Int J Thyroidol.
2021 May;14(1):6-17. 10.11106/ijt.2021.14.1.6.
Clinical Outcome of Parotid Gland Massage for Preventing Parotid Gland Dysfunction in Patients Treated with Radioiodine Therapy for Differentiated Thyroid Cancer: a Prospective Longitudinal Follow-Up Study
- Affiliations
-
- 1Department of Nuclear Medicine, School of Medicine, Kyungpook National University, Kyungpook National University Hospital, Daegu, Korea
- KMID: 2516160
- DOI: http://doi.org/10.11106/ijt.2021.14.1.6
Abstract
- Background and Objectives
The aim of this study was to determine the clinical effectiveness of parotid gland (PG) massage for the prevention of PG dysfunction after administration of radioiodine (I-131) therapy for treatment of differentiated thyroid cancer (DTC).
Materials and Methods
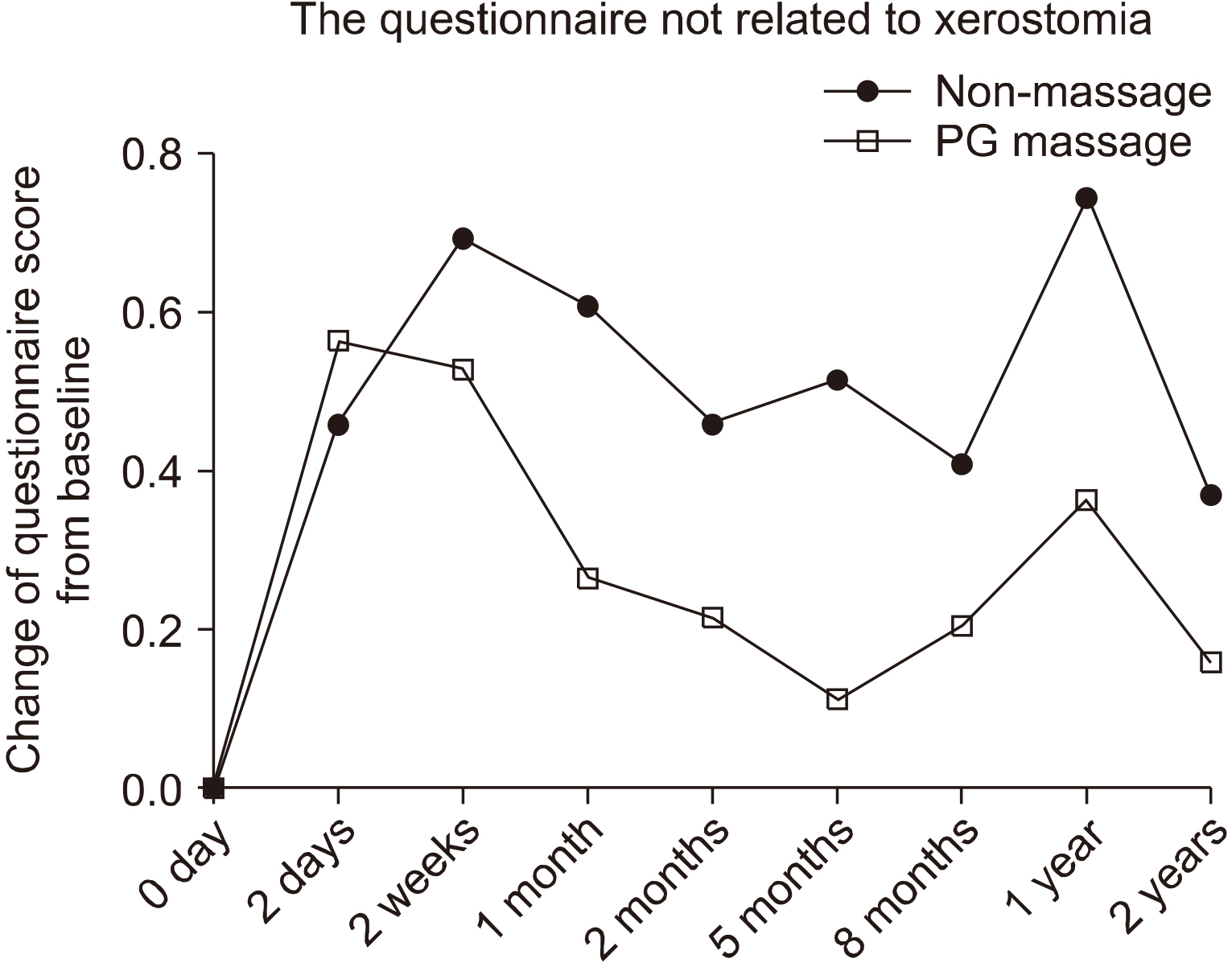
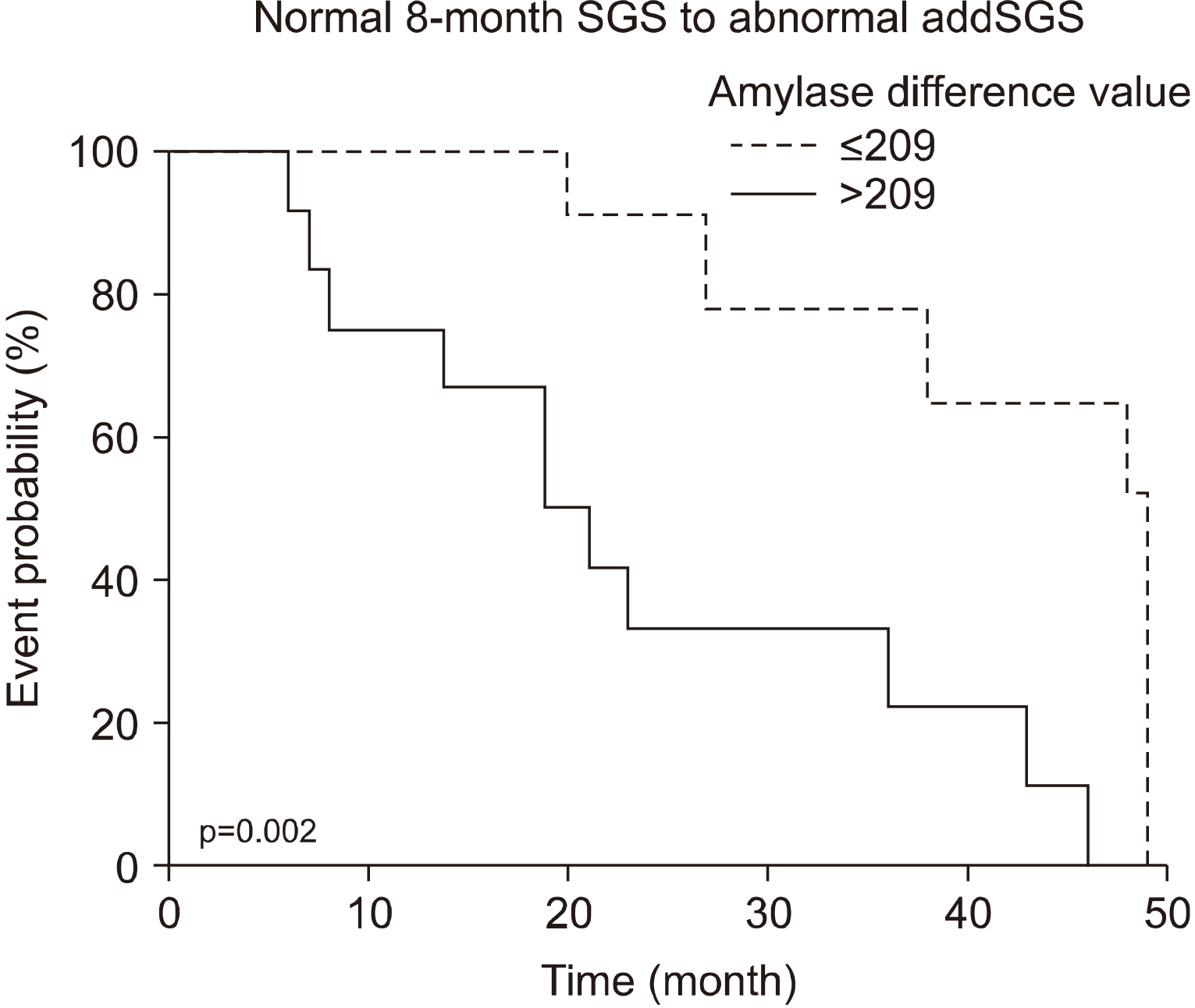
One hundred patients with DTC with planned high-dose I-131 therapy were enrolled in the clinical trial and randomized into two groups (massage and non-massage group). Serum amylase values were obtained before and 24 h after I-131 therapy, and salivary gland