Clin Exp Otorhinolaryngol.
2021 May;14(2):159-168. 10.21053/ceo.2020.00465.
Pepsin and Laryngeal and Hypopharyngeal Carcinomas
- Affiliations
-
- 1Department of Otolaryngology, The First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, China
- 2Department of Otolaryngology, The First People’s Hospital of Huzhou City, Zhejiang, China
- KMID: 2515428
- DOI: http://doi.org/10.21053/ceo.2020.00465
Abstract
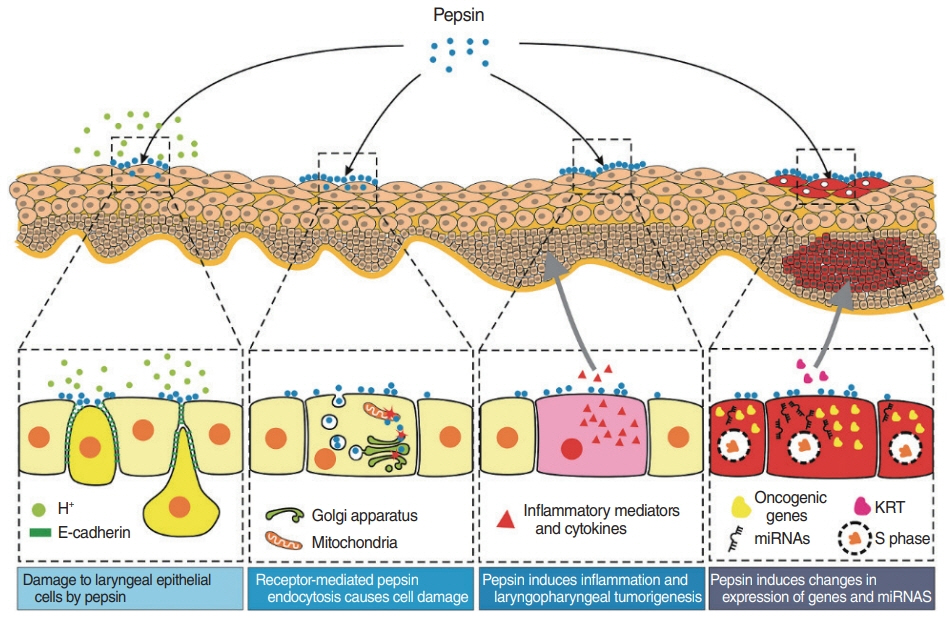
- Laryngeal and hypopharyngeal carcinomas are common malignant tumors of the head and neck, and the incidence of both is increasing. Laryngopharyngeal reflux refers to the retrograde flow of gastric contents into the larynx, oropharynx, and/or nasopharynx. It remains controversial whether laryngopharyngeal reflux is a risk factor for laryngeal and hypopharyngeal cancers. The refluxing substances mainly include hydrochloric acid, pepsin, and occasionally bile acids and bile salts, as well as bacteria that colonize the gastrointestinal tract. Loss of epithelium in the mucous membrane of the larynx and hypopharynx is thought to be caused by pepsin. Here, we review the relationships between laryngopharyngeal reflux and both laryngeal and hypopharyngeal carcinomas, as well as the significance of pepsin, methods of clinical detection, and the mechanism of carcinogenesis.
Figure
Reference
-
1. Bates JE, Morris CG, Hitchcock KE, Dziegielewski PT, Mendenhall WM, Amdur RJ. Locally advanced hypopharyngeal and laryngeal cancer: influence of HPV status. Radiother Oncol. 2019; Nov. 140:6–9.
Article2. Acuna G, Goma M, Temprana-Salvador J, Garcia-Bragado F, Alos L, Ordi J, et al. Human papillomavirus in laryngeal and hypopharyngeal lymphoepithelial carcinoma. Mod Pathol. 2019; May. 32(5):621–6.
Article3. Du E, Mazul AL, Farquhar D, Brennan P, Anantharaman D, AbediArdekani B, et al. Long-term survival in head and neck cancer: impact of site, stage, smoking, and human papillomavirus status. Laryngoscope. 2019; Nov. 129(11):2506–13.
