Korean Circ J.
2021 Jun;51(6):518-529. 10.4070/kcj.2020.0443.
Hospital Case Volume, Health Care Providers, and Mortality in Patients Undergoing Coronary Artery Bypass Grafting: a Nationwide Cohort Study in South Korea
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2516213
- DOI: http://doi.org/10.4070/kcj.2020.0443
Abstract
- Background and Objectives
Surgical quality is evaluated by measuring the annual hospital case volume; a higher case volume is associated with better survival after various surgeries. We aimed to investigate if the annual hospital case volume and the health care providers were associated with a 90-day mortality after coronary artery bypass grafting (CABG).
Methods
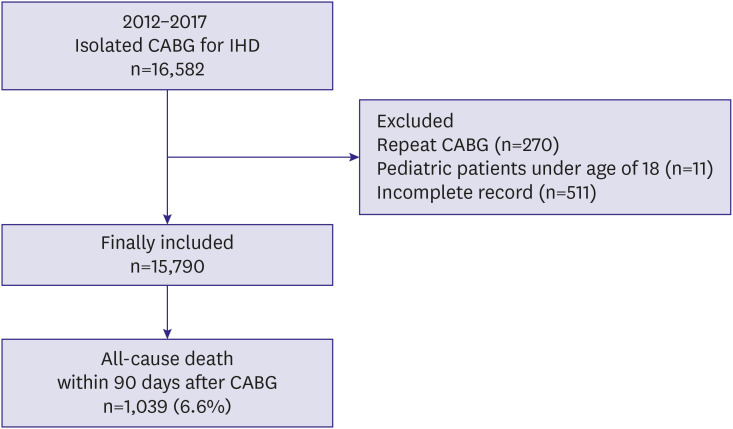
For this population-based cohort study, we used data from a National Health Insurance Service database in South Korea. We included all adult patients diagnosed with ischemic heart disease who underwent isolated CABG between January 2012 and December 2017. Data on the annual surgical volume for CABG in each hospital where the patients received CABG and the total number of health care providers (including physicians [trainees and specialists] from all department of the hospitals, nurses, and pharmacists) were collected.
Results
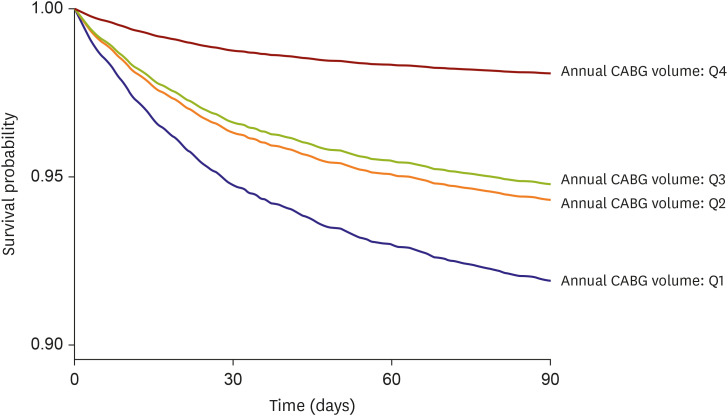
The final analysis included 15,790 adult patients; of these, 1,039 (6.6%) died within 90 days. The annual CABG volume was divided into 4 groups (Q1: ≤33, Q2: 34–86, Q3: 87– 223, and Q4: ≥224). Multivariable Cox regression analysis revealed that the 90-day mortality rates in the Q4, Q3, Q2 groups were 75%, 32%, and 31% lower than that in the Q1 group, respectively. Additionally, an increase in the ratio of the total number of specialist physicians to 100 hospital beds was associated with a 4% decrease in the 90-day mortality after CABG.
Conclusion
Both, a higher annual hospital case volume and overall specialist physician volume were associated with better 90-day mortality rates after isolated CABG.
Keyword
Figure
Cited by 1 articles
-
Does Hospital Volume of Coronary Artery Bypass Graft Matter on Mid-Term Mortality?: from the Data of National Health Insurance Service in Korea
Jang-Whan Bae
Korean Circ J. 2021;51(6):530-532. doi: 10.4070/kcj.2021.0122.
Reference
-
1. Sanchis-Gomar F, Perez-Quilis C, Leischik R, Lucia A. Epidemiology of coronary heart disease and acute coronary syndrome. Ann Transl Med. 2016; 4:256. PMID: 27500157.
Article2. Epstein AJ, Polsky D, Yang F, Yang L, Groeneveld PW. Coronary revascularization trends in the United States, 2001-2008. JAMA. 2011; 305:1769–1776. PMID: 21540420.
Article3. Head SJ, Milojevic M, Daemen J, et al. Mortality after coronary artery bypass grafting versus percutaneous coronary intervention with stenting for coronary artery disease: a pooled analysis of individual patient data. Lancet. 2018; 391:939–948. PMID: 29478841.
Article4. Alexander JH, Smith PK. Coronary-artery bypass grafting. N Engl J Med. 2016; 374:1954–1964. PMID: 27192673.
Article5. Adelborg K, Horváth-Puhó E, Schmidt M, et al. Thirty-year mortality after coronary artery bypass graft surgery: a Danish nationwide population-based cohort study. Circ Cardiovasc Qual Outcomes. 2017; 10:e002708. PMID: 28500223.6. Erickson LC, Torchiana DF, Schneider EC, Newburger JW, Hannan EL. The relationship between managed care insurance and use of lower-mortality hospitals for CABG surgery. JAMA. 2000; 283:1976–1982. PMID: 10789665.
