Obstet Gynecol Sci.
2021 May;64(3):332-335. 10.5468/ogs.21025.
Efficient myometrial defect closure in a layer by layer fashion after robot-assisted laparoscopic adenomyomectomy: a novel technique
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Seoul St. Mary's Fibroid Center, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2515988
- DOI: http://doi.org/10.5468/ogs.21025
Abstract
Objective
In this video, we present our novel technique for myometrial defect closure following robot-assisted laparoscopic adenomyomectomy.
Methods
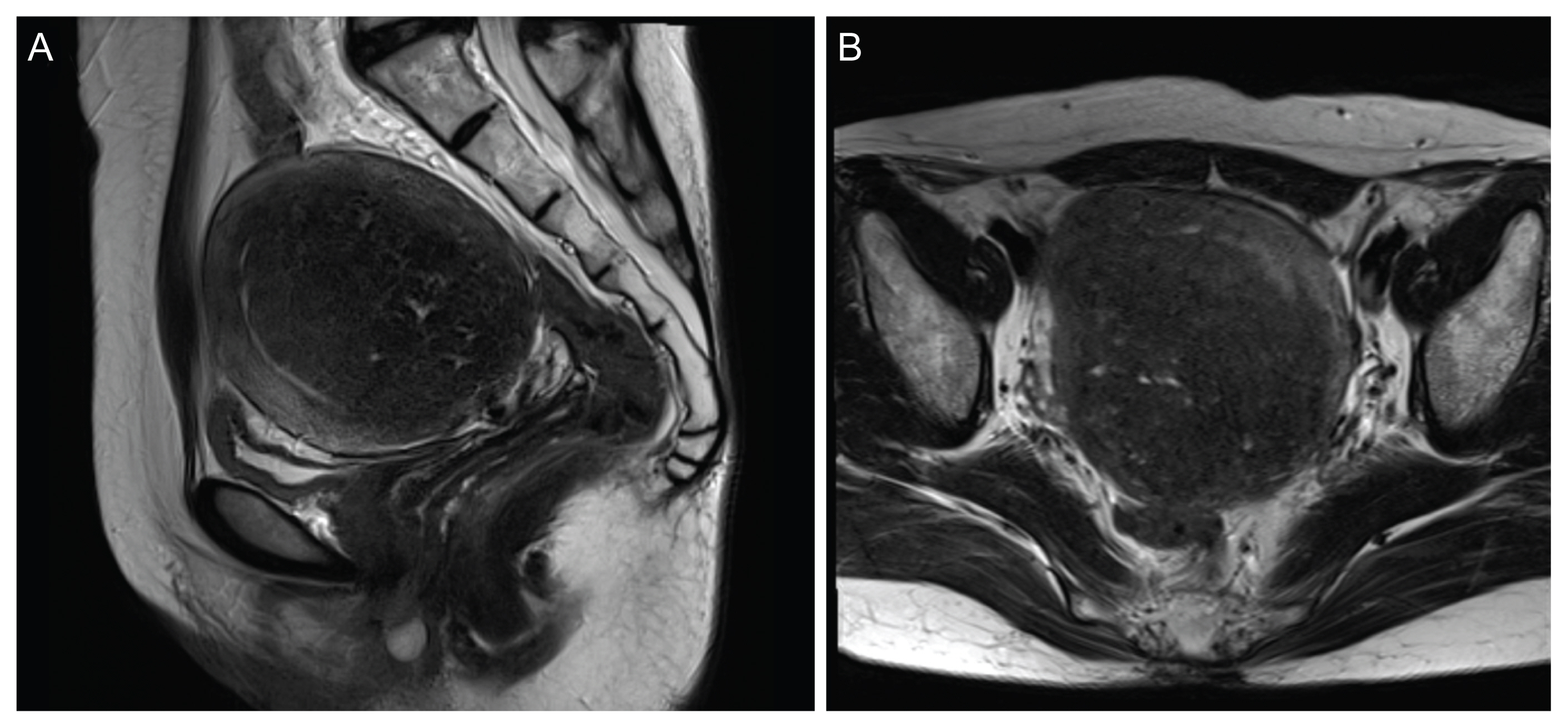
A narrated video demonstration of our technique. Our patient was a 47-year-old single woman with severe dysmenorrhea, who did not respond to medical therapy and wished to preserve her uterus. Surgery was performed after thorough counseling and obtaining informed consent from the patient (Institutional Review Board number: KC17OESI0238; approval date: March 19, 2018). After removal of the adenomyotic tissue during surgical intervention, the myometrial defect was closed in three steps. First, the defect between the anterior and posterior innermost myometrial layers was closed using a 2-0 Stratafix suture, CT-1 (circle taper) needle (Ethicon, Somerville, NJ, USA). Next, the two sides were approximated using a 2-0 PDS® (polydioxanone) Suture (Ethicon, Somerville, NJ, USA) and V-34 (TAPERCUT®) surgical needle (Ethicon, Somerville, NJ, USA). Finally, the serosa was sutured in a baseball fashion using a 2-0 PDS suture, slim half-circle [SH] needle (Ethicon, Somerville, NJ, USA).