Article4. Marur S, Forastiere AA. Head and neck squamous cell carcinoma: update on epidemiology, diagnosis, and treatment. Mayo Clin Proc. 2016; Mar. 91(3):386–96.
Article5. Alam MS, Siddiqui SA, Perween R. Epidemiological profile of head and neck cancer patients in Western Uttar Pradesh and analysis of distributions of risk factors in relation to site of tumor. J Cancer Res Ther. 2017; Jul-Sep. 13(3):430–5.
Article6. Faggons CE, Mabedi C, Shores CG, Gopal S. Review: head and neck squamous cell carcinoma in sub-Saharan Africa. Malawi Med J. 2015; Sep. 27(3):79–87.
Article7. Rooper LM, Windon MJ, Hernandez T, Miles B, Ha PK, Ryan WR, et al. HPV-positive squamous cell carcinoma of the larynx, oral cavity, and hypopharynx: clinicopathologic characterization with recognition of a novel warty variant. Am J Surg Pathol. 2020; May. 44(5):691–702.8. Nurgalieva ZZ, Graham DY, Dahlstrom KR, Wei Q, Sturgis EM. A pilot study of Helicobacter pylori infection and risk of laryngopharyngeal cancer. Head Neck. 2005; Jan. 27(1):22–7.9. Lechien JR, Saussez S, Harmegnies B, Finck C, Burns JA. Laryngopharyngeal reflux and voice disorders: a multifactorial model of etiology and pathophysiology. J Voice. 2017; Nov. 31(6):733–52.
Article10. Wilson JA. What is the evidence that gastroesophageal reflux is involved in the etiology of laryngeal cancer. Curr Opin Otolaryngol Head Neck Surg. 2005; Apr. 13(2):97–100.
Article11. Shimazu R, Kuratomi Y, Aoki S, Inokuchi A. Laryngeal granuloma in experimental rats with gastroesophageal reflux disease and mechanically injured vocal cord mucosa. Ann Otol Rhinol Laryngol. 2014; Apr. 123(4):247–51.
Article12. Sasaki CT, Issaeva N, Vageli DP. In vitro model for gastroduodenal reflux-induced nuclear factor-kappaB activation and its role in hypopharyngeal carcinogenesis. Head Neck. 2016; Apr. 38 Suppl 1:E1381–91.
Article13. Gtari W, Bey H, Aschi A, Bitri L, Othman T. Impact of macromolecular crowding on structure and properties of pepsin and trypsin. Mater Sci Eng C Mater Biol Appl. 2017; Mar. 72:98–105.
Article14. Wight R, Paleri V, Arullendran P. Current theories for the development of nonsmoking and nondrinking laryngeal carcinoma. Curr Opin Otolaryngol Head Neck Surg. 2003; Apr. 11(2):73–7.
Article15. Copper MP, Smit CF, Stanojcic LD, Devriese PP, Schouwenburg PF, Mathus-Vliegen LM. High incidence of laryngopharyngeal reflux in patients with head and neck cancer. Laryngoscope. 2000; Jun. 110(6):1007–11.
Article16. Galli J, Cammarota G, Calo L, Agostino S, D’Ugo D, Cianci R, et al. The role of acid and alkaline reflux in laryngeal squamous cell carcinoma. Laryngoscope. 2002; Oct. 112(10):1861–5.
Article17. Tan JJ, Wang L, Mo TT, Wang J, Wang MG, Li XP. Pepsin promotes IL-8 signaling-induced epithelial-mesenchymal transition in laryngeal carcinoma. Cancer Cell Int. 2019; Mar. 19:64.
Article18. Anis MM, Razavi MM, Xiao X, Soliman AM. Association of gastroesophageal reflux disease and laryngeal cancer. World J Otorhinolaryngol Head Neck Surg. 2018; Apr. 4(4):278–81.
Article19. Riley CA, Marino MJ, Hsieh MC, Wu EL, Wu XC, McCoul ED. Detection of laryngeal carcinoma in the U.S. elderly population with gastroesophageal reflux disease. Head Neck. 2019; May. 41(5):1434–40.
Article20. Parsel SM, Wu EL, Riley CA, McCoul ED. Gastroesophageal and laryngopharyngeal reflux associated with laryngeal malignancy: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2019; Jun. 17(7):1253–64.21. Busch EL, Zevallos JP, Olshan AF. Gastroesophageal reflux disease and odds of head and neck squamous cell carcinoma in North Carolina. Laryngoscope. 2016; May. 126(5):1091–6.