scintigraphy (SGS) were taken before and at eight months after the I-131 therapy. Additional SGS (addSGS) were taken when the patients complained symptoms related to salivary gland dysfunction. Questionnaire surveys were performed before and until two years after I-131 therapy.
Results
Ninety-five of 100 patients finished the study protocol. Changes in survey scores tended to be higher in the non-massage group. The non-massage group had more severe symptoms related to salivary gland dysfunction. Among 32 patients who underwent addSGS, 27 had normal 8-month SGS. Of these 27 patients, 18 (66.7%) had salivary gland dysfunction on the addSGS. Amylase values were significantly increased in patients with normal 8-month SGS but abnormal addSGS, as compared to patients who were normal on both 8-month SGS and addSGS (p=0.046). Amylase difference values were a significant predictor of abnormal addSGS (p=0.002). Conclusion: PG massage reduced symptoms related to salivary gland dysfunction. The PG massage may be helpful in preventing damage to salivary glands caused by I-131 therapy.
Figure
Reference
-
References
1. Ahn BC. 2016; Personalized medicine based on theranostic radioiodine molecular imaging for differentiated thyroid cancer. Biomed Res Int. 2016:1680464. DOI: 10.1155/2016/1680464. PMID: 27239470. PMCID: PMC4864569.
Article2. Hong CM, Ahn BC. 2017; Redifferentiation of radioiodine refractory differentiated thyroid cancer for reapplication of I-131 therapy. Front Endocrinol (Lausanne). 8:260. DOI: 10.3389/fendo.2017.00260. PMID: 29085335. PMCID: PMC5649198.
Article3. Hong CM, Kim CY, Son SH, Jung JH, Lee CH, Jeong JH, et al. 2017; I-131 biokinetics of remnant normal thyroid tissue and residual thyroid cancer in patients with differentiated thyroid cancer: comparison between recombinant human TSH admini-stration and thyroid hormone withdrawal. Ann Nucl Med. 31(8):582–9. DOI: 10.1007/s12149-017-1188-x. PMID: 28677070.
Article4. Jeong JH, Kong EJ, Jeong SY, Lee SW, Cho IH, Ah Chun K, et al. 2017; Clinical outcomes of low-dose and high-dose post-operative radioiodine therapy in patients with intermediate-risk differentiated thyroid cancer. Nucl Med Commun. 38(3):228–33. DOI: 10.1097/MNM.0000000000000636. PMID: 27984538.