Article7. Ghali WA, Ash AS, Hall RE, Moskowitz MA. Statewide quality improvement initiatives and mortality after cardiac surgery. JAMA. 1997; 277:379–382. PMID: 9010169.
Article8. Dimick JB, Birkmeyer JD, Upchurch GR Jr. Measuring surgical quality: What's the role of provider volume? World J Surg. 2005; 29:1217–1221. PMID: 16132399.
Article9. Finlayson SR. The volume-outcome debate revisited. Am Surg. 2006; 72:1038–1042. PMID: 17120945.
Article10. Dikken JL, Dassen AE, Lemmens VE, et al. Effect of hospital volume on postoperative mortality and survival after oesophageal and gastric cancer surgery in the Netherlands between 1989 and 2009. Eur J Cancer. 2012; 48:1004–1013. PMID: 22456179.
Article11. Gooiker GA, van Gijn W, Wouters MW, et al. Systematic review and meta-analysis of the volume-outcome relationship in pancreatic surgery. Br J Surg. 2011; 98:485–494. PMID: 21500187.
Article12. Hata T, Motoi F, Ishida M, et al. Effect of hospital volume on surgical outcomes after pancreaticoduodenectomy: a systematic review and meta-analysis. Ann Surg. 2016; 263:664–672. PMID: 26636243.13. Cowan JA Jr, Dimick JB, Leveque JC, Thompson BG, Upchurch GR Jr, Hoff JT. The impact of provider volume on mortality after intracranial tumor resection. Neurosurgery. 2003; 52:48–53. PMID: 12493100.
Article14. Auerbach AD, Hilton JF, Maselli J, Pekow PS, Rothberg MB, Lindenauer PK. Case volume, quality of care, and care efficiency in coronary artery bypass surgery. Arch Intern Med. 2010; 170:1202–1208. PMID: 20660837.
Article15. Hannan EL, Kilburn H Jr, Bernard H, O'Donnell JF, Lukacik G, Shields EP. Coronary artery bypass surgery: the relationship between inhospital mortality rate and surgical volume after controlling for clinical risk factors. Med Care. 1991; 29:1094–1107. PMID: 1943270.16. Wen HC, Tang CH, Lin HC, Tsai CS, Chen CS, Li CY. Association between surgeon and hospital volume in coronary artery bypass graft surgery outcomes: a population-based study. Ann Thorac Surg. 2006; 81:835–842. PMID: 16488681.
Article17. Wu SC, Chien LN, Ng YY, Chu HF, Chen CC. Association of case volume with mortality of Chinese patients after coronary artery bypass grafting: Taiwan experience. Circ J. 2005; 69:1327–1332. PMID: 16247206.18. Kurlansky PA, Argenziano M, Dunton R, et al. Quality, not volume, determines outcome of coronary artery bypass surgery in a university-based community hospital network. J Thorac Cardiovasc Surg. 2012; 143:287–293.e1. PMID: 22104669.
Article19. Lee KS, Kim CS, Park JH, et al. The longitudinal trend of cardiac surgery in Korea from 2003 to 2013. Korean J Thorac Cardiovasc Surg. 2016; 49:S1–13. PMID: 28035292.
Article20. Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Ann Intern Med. 2007; 147:W163–94. PMID: 17938389.
Article21. Ruopp MD, Perkins NJ, Whitcomb BW, Schisterman EF. Youden index and optimal cut-point estimated from observations affected by a lower limit of detection. Biom J. 2008; 50:419–430. PMID: 18435502.
Article22. Harold JG, Bass TA, Bashore TM, et al. ACCF/AHA/SCAI 2013 update of the clinical competence statement on coronary artery interventional procedures: a report of the American College of Cardiology Foundation/American Heart Association/American College of Physicians Task Force on clinical competence and training (writing committee to revise the 2007 clinical competence statement on cardiac interventional procedures). Catheter Cardiovasc Interv. 2013; 82:E69–E111. PMID: 23653399.23. Kilic A, Shah AS, Conte JV, Baumgartner WA, Yuh DD. Operative outcomes in mitral valve surgery: combined effect of surgeon and hospital volume in a population-based analysis. J Thorac Cardiovasc Surg. 2013; 146:638–646. PMID: 22914251.24. Joynt KE, Orav EJ, Jha AK. Physician volume, specialty, and outcomes of care for patients with heart failure. Circ Heart Fail. 2013; 6:890–897. PMID: 23926203.
Article25. Chu D, Anastacio MM, Mulukutla SR, et al. Safety and efficacy of implementing a multidisciplinary heart team approach for revascularization in patients with complex coronary artery disease: an observational cohort pilot study. JAMA Surg. 2014; 149:1109–1112. PMID: 25207883.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Wrapping of an Ascending Aortic Aneurysm with the Multiple Boot-Straps Technique in a Patient Undergoing Off-Pump Coronary Artery Bypass Grafting
- Awake OPCAB: Initial Experience
- Clinical Results of Mitral Valvular Surgery in Patients with Moderate Ischemic Mitral Regurgitation Undergoing Coronary Artery Bypass Grafting
- Effect of Postoperative Constrictive Physiology on Early Outcomes after Off-Pump Coronary Artery Bypass Grafting
- Native Coronary Artery and Grafted Artery Spasm Just after Coronary Artery Bypass Grafting: A Case Report