Article22. LeBlanc B, Lewis E, Caldito G, Nathan CA. Increased pharyngeal reflux in patients treated for laryngeal cancer: a pilot study. Otolaryngol Head Neck Surg. 2015; Nov. 153(5):791–4.23. Sereg-Bahar M, Jerin A, Hocevar-Boltezar I. Higher levels of total pepsin and bile acids in the saliva as a possible risk factor for early laryngeal cancer. Radiol Oncol. 2015; Mar. 49(1):59–64.
Article24. Zhang D, Zhou J, Chen B, Zhou L, Tao L. Gastroesophageal reflux and carcinoma of larynx or pharynx: a meta-analysis. Acta Otolaryngol. 2014; Oct. 134(10):982–9.
Article25. Coca-Pelaz A, Rodrigo JP, Takes RP, Silver CE, Paccagnella D, Rinaldo A, et al. Relationship between reflux and laryngeal cancer. Head Neck. 2013; Dec. 35(12):1814–8.
Article26. Langevin SM, Michaud DS, Marsit CJ, Nelson HH, Birnbaum AE, Eliot M, et al. Gastric reflux is an independent risk factor for laryngopharyngeal carcinoma. Cancer Epidemiol Biomarkers Prev. 2013; Jun. 22(6):1061–8.
Article27. Tae K, Jin BJ, Ji YB, Jeong JH, Cho SH, Lee SH. The role of laryngopharyngeal reflux as a risk factor in laryngeal cancer: a preliminary report. Clin Exp Otorhinolaryngol. 2011; Jun. 4(2):101–4.
Article28. Basseri B, Conklin JL, Mertens RB, Lo SK, Bellack GS, Shaye OA. Heterotopic gastric mucosa (inlet patch) in a patient with laryngopharyngeal reflux (LPR) and laryngeal carcinoma: a case report and review of literature. Dis Esophagus. 2009; 22(4):E1–5.
Article29. Ozlugedik S, Yorulmaz I, Gokcan K. Is laryngopharyngeal reflux an important risk factor in the development of laryngeal carcinoma. Eur Arch Otorhinolaryngol. 2006; Apr. 263(4):339–43.
Article30. Geterud A, Bove M, Ruth M. Hypopharyngeal acid exposure: an independent risk factor for laryngeal cancer. Laryngoscope. 2003; Dec. 113(12):2201–5.
Article31. Nilsson M, Chow WH, Lindblad M, Ye W. No association between gastroesophageal reflux and cancers of the larynx and pharynx. Cancer Epidemiol Biomarkers Prev. 2005; May. 14(5):1194–7.
Article32. Smit CF, Copper MP, van Leeuwen JA, Schoots IG, Stanojcic LD. Effect of cigarette smoking on gastropharyngeal and gastroesophageal reflux. Ann Otol Rhinol Laryngol. 2001; Feb. 110(2):190–3.
Article33. Francis DO, Maynard C, Weymuller EA, Reiber G, Merati AL, Yueh B. Reevaluation of gastroesophageal reflux disease as a risk factor for laryngeal cancer. Laryngoscope. 2011; Jan. 121(1):102–5.
Article34. Qadeer MA, Colabianchi N, Strome M, Vaezi MF. Gastroesophageal reflux and laryngeal cancer: causation or association? A critical review. Am J Otolaryngol. 2006; Mar-Apr. 27(2):119–28.
Article35. El-Serag HB, Hepworth EJ, Lee P, Sonnenberg A. Gastroesophageal reflux disease is a risk factor for laryngeal and pharyngeal cancer. Am J Gastroenterol. 2001; Jul. 96(7):2013–8.
Article36. Kim SY, Park B, Lim H, Kim M, Kong IG, Choi HG. Increased risk of larynx cancer in patients with gastroesophageal reflux disease from a national sample cohort. Clin Otolaryngol. 2019; Jul. 44(4):534–40.
Article37. Best AR, Halum SL, Parker NP. Current indications for transnasal esophagoscopy: an american broncho-esophagological association survey. Ann Otol Rhinol Laryngol. 2018; Dec. 127(12):926–30.