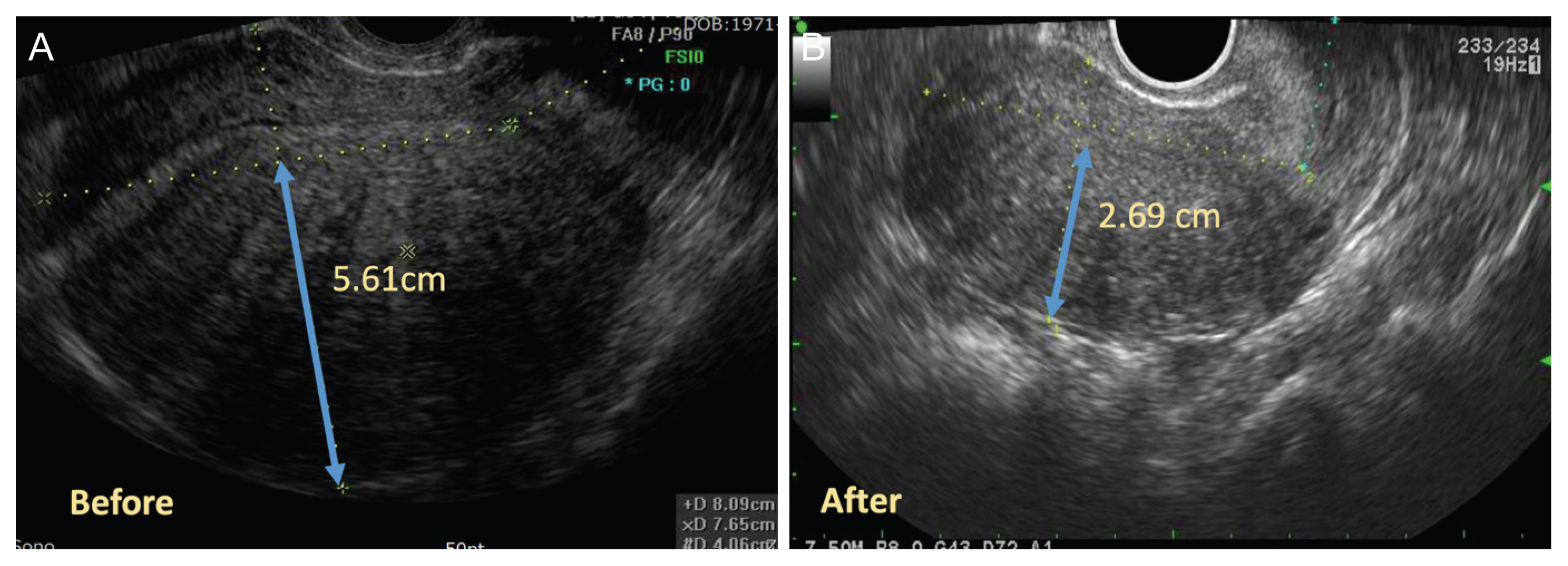
Results
The patient had no postoperative complications, and her pain was greatly improved. The CA125 level decreased from 434 U/mL to 45.99 U/mL, and the transvaginal ultrasound showed a reduction in posterior myometrial thickness from 5.61 cm to 2.69 cm.
Conclusion
This technique maintained the integrity of the endometrial cavity, posterior myometrial thickness, and uterine layer alignment. We believe that it is a feasible technique and may be a solution for adenomyosis in patients seeking for fertility preservation.
Keyword
Figure
Reference
-
References
1. Donnez J, Donnez O, Dolmans MM. Introduction: uterine adenomyosis, another enigmatic disease of our time. Fertil Steril. 2018; 109:369–70.2. Struble J, Reid S, Bedaiwy MA. Adenomyosis: a clinical review of a challenging gynecologic condition. J Minim Invasive Gynecol. 2016; 23:164–85.3. Leyendecker G, Kunz G, Kissler S, Wildt L. Adenomyosis and reproduction. Best Pract Res Clin Obstet Gynaecol. 2006; 20:523–46.
Article4. Thain S, Tan HH. Approaches to adenomyomectomy. Gynecol Minim Invasive Ther. 2015; 4:49–54.
Article5. Sinha R, Sanjay M, Rupa B, Kumari S. Robotic surgery in gynecology. J Minim Access Surg. 2015; 11:50–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Robot-Assisted Laparoscopic Adenomyomectomy for Patients Who Want to Preserve Fertility
- Transverse uterine incision closure: One versus Two layers
- Single-Layer vs. Double-Layer Donor Scalp Wound Closure in Strip Harvest
- Result of modified two-layer vasovasostomy and modified one-layer vasovasostomy using stent under microscope
- Reconstruction of Wide Palatal Defect Using Mucoperiosteal Hinge Flap and Pushback Palatoplasty