–456. PMID: 22330034.3. Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MH, de Lange-de Klerk ES, et al. A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med. 2015; 372:1324–1332. PMID: 25830422.
Article4. Hasegawa H, Kabeshima Y, Watanabe M, Yamamoto S, Kitajima M. Randomized controlled trial of laparoscopic versus open colectomy for advanced colorectal cancer. Surg Endosc. 2003; 17:636–640. PMID: 12574925.
Article5. Kennedy RH, Francis EA, Wharton R, Blazeby JM, Quirke P, West NP, et al. Multicenter randomized controlled trial of conventional versus laparoscopic surgery for colorectal cancer within an enhanced recovery programme: EnROL. J Clin Oncol. 2014; 32:1804–1811. PMID: 24799480.
Article6. van der Pas MH, Haglind E, Cuesta MA, Fürst A, Lacy AM, Hop WC, et al. Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol. 2013; 14:210–218. PMID: 23395398.
Article7. Croome KP, Farnell MB, Que FG, Reid-Lombardo KM, Truty MJ, Nagorney DM, et al. Total laparoscopic pancreaticoduodenectomy for pancreatic ductal adenocarcinoma: oncologic advantages over open approaches? Ann Surg. 2014; 260:633–638. PMID: 25203880.8. Song KB, Kim SC, Hwang DW, Lee JH, Lee DJ, Lee JW, et al. Matched case-control analysis comparing laparoscopic and open pylorus-preserving pancreaticoduodenectomy in patients with periampullary tumors. Ann Surg. 2015; 262:146–155. PMID: 25563866.
Article9. de Rooij T, van Hilst J, van Santvoort H, Boerma D, van den Boezem P, Daams F, et al. Minimally invasive versus open distal pancreatectomy (LEOPARD): a multicenter patient-blinded randomized controlled trial. Ann Surg. 2019; 269:2–9. PMID: 30080726.10. Kooby DA, Hawkins WG, Schmidt CM, Weber SM, Bentrem DJ, Gillespie TW, et al. A multicenter analysis of distal pancreatectomy for adenocarcinoma: is laparoscopic resection appropriate? J Am Coll Surg. 2010; 210:779–785. PMID: 20421049.
Article11. Rehman S, John SK, Lochan R, Jaques BC, Manas DM, Charnley RM, et al. Oncological feasibility of laparoscopic distal pancreatectomy for adenocarcinoma: a single-institution comparative study. World J Surg. 2014; 38:476–483. PMID: 24081543.
Article12. Zhang M, Fang R, Mou Y, Chen R, Xu X, Zhang R, et al. LDP vs ODP for pancreatic adenocarcinoma: a case matched study from a single-institution. BMC Gastroenterol. 2015; 15:182. PMID: 26695506.
Article13. Kim EY, Hong TH. Initial experience with laparoscopic radical antegrade modular pancreatosplenectomy for left-sided pancreatic cancer in a single institution: technical aspects and oncological outcomes. BMC Surg. 2017; 17:2. PMID: 28061895.
Article14. Kim S, Yoon YS, Han HS, Cho JY. Laparoscopic subtotal pancreatectomy with radical antegrade modular pancreatosplenectomy for left-sided pancreatic cancer. Surg Oncol. 2019; 28:150. PMID: 30851891.
Article15. Lee SH, Kang CM, Hwang HK, Choi SH, Lee WJ, Chi HS. Minimally invasive RAMPS in well-selected left-sided pancreatic cancer within Yonsei criteria: long-term (>median 3 years) oncologic outcomes. Surg Endosc. 2014; 28:2848–2855. PMID: 24853839.16. Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 2017; 161:584–591. PMID: 28040257.17. Geer RJ, Brennan MF. Prognost ic indicators for survival after resection of pancreatic adenocarcinoma. Am J Surg. 1993; 165:68–72. PMID: 8380315.18. Ozaki H, Kishi K. Lymph node dissection in radical resection for carcinoma of the head of the pancreas and periampullary region. Jpn J Clin Oncol. 1983; 13:371–377. PMID: 6887557.19. Fatima J, Schnelldorfer T, Barton J, Wood CM, Wiste HJ, Smyrk TC, et al. Pancreatoduodenectomy for ductal adenocarcinoma: implications of positive margin on survival. Arch Surg. 2010; 145:167–172. PMID: 20157085.20. Moon HJ, An JY, Heo JS, Choi SH, Joh JW, Kim YI. Predicting survival after surgical resection for pancreatic ductal adenocarcinoma. Pancreas. 2006; 32:37–43. PMID: 16340742.
Article21. Zhang AB, Wang Y, Hu C, Shen Y, Zheng SS. Laparoscopic versus open distal pancreatectomy for pancreatic ductal adenocarcinoma: a single-center experience. J Zhejiang Univ Sci B. 2017; 18:532–538. PMID: 28585429.
Article22. Bauman MD, Becerra DG, Kilbane EM, Zyromski NJ, Schmidt CM, Pitt HA, et al. Laparoscopic distal pancreatectomy for pancreatic cancer is safe and effective. Surg Endosc. 2018; 32:53–61. PMID: 28643065.
Article23. van Hilst J, de Rooij T, Klompmaker S, Rawashdeh M, Aleotti F, Al-Sarireh B, et al. Minimally invasive versus open distal pancreatectomy for ductal adenocarcinoma (DIPLOMA): a pan-European propensity score matched study. Ann Surg. 2019; 269:10–17. PMID: 29099399.24. Shin SH, Kim SC, Song KB, Hwang DW, Lee JH, Lee D, et al. A comparative study of laparoscopic vs. open distal pancreatectomy for left-sided ductal adenocarcinoma: a propensity scorematched analysis. J Am Coll Surg. 2015; 220:177–185. PMID: 25529901.
Article25. Heinemann V, Boeck S, Hinke A, Labianca R, Louvet C. Meta-analysis of randomized trials: evaluation of benefit from gemcitabine-based combination chemotherapy applied in advanced pancreatic cancer. BMC Cancer. 2008; 8:82. PMID: 18373843.
Article26. Oettle H, Neuhaus P, Hochhaus A, Hartmann JT, Gellert K, Ridwelski K, et al. Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: the CONKO-001 randomized trial. JAMA. 2013; 310:1473–1481. PMID: 24104372.27. Neoptolemos JP, Stocken DD, Friess H, Bassi C, Dunn JA, Hickey H, et al. A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. N Engl J Med. 2004; 350:1200–1210. PMID: 15028824.
Article28. Sulpice L, Farges O, Goutte N, Bendersky N, Dokmak S, Sauvanet A, et al. Laparoscopic distal pancreatectomy for pancreatic ductal adenocarcinoma: time for a randomized controlled trial? Results of an all-inclusive national observational study. Ann Surg. 2015; 262:868–873. PMID: 26583678.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current status of robotic surgery for pancreatic tumors
- Comparison of perioperative outcomes in pancreatic head cancer patients following either a laparoscopic or open pancreaticoduodenectomy with a superior mesenteric artery first approach
- Comparison of Laparoscopy and Exploration in the Distal Pancreatectomy
- Comparison of Long-term Survival for Laparoscopic-assisted Surgery and Open Surgery for Right Colon Cancer: A Case-Control Study
- Robotic major liver resections: Surgical outcomes compared with open major liver resections