Article38. Chung EJ, Rho YS, Jung KY, Kim JW, Lee SW. The role of transnasal esophagoscopy in ENT office: a prospective, multicenter study in Korea. Clin Exp Otorhinolaryngol. 2014; Jun. 7(2):123–5.
Article39. Velanovich V. Endoscopic, endoluminal fundoplication for gastroesophageal reflux disease: initial experience and lessons learned. Surgery. 2010; Oct. 148(4):646–53.
Article40. Doustmohammadian N, Naderpour M, Khoshbaten M, Doustmohammadian A. Is there any association between esophagogastric endoscopic findings and laryngeal cancer. Am J Otolaryngol. 2011; Nov-Dec. 32(6):490–3.
Article41. Maldhure S, Chandrasekharan R, Dutta AK, Chacko A, Kurien M. Role of PH monitoring in laryngopharyngeal reflux patients with voice disorders. Iran J Otorhinolaryngol. 2016; Nov. 28(89):377–83.42. Mosli M, Alkhathlan B, Abumohssin A, Merdad M, Alherabi A, Marglani O, et al. Prevalence and clinical predictors of LPR among patients diagnosed with GERD according to the reflux symptom index questionnaire. Saudi J Gastroenterol. 2018; Jul-Aug. 24(4):236–41.
Article43. Lechien JR, Bobin F, Muls V, Thill MP, Horoi M, Ostermann K, et al. Validity and reliability of the reflux symptom score. Laryngoscope. 2020; Mar. 130(3):E98–107.
Article44. Lechien JR, Rodriguez Ruiz A, Dequanter D, Bobin F, Mouawad F, Muls V, et al. Validity and reliability of the reflux sign assessment. Ann Otol Rhinol Laryngol. 2020; Apr. 129(4):313–25.
Article45. Lechien JR, Akst LM, Hamdan AL, Schindler A, Karkos PD, Barillari MR, et al. Evaluation and management of laryngopharyngeal reflux disease: state of the art review. Otolaryngol Head Neck Surg. 2019; May. 160(5):762–82.
Article46. Hammer HF. Reflux-associated laryngitis and laryngopharyngeal reflux: a gastroenterologist’s point of view. Dig Dis. 2009; 27(1):14–7.47. Ford CN. Evaluation and management of laryngopharyngeal reflux. JAMA. 2005; Sep. 294(12):1534–40.
Article48. Hanson DG, Conley D, Jiang J, Kahrilas P. Role of esophageal pH recording in management of chronic laryngitis: an overview. Ann Otol Rhinol Laryngol Suppl. 2000; Oct. 184:4–9.
Article49. Postma GN. Ambulatory pH monitoring methodology. Ann Otol Rhinol Laryngol Suppl. 2000; Oct. 184:10–4.
Article50. Hayat JO, Gabieta-Somnez S, Yazaki E, Kang JY, Woodcock A, Dettmar P, et al. Pepsin in saliva for the diagnosis of gastro-oesophageal reflux disease. Gut. 2015; Mar. 64(3):373–80.
Article51. Na SY, Kwon OE, Lee YC, Eun YG. Optimal timing of saliva collection to detect pepsin in patients with laryngopharyngeal reflux. Laryngoscope. 2016; Dec. 126(12):2770–3.
Article52. Johnston N, Yan JC, Hoekzema CR, Samuels TL, Stoner GD, Blumin JH, et al. Pepsin promotes proliferation of laryngeal and pharyngeal epithelial cells. Laryngoscope. 2012; Jun. 122(6):1317–25.
Article53. Dy F, Amirault J, Mitchell PD, Rosen R. Salivary pepsin lacks sensitivity as a diagnostic tool to evaluate extraesophageal reflux disease. J Pediatr. 2016; Oct. 177:53–8.
Article54. Hayat JO, Yazaki E, Moore AT, Hicklin L, Dettmar P, Kang JY, et al. Objective detection of esophagopharyngeal reflux in patients with hoarseness and endoscopic signs of laryngeal inflammation. J Clin Gastroenterol. 2014; Apr. 48(4):318–27.
