Healthc Inform Res.
2021 Apr;27(2):153-161. 10.4258/hir.2021.27.2.153.
Barriers in Health Information Systems and Technologies to Support Maternal and Neonatal Referrals at Primary Health Centers
- Affiliations
-
- 1Faculty of Computer Science, University of Indonesia, Depok, West Java, Indonesia
- KMID: 2515918
- DOI: http://doi.org/10.4258/hir.2021.27.2.153
Abstract
Objectives
This study explored health workers’ perceptions and experiences regarding the maternal and neonatal referral system, focusing on barriers of health information systems and technologies (IS/IT) at primary health centers (PHCs) in South Tangerang, Indonesia.
Methods
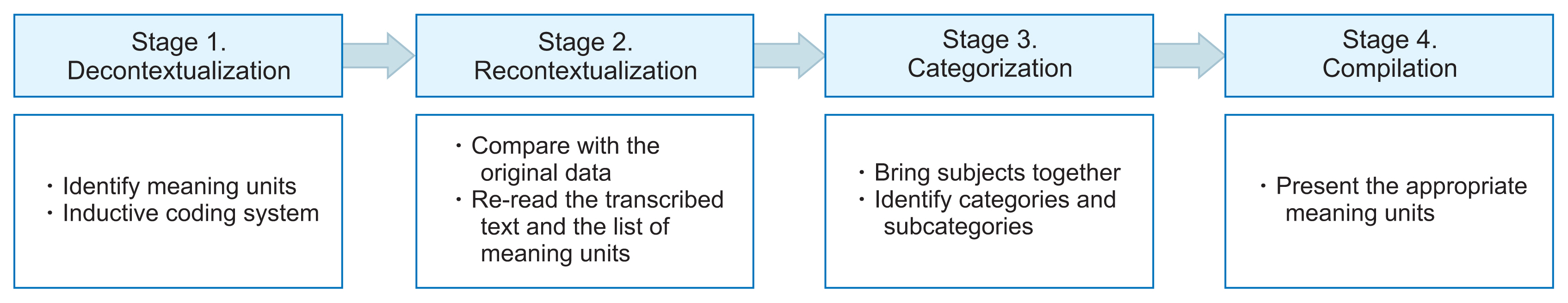
This qualitative study was conducted using semi-structured interviews, which were conducted at the South Tangerang District Health Office and three PHCs. Interviews were conducted with nine participants responsible for maternal and neonatal referrals in their organizations. The data were analyzed using qualitative content analysis.
Results
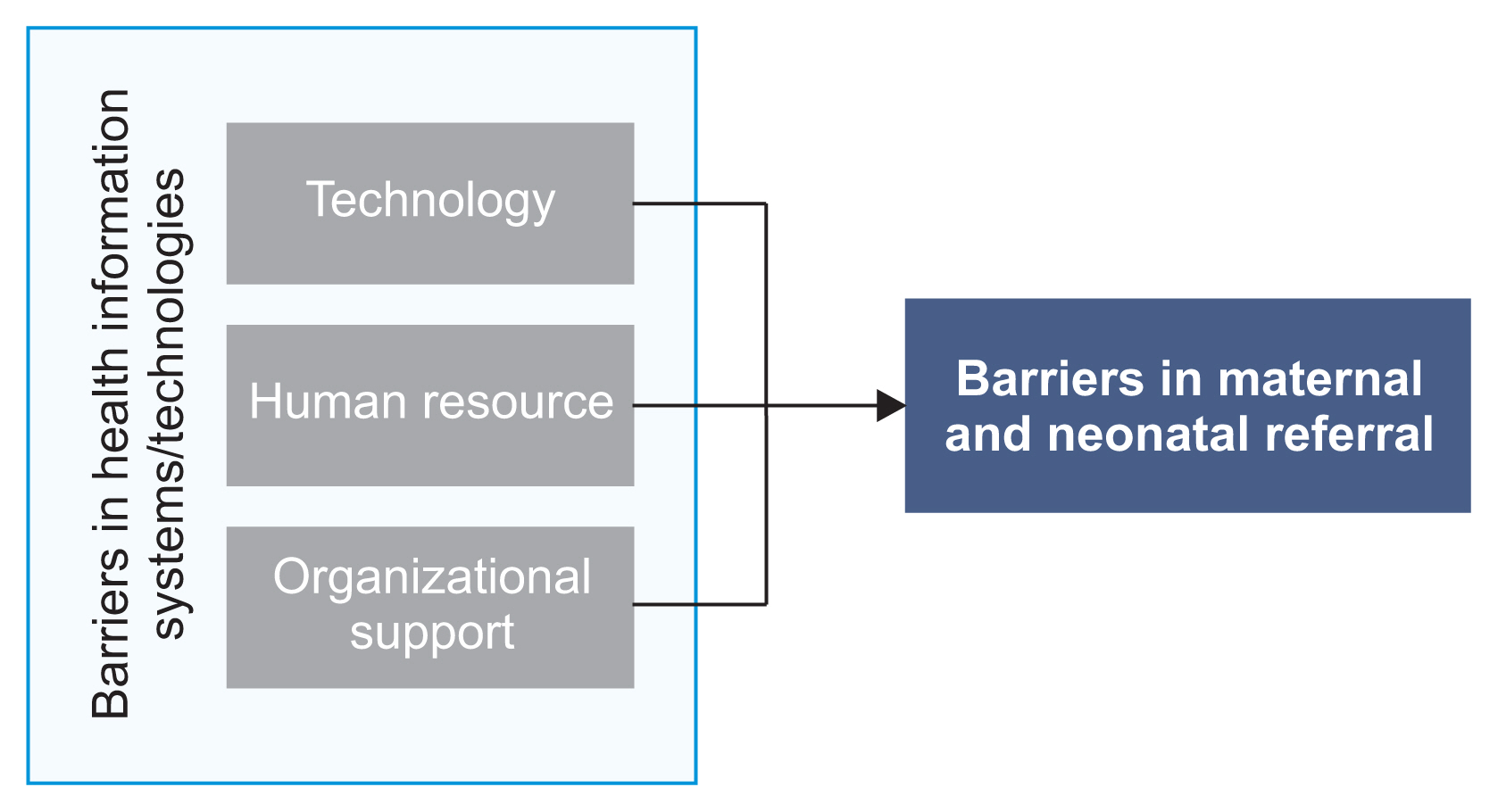
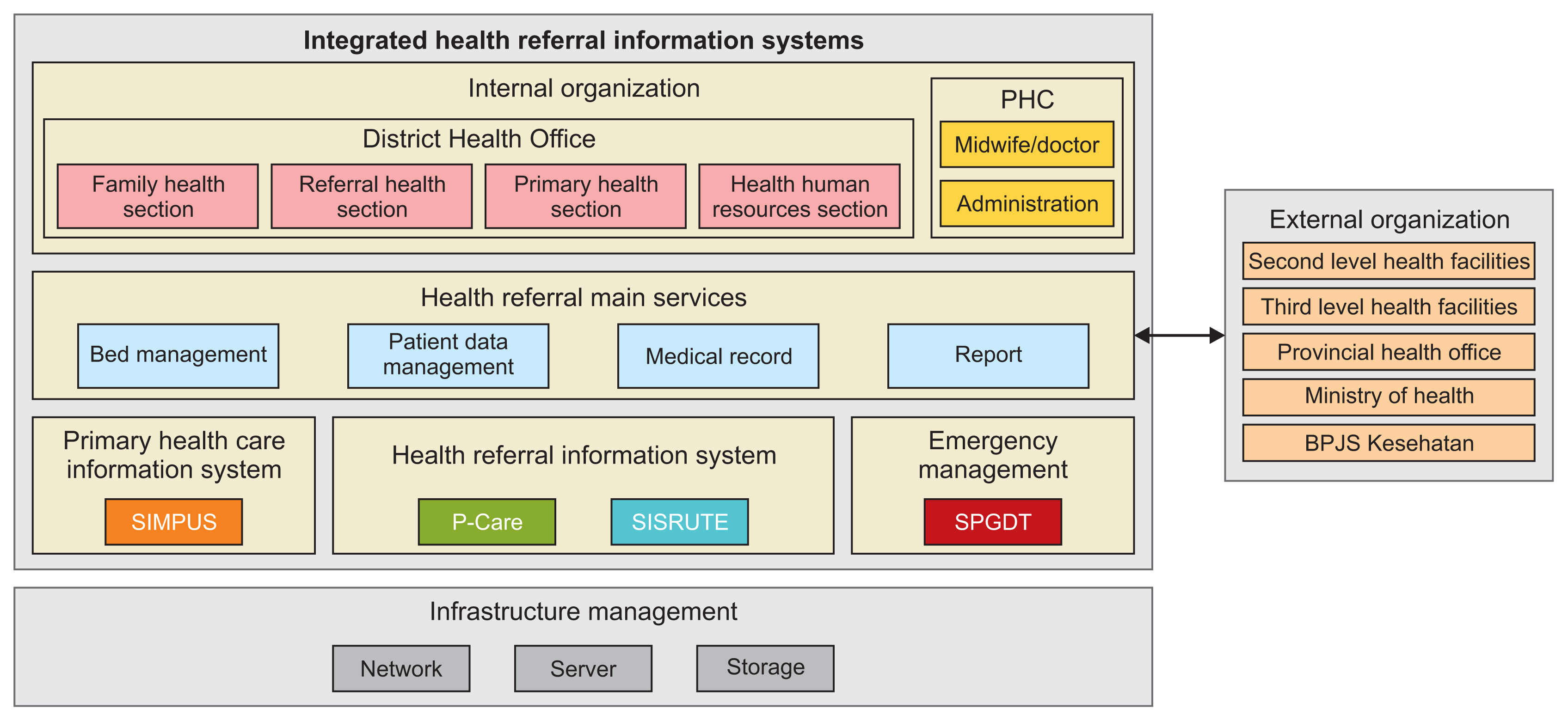
In South Tangerang, the Primary Health Care Information System (SIMPUS) is used to register patients and record data on medical treatment. To facilitate referrals, the PHCs currently use the Integrated Referral Information System (SISRUTE), P-Care, and the