Article5. Alexander C, Bader JB, Schaefer A, Finke C, Kirsch CM. 1998; Intermediate and long-term side effects of high-dose radioiodine therapy for thyroid carcinoma. J Nucl Med. 39(9):1551–4. PMID: 9744341.6. Allweiss P, Braunstein GD, Katz A, Waxman A. 1984; Sialadenitis following I-131 therapy for thyroid carcinoma: concise com-munication. J Nucl Med. 25(7):755–8. PMID: 6737074.7. Kita T, Yokoyama K, Higuchi T, Kinuya S, Taki J, Nakajima K, et al. 2004; Multifactorial analysis on the short-term side effects occurring within 96 hours after radioiodine-131 therapy for differentiated thyroid carcinoma. Ann Nucl Med. 18(4):345–9. DOI: 10.1007/BF02984474. PMID: 15359929.8. Hong CM, Son SH, Kim CY, Kim DH, Jeong SY, Lee SW, et al. 2014; Emptying effect of massage on parotid gland radioiodine content. Nucl Med Commun. 35(11):1127–31. DOI: 10.1097/MNM.0000000000000176. PMID: 25121980.
Article9. Kim HW, Ahn BC, Lee SW, Lee J. 2012; Effect of parotid gland massage on parotid gland Tc-99m pertechnetate uptake. Thyroid. 22(6):611–6. DOI: 10.1089/thy.2011.0188. PMID: 22524471. PMCID: PMC3358109.
Article10. Son SH, Lee CH, Jung JH, Kim DH, Hong CM, Jeong JH, et al. 2019; The preventive effect of parotid gland massage on salivary gland dysfunction during high-dose radioactive iodine therapy for differentiated thyroid cancer: a randomized clinical trial. Clin Nucl Med. 44(8):625–33. DOI: 10.1097/RLU.0000000000002602. PMID: 31274608.11. Becciolini A, Giannardi G, Cionini L, Porciani S, Fallai C, Pirtoli L. 1984; Plasma amylase activity as a biochemical indicator of radiation injury to salivary glands. Acta Radiol Oncol. 23(1):9–14. DOI: 10.3109/02841868409135978. PMID: 6203336.
Article12. Kishima HK, Kirkham WR, Andrews JR. 1965; Post-irradiation sialadenitis. A study of the clinical features, histopathologic changes and serum enzyme variations following irradiation of human salivary glands. Am J Roentgenol Radium Therapy Nucl Med. 94:271–91.13. Van den Brenk HA, Hurley RA, Gomez C, Richter W. 1969; Serum amylase as a measure of salivary gland radiation damage. Hyperamylasaemia following fractionated exposure to 4 MV X rays delivered in high pressure oxygen, and effects of certain steroids on this response. Br J Radiol. 42(501):688–700. DOI: 10.1259/0007-1285-42-501-688. PMID: 4981289.14. Eisbruch A, Kim HM, Terrell JE, Marsh LH, Dawson LA, Ship JA. 2001; Xerostomia and its predictors following parotid-sparing irradiation of head-and-neck cancer. Int J Radiat Oncol Biol Phys. 50(3):695–704. DOI: 10.1016/S0360-3016(01)01512-7. PMID: 11395238.
Article15. Ahn BC. 2012; Sodium iodide symporter for nuclear molecular imaging and gene therapy: from bedside to bench and back. Theranostics. 2(4):392–402. DOI: 10.7150/thno.3722. PMID: 22539935. PMCID: PMC3337731.
Article16. De La Vieja A, Dohan O, Levy O, Carrasco N. 2000; Molecular analysis of the sodium/iodide symporter: impact on thyroid and extrathyroid pathophysiology. Physiol Rev. 80(3):1083–105. DOI: 10.1152/physrev.2000.80.3.1083. PMID: 10893432.17. Mandel SJ, Mandel L. 2003; Radioactive iodine and the salivary glands. Thyroid. 13(3):265–71. DOI: 10.1089/105072503321582060. PMID: 12729475.
Article18. Oh JR, Ahn BC. 2012; False-positive uptake on radioiodine whole- body scintigraphy: physiologic and pathologic variants unrelated to thyroid cancer. Am J Nucl Med Mol Imaging. 2(3):362–85. PMID: 23133823. PMCID: PMC3477738.19. Hall EJ. 2000. Radiobiology for the radiologist. 5th ed. Lippincott Williams & Wilkins;Philadelphia:20. Van Nostrand D. 2011; Sialoadenitis secondary to (1)(3)(1)I therapy for well-differentiated thyroid cancer. Oral Dis. 17(2):154–61. DOI: 10.1111/j.1601-0825.2010.01726.x. PMID: 21029259.