Article55. Yadlapati R, Adkins C, Jaiyeola DM, Lidder AK, Gawron AJ, Tan BK, et al. Abilities of oropharyngeal pH tests and salivary pepsin analysis to discriminate between asymptomatic volunteers and subjects with symptoms of laryngeal irritation. Clin Gastroenterol Hepatol. 2016; Apr. 14(4):535–42.
Article56. Raja Nhari RM, Muhammad Zailani AN, Khairil Mokhtar NF, Hanish I. Detection of porcine pepsin in model cheese using polyclonal antibody-based ELISA. Food Addit Contam Part A Chem Anal Control Expo Risk Assess. 2020; Apr. 37(4):561–7.
Article57. Ju H, Liu X, Zhang G, Liu D, Yang Y. Comparison of the structural characteristics of native collagen fibrils derived from bovine tendons using two different methods: modified acid-solubilized and pepsin-aided extraction. Materials (Basel). 2020; Jan. 13(2):358.
Article58. Fortunato JE, D’Agostino RB Jr, Lively MO. Pepsin in saliva as a biomarker for oropharyngeal reflux compared with 24-hour esophageal impedance/pH monitoring in pediatric patients. Neurogastroenterol Motil. 2017; Feb. 29(2):e12936.
Article59. Lee YJ, Kwon J, Shin S, Eun YG, Shin JH, Lee GJ. Optimization of saliva collection and immunochromatographic detection of salivary pepsin for point-of-care testing of laryngopharyngeal reflux. Sensors (Basel). 2020; Jan. 20(1):325.
Article60. Sereg-Bahar M, Jerin A, Jansa R, Stabuc B, Hocevar-Boltezar I. Pepsin and bile acids in saliva in patients with laryngopharyngeal reflux: a prospective comparative study. Clin Otolaryngol. 2015; Jun. 40(3):234–9.61. Guo Z, Wu H, Jiang J, Zhang C. Pepsin in saliva as a diagnostic marker for gastroesophageal reflux disease: a meta-analysis. Med Sci Monit. 2018; Dec. 24:9509–16.
Article62. Du X, Wang F, Hu Z, Wu J, Wang Z, Yan C, et al. The diagnostic value of pepsin detection in saliva for gastro-esophageal reflux disease: a preliminary study from China. BMC Gastroenterol. 2017; Oct. 17(1):107.
Article63. Formanek M, Jancatova D, Kominek P, Tomanova R, Zelenik K. Comparison of impedance and pepsin detection in the laryngeal mucosa to determine impedance values that indicate pathological laryngopharyngeal reflux. Clin Transl Gastroenterol. 2017; Oct. 8(10):e123.64. Jiang A, Liang M, Su Z, Chai L, Lei W, Wang Z, et al. Immunohistochemical detection of pepsin in laryngeal mucosa for diagnosing laryngopharyngeal reflux. Laryngoscope. 2011; Jul. 121(7):1426–30.
Article65. Johnston N, Knight J, Dettmar PW, Lively MO, Koufman J. Pepsin and carbonic anhydrase isoenzyme III as diagnostic markers for laryngopharyngeal reflux disease. Laryngoscope. 2004; Dec. 114(12):2129–34.
Article66. Komatsu Y, Kelly LA, Zaidi AH, Rotoloni CL, Kosovec JE, Lloyd EJ, et al. Hypopharyngeal pepsin and Sep70 as diagnostic markers of laryngopharyngeal reflux: preliminary study. Surg Endosc. 2015; May. 29(5):1080–7.
Article67. Saritas Yuksel E, Hong SK, Strugala V, Slaughter JC, Goutte M, Garrett CG, et al. Rapid salivary pepsin test: blinded assessment of test performance in gastroesophageal reflux disease. Laryngoscope. 2012; Jun. 122(6):1312–6.
Article68. Knight J, Lively MO, Johnston N, Dettmar PW, Koufman JA. Sensitive pepsin immunoassay for detection of laryngopharyngeal reflux. Laryngoscope. 2005; Aug. 115(8):1473–8.
Article69. Niu K, Guo C, Teng S, Zhou D, Yu S, Yin W, et al. Pepsin promotes laryngopharyngeal neoplasia by modulating signaling pathways to induce cell proliferation. PLoS One. 2020; Jan. 15(1):e0227408.