Integrated Emergency Management System (SPGDT). The following four IS/IT barriers to support maternal and neonatal referrals were found: technology, human resources, organizational support, and the referral process and implementation.
Conclusions
The barriers in technology, human resources, and organizational support cause problems in the maternal and neonatal referral process and in the implementation of referrals. Barriers to referrals can influence patients’ ability to receive appropriate care in a timely fashion and lead to inefficiency in maternal and neonatal referrals. This study contributes knowledge about IS/IT implementation in maternal and neonatal referral systems and provides recommendations to health regulators and application developers for the implementation of IS/IT in Indonesia.
Keyword
Figure
Reference
-
References
1. Murray SF, Pearson SC. Maternity referral systems in developing countries: current knowledge and future research needs. Soc Sci Med. 2006; 62(9):2205–15.
Article2. Harahap NC, Handayani PW, Hidayanto AN. Barriers and technologies of maternal and neonatal referral system in developing countries: a narrative review. Informatics in Medicine Unlocked. 2019; 15:100184.
Article3. Gance-Cleveland B, Leiferman J, Aldrich H, Nodine P, Anderson J, Nacht A, et al. Using the technology acceptance model to develop StartSmart: mHealth for screening, brief intervention, and referral for risk and protective factors in pregnancy. J Midwifery Womens Health. 2019; 64(5):630–40.4. Battle JD, Farrow L, Tibaijuka J, Mitchell M. mHealth for Safer Deliveries: a mixed methods evaluation of the effect of an integrated mobile health intervention on maternal care utilization. Healthc (Amst). 2015; 3(4):180–4.
Article5. Martinez B, Ixen EC, Hall-Clifford R, Juarez M, Miller AC, Francis A, et al. mHealth intervention to improve the continuum of maternal and perinatal care in rural Guatemala: a pragmatic, randomized controlled feasibility trial. Reprod Health. 2018; 15(1):120.
Article6. Walsham G. Health information systems in developing countries: some reflections on information for action. Inf Technol Dev. 2020; 26(1):194–200.
Article7. Jawhari B, Keenan L, Zakus D, Ludwick D, Isaac A, Saleh A, et al. Barriers and facilitators to Electronic Medical Record (EMR) use in an urban slum. Int J Med Inform. 2016; 94:246–54.
Article8. Sahay S, Nielsen P, Latifov M. Grand challenges of public health: How can health information systems support facing them? Health Policy Technol. 2018; 7(1):81–7.
Article9. Handayani PW, Pinem AA, Azzahro F, Hidayanto AN, Ayuningtyas D. The information system/information technology (IS/IT) practices in the Indonesia health referral system. Inform Med Unlocked. 2019; 17:100263.