Article21. Fox PC. 1998; Acquired salivary dysfunction. Drugs and radiation. Ann N Y Acad Sci. 842:132–7. DOI: 10.1111/j.1749-6632.1998.tb09641.x. PMID: 9599303.
Article22. van Luijk P, Pringle S, Deasy JO, Moiseenko VV, Faber H, Hovan A, et al. 2015; Sparing the region of the salivary gland con-taining stem cells preserves saliva production after radiotherapy for head and neck cancer. Sci Transl Med. 7(305):305ra147. DOI: 10.1126/scitranslmed.aac4441. PMID: 26378247. PMCID: PMC4964284.
Article23. Klein Hesselink EN, Links TP. 2015; Radioiodine treatment and thyroid hormone suppression therapy for differentiated thyroid carcinoma: adverse effects support the trend toward less aggressive treatment for low-risk patients. Eur Thyroid J. 4(2):82–92. DOI: 10.1159/000432397. PMID: 26279993. PMCID: PMC4521066.
Article24. Jeong SY, Kim HW, Lee SW, Ahn BC, Lee J. 2013; Salivary gland function 5 years after radioactive iodine ablation in patients with differentiated thyroid cancer: direct comparison of pre- and postablation scintigraphies and their relation to xerostomia symptoms. Thyroid. 23(5):609–16. DOI: 10.1089/thy.2012.0106. PMID: 23153322. PMCID: PMC3643252.
Article25. Hancock PJ, Epstein JB, Sadler GR. 2003; Oral and dental management related to radiation therapy for head and neck cancer. J Can Dent Assoc. 69(9):585–90. PMID: 14653934.26. Cady J. 2007; Nutritional support during radiotherapy for head and neck cancer: the role of prophylactic feeding tube placement. Clin J Oncol Nurs. 11(6):875–80. DOI: 10.1188/07.CJON.875-880. PMID: 18063546.
Article27. Li Y, Taylor JM, Ten Haken RK, Eisbruch A. 2007; The impact of dose on parotid salivary recovery in head and neck cancer patients treated with radiation therapy. Int J Radiat Oncol Biol Phys. 67(3):660–9. DOI: 10.1016/j.ijrobp.2006.09.021. PMID: 17141973. PMCID: PMC2001308.
Article28. Stephens LC, King GK, Peters LJ, Ang KK, Schultheiss TE, Jardine JH. 1986; Acute and late radiation injury in rhesus monkey parotid glands. Evidence of interphase cell death. Am J Pathol. 124(3):469–78. PMID: 3766705. PMCID: PMC1888342.29. Marmary Y, Adar R, Gaska S, Wygoda A, Maly A, Cohen J, et al. 2016; Radiation-induced loss of salivary gland function is driven by cellular senescence and prevented by IL6 modulation. Cancer Res. 76(5):1170–80. DOI: 10.1158/0008-5472.CAN-15-1671. PMID: 26759233.
Article30. Pawlikowski JS, Adams PD, Nelson DM. 2013; Senescence at a glance. J Cell Sci. 126(Pt 18):4061–7. DOI: 10.1242/jcs.109728. PMID: 23970414. PMCID: PMC3772382.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Significance of Salivary Gland Radioiodine Retention on Post-ablation 131I Scintigraphy as a Predictor of Salivary Gland Dysfunction in Patients with Differentiated Thyroid Carcinoma
- A Case of Parotid Tuberculosis Mimicking Benign Tumor of Parotid Gland
- A Case of Metachronous Carcinosarcoma and Squamous Cell Carcinoma of the Both Parotid Glands
- Unilateral Agenesis of the Parotid Gland: A Case Report
- Usefulness of Sialendoscopy for Sialadenitis after Radioactive Iodine Therapy