Article70. Sasaki CT, Doukas SG, Costa J, Vageli DP. Biliary reflux as a causal factor in hypopharyngeal carcinoma: new clinical evidence and implications. Cancer. 2019; Oct. 125(20):3554–65.
Article71. Doukas SG, Cardoso B, Tower JI, Vageli DP, Sasaki CT. Biliary tumorigenic effect on hypopharyngeal cells is significantly enhanced by pH reduction. Cancer Med. 2019; Aug. 8(9):4417–27.72. Koufman JA. The otolaryngologic manifestations of gastroesophageal reflux disease (GERD): a clinical investigation of 225 patients using ambulatory 24-hour pH monitoring and an experimental investigation of the role of acid and pepsin in the development of laryngeal injury. Laryngoscope. 1991; Apr. 101(4 Pt 2 Suppl 53):1–78.73. Sharma N, Agrawal A, Freeman J, Vela MF, Castell D. An analysis of persistent symptoms in acid-suppressed patients undergoing impedance-pH monitoring. Clin Gastroenterol Hepatol. 2008; May. 6(5):521–4.
Article74. Koufman JA. Laryngopharyngeal reflux is different from classic gastroesophageal reflux disease. Ear Nose Throat J. 2002; Sep. 81(9 Suppl 2):7–9.75. Piper DW, Fenton BH. pH stability and activity curves of pepsin with special reference to their clinical importance. Gut. 1965; Oct. 6(5):506–8.
Article76. Tutuian R, Vela MF, Hill EG, Mainie I, Agrawal A, Castell DO. Characteristics of symptomatic reflux episodes on acid suppressive therapy. Am J Gastroenterol. 2008; May. 103(5):1090–6.
Article77. Poelmans J, Tack J, Feenstra L. Paroxysmal laryngospasm: a typical but underrecognized supraesophageal manifestation of gastroesophageal reflux. Dig Dis Sci. 2004; Nov-Dec. 49(11-12):1868–74.
Article78. Sifrim D, Mittal R, Fass R, Smout A, Castell D, Tack J, et al. Review article: acidity and volume of the refluxate in the genesis of gastrooesophageal reflux disease symptoms. Aliment Pharmacol Ther. 2007; May. 25(9):1003–17.
Article79. Alimperti S, Andreadis ST. CDH2 and CDH11 act as regulators of stem cell fate decisions. Stem Cell Res. 2015; May. 14(3):270–82.
Article80. Reichel O, Mayr D, Durst F, Berghaus A. E-cadherin but not betacatenin expression is decreased in laryngeal biopsies from patients with laryngopharyngeal reflux. Eur Arch Otorhinolaryngol. 2008; Aug. 265(8):937–42.81. Galera-Ruiz H, Rios-Moreno MJ, Gonzalez-Campora R, Ortega I, Fernandez A, Garcia-Escudero A, et al. The cadherin-catenin complex in laryngeal squamous cell carcinoma. Eur Arch Otorhinolaryngol. 2012; Apr. 269(4):1183–8.
Article82. Takeichi M. Cadherins in cancer: implications for invasion and metastasis. Curr Opin Cell Biol. 1993; Oct. 5(5):806–11.
Article83. Johnston N, Dettmar PW, Lively MO, Postma GN, Belafsky PC, Birchall M, et al. Effect of pepsin on laryngeal stress protein (Sep70, Sep53, and Hsp70) response: role in laryngopharyngeal reflux disease. Ann Otol Rhinol Laryngol. 2006; Jan. 115(1):47–58.
Article84. Johnston N, Bulmer D, Gill GA, Panetti M, Ross PE, Pearson JP, et al. Cell biology of laryngeal epithelial defenses in health and disease: further studies. Ann Otol Rhinol Laryngol. 2003; Jun. 112(6):481–91.
Article85. Samuels TL, Handler E, Syring ML, Pajewski NM, Blumin JH, Kerschner JE, et al. Mucin gene expression in human laryngeal epithelia: effect of laryngopharyngeal reflux. Ann Otol Rhinol Laryngol. 2008; Sep. 117(9):688–95.