Article10. Mahendradhata Y, Trisnantoro L, Listyadewi S, Soewondo P, Marthias T, Harimurti P, et al. The Republic of Indonesia health system review. Geneva, Switzerland: World Health Organization;2017.11. Jahn A, De Brouwere V. Referral in pregnancy and childbirth: concepts and strategies. Safe motherhood strategies: a review of the evidence. Stud HSO&P. 2001; 17:225–42.12. Minister of Health of the Republic of Indonesia. Workshop Integrasi SIKDA Generik versi 1.4 P-Care [Internet]. Jakarta, Indonesia: Minister of Health of the Republic of Indonesia;2017. [cited at 2021 Apr 10]. Available from: https://pusdatin.kemkes.go.id/article/view/17073100001/workshop-integrasi-sikda-generik-versi-1-4---p-care.html .13. Sofiah , Habsari SK, Sumardiyono . The effectiveness and perception of ICT program implementation in enhancing maternal and newborn survival among pregnant women in Indonesian society. In : Proceedings of the 3rd International Conference on Social and Political Science; 2016 Nov 2–3; Central Java, Indonesia. p. 160–9.14. Handayani PW, Pinem AA, Munajat Q, Azzahro F, Hidayanto AN, Ayuningtyas D, et al. Health referral enterprise architecture design in Indonesia. Healthc Inform Res. 2019; 25(1):3–11.
Article15. Minister of Health of the Republic of Indonesia. Regulation of the Minister of Health of the Republic of Indonesia Number 97 of 2014 concerning health services before pregnancy, pregnancy, childbirth, and postpartum, contraceptive services and sexual health services [Internet]. Jakarta, Indonesia: Minister of Health of the Republic of Indonesia;2014. [cited at 2021 Apr 10]. Available from: https://www.kebijakanaidsindonesia.net/id/dokumen-kebijakan?task=download.send&id=644&catid=17&m=0 .16. South Tangerang District Health Office [Internet]. Kota Tangerang Selatan, Indonesia: South Tangerang District Health Office;c2017. [cited at 2021 Apr 10]. Available from: https://dinkes.tangerangselatankota.go.id/ .17. Bengtsson M. How to plan and perform a qualitative study using content analysis. NursingPlus Open. 2016; 2:8–14.
Article18. Afrizal SH, Handayani PW, Hidayanto AN, Eryando T, Budiharsana M, Martha E. Barriers and challenges to Primary Health Care Information System (PHCIS) adoption from health management perspective: a qualitative study. Inform Med Unlocked. 2019; 17:100198.
Article19. Minister of Health of the Republic of Indonesia. Implementasi E-Health di Indonesia [Internet]. Jakarta, Indonesia: Minister of Health of the Republic of Indonesia;2017. [cited at 2021 Apr 10]. Available from: https://web.persi.or.id/images/2017/pengurus-harian/implementasi_ehealth.pdf .20. Seniwati E. Pcare BPJS Kesehatan untuk Faskes Pertama (Klinik, Puskesmas, Dokter) [Internet]. Jakarta, Indonesia: BPJS Kesehatan;2019. [cited at 2021 Apr 10]. Available from: https://www.panduanbpjs.com/pcare-bpjs-untuk-faskes/ .21. Minister of Health of the Republic of Indonesia. Regulation of the Minister of Health of the Republic of Indonesia Number 19 of 2016 concerning an integrated emergency response system [Internet]. Jakarta, Indonesia: Minister of Health of the Republic of Indonesia;2016. [cited at 2021 Apr 10]. Available from: https://peraturan.go.id/peraturan/view.html?id=11e6b62f8f2449608185313233303036 .22. Handayani PW, Saladdin IR, Pinem AA, Azzahro F, Hidayanto AN, Ayuningtyas D. Health referral system user acceptance model in Indonesia. Heliyon. 2018; 4(12):e01048.
Article23. World Health Organization. Standards for improving quality of maternal and newborn care in health facilities [Internet]. Geneva, Switzerland: World Health Organization;2016. [cited at 2021 Apr 10]. Available from: https://apps.who.int/iris/bitstream/handle/10665/249155/9789241511216-eng.pdf?sequence=1 .24. Sutiono AB, Qiantori A, Prasetio S, Santoso H, Suwa H, et al. Designing an emergency medical information system for the early stages of disasters in developing countries: the human interface advantage, simplicity and efficiency. J Med Syst. 2010; 34(4):667–75.
Article25. Wahid F, Dirgahayu RT, Hamzah A, Setiaji H. When more is less: the case of disconnected information systems in Indonesian public health facilities. IOP Conf Ser Mater Sci Eng. 2018; 325:012017.
Article26. World Health Organization. Framework and standards for country health information systems. 2nd ed. Geneva, Switzerland: World Health Organization;2008.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ubiquitous Health in Korea: Progress, Barriers, and Prospects
- Geographical Information Systems and Health: Current State and Future Directions
- Wearable Sensors in Healthcare and Sensor-Enhanced Health Information Systems: All Our Tomorrows?
- Development of a Drug Management Performance Application: A Needs Assessment in Indonesia
- Health Referral Enterprise Architecture Design in Indonesia