Article86. Forero-Quintero LS, Ames S, Schneider HP, Thyssen A, Boone CD, Andring JT, et al. Membrane-anchored carbonic anhydrase IV interacts with monocarboxylate transporters via their chaperones CD147 and GP70. J Biol Chem. 2019; Jan. 294(2):593–607.
Article87. Mikulski RL, Silverman DN. Proton transfer in catalysis and the role of proton shuttles in carbonic anhydrase. Biochim Biophys Acta. 2010; Feb. 1804(2):422–6.
Article88. Tashian RE. The carbonic anhydrases: widening perspectives on their evolution, expression and function. Bioessays. 1989; Jun. 10(6):186–92.
Article89. Belafsky PC, Rees CJ. Laryngopharyngeal reflux: the value of otolaryngology examination. Curr Gastroenterol Rep. 2008; Jun. 10(3):278–82.
Article90. Kannan KK, Ramanadham M, Jones TA. Structure, refinement, and function of carbonic anhydrase isozymes: refinement of human carbonic anhydrase I. Ann N Y Acad Sci. 1984; 429:49–60.
Article91. Monti DM, De Simone G, Langella E, Supuran CT, Di Fiore A, Monti SM. Insights into the role of reactive sulfhydryl groups of Carbonic Anhydrase III and VII during oxidative damage. J Enzyme Inhib Med Chem. 2017; Dec. 32(1):5–12.92. Welch WJ, Brown CR. Influence of molecular and chemical chaperones on protein folding. Cell Stress Chaperones. 1996; Jun. 1(2):109–15.
Article93. Wu K, Stull F, Lee C, Bardwell JC. Protein folding while chaperone bound is dependent on weak interactions. Nat Commun. 2019; Oct. 10(1):4833.
Article94. Freilich R, Arhar T, Abrams JL, Gestwicki JE. Protein-protein interactions in the molecular chaperone network. Acc Chem Res. 2018; Apr. 51(4):940–9.
Article95. Johnston N, Wells CW, Samuels TL, Blumin JH. Rationale for targeting pepsin in the treatment of reflux disease. Ann Otol Rhinol Laryngol. 2010; Aug. 119(8):547–58.
Article96. Johnston N, Wells CW, Blumin JH, Toohill RJ, Merati AL. Receptormediated uptake of pepsin by laryngeal epithelial cells. Ann Otol Rhinol Laryngol. 2007; Dec. 116(12):934–8.
Article97. Samuels TL, Johnston N. Pepsin as a causal agent of inflammation during nonacidic reflux. Otolaryngol Head Neck Surg. 2009; Nov. 141(5):559–63.
Article98. Samuels TL, Altman KW, Gould JC, Kindel T, Bosler M, MacKinnon A, et al. Esophageal pepsin and proton pump synthesis in barrett’s esophagus and esophageal adenocarcinoma. Laryngoscope. 2019; Dec. 129(12):2687–95.
Article99. Wood JM, Hussey DJ, Woods CM, Astill D, Watson DI, Lee B, et al. Does gene expression in laryngeal subsites differ between patients with laryngopharyngeal reflux and controls. Clin Otolaryngol. 2018; Feb. 43(1):158–63.
Article100. Van Roon AH, Mayne GC, Wijnhoven BP, Watson DI, Leong MP, Neijman GE, et al. Impact of gastro-esophageal reflux on mucin mRNA expression in the esophageal mucosa. J Gastrointest Surg. 2008; Aug. 12(8):1331–40.
Article101. Zhang F, Cao H. MicroRNA-143-3p suppresses cell growth and invasion in laryngeal squamous cell carcinoma via targeting the k-Ras/ Raf/MEK/ERK signaling pathway. Int J Oncol. 2019; Feb. 54(2):689–701.102. Nath K, Reyaldeen R, Palamuthusingam D. Proton-pump inhibitor overuse: a cautionary tale in misguided benefit. Intern Med J. 2019; Oct. 49(10):1337.
Article103. Delshad SD, Almario CV, Chey WD, Spiegel BM. Prevalence of gastroesophageal reflux disease and proton pump inhibitor-refractory symptoms. Gastroenterology. 2020; Apr. 158(5):1250–61.
Article104. Eherer AJ, Habermann W, Hammer HF, Kiesler K, Friedrich G, Krejs GJ. Effect of pantoprazole on the course of reflux-associated laryngitis: a placebo-controlled double-blind crossover study. Scand J Gastroenterol. 2003; May. 38(5):462–7.
Article105. Noordzij JP, Khidr A, Evans BA, Desper E, Mittal RK, Reibel JF, et al. Evaluation of omeprazole in the treatment of reflux laryngitis: a prospective, placebo-controlled, randomized, double-blind study. Laryngoscope. 2001; Dec. 111(12):2147–51.
Article106. El-Serag HB, Lee P, Buchner A, Inadomi JM, Gavin M, McCarthy DM. Lansoprazole treatment of patients with chronic idiopathic laryngitis: a placebo-controlled trial. Am J Gastroenterol. 2001; Apr. 96(4):979–83.
Article107. Hu Q, Sun TT, Hong J, Fang JY, Xiong H, Meltzer SJ. Proton pump inhibitors do not reduce the risk of esophageal adenocarcinoma in patients with Barrett’s esophagus: a systematic review and meta-analysis. PLoS One. 2017; Jan. 12(1):e0169691.
Article108. Samuels T, Hoekzema C, Gould J, Goldblatt M, Frelich M, Bosler M, et al. Local synthesis of pepsin in Barrett’s esophagus and the role of pepsin in esophageal adenocarcinoma. Ann Otol Rhinol Laryngol. 2015; Nov. 124(11):893–902.
Article109. Hvid-Jensen F, Pedersen L, Funch-Jensen P, Drewes AM. Proton pump inhibitor use may not prevent high-grade dysplasia and oesophageal adenocarcinoma in Barrett’s oesophagus: a nationwide study of 9883 patients. Aliment Pharmacol Ther. 2014; May. 39(9):984–91.
Article110. Nason KS, Wichienkuer PP, Awais O, Schuchert MJ, Luketich JD, O’Rourke RW, et al. Gastroesophageal reflux disease symptom severity, proton pump inhibitor use, and esophageal carcinogenesis. Arch Surg. 2011; Jul. 146(7):851–8.
Article111. Lao-Sirieix P, Roy A, Worrall C, Vowler SL, Gardiner S, Fitzgerald RC. Effect of acid suppression on molecular predictors for esophageal cancer. Cancer Epidemiol Biomarkers Prev. 2006; Feb. 15(2):288–93.
Article112. Ten Kate RW, Tuynman HA, Festen HP, Pals G, Meuwissen SG. Effect of high dose omeprazole on gastric pepsin secretion and serum pepsinogen levels in man. Eur J Clin Pharmacol. 1988; 35(2):173–6.
Article113. Hurley BP, Jugo RH, Snow RF, Samuels TL, Yonker LM, Mou H, et al. Pepsin triggers neutrophil migration across acid damaged lung epithelium. Sci Rep. 2019; Sep. 9(1):13778.
Article114. Walentek P, Beyer T, Hagenlocher C, Muller C, Feistel K, Schweickert A, et al. ATP4a is required for development and function of the Xenopus mucociliary epidermis: a potential model to study proton pump inhibitor-associated pneumonia. Dev Biol. 2015; Dec. 408(2):292–304.115. Johnston N, Dettmar PW, Ondrey FG, Nanchal R, Lee SH, Bock JM. Pepsin: biomarker, mediator, and therapeutic target for reflux and aspiration. Ann N Y Acad Sci. 2018; Dec. 1434(1):282–9.
Article116. Bardhan KD, Strugala V, Dettmar PW. Reflux revisited: advancing the role of pepsin. Int J Otolaryngol. 2012; 2012:646901.
Article117. Strugala V, Avis J, Jolliffe IG, Johnstone LM, Dettmar PW. The role of an alginate suspension on pepsin and bile acids: key aggressors in the gastric refluxate: does this have implications for the treatment of gastro-oesophageal reflux disease. J Pharm Pharmacol. 2009; Aug. 61(8):1021–8.118. McGlashan JA, Johnstone LM, Sykes J, Strugala V, Dettmar PW. The value of a liquid alginate suspension (Gaviscon Advance) in the management of laryngopharyngeal reflux. Eur Arch Otorhinolaryngol. 2009; Feb. 266(2):243–51.
Article119. Reimer C, Lodrup AB, Smith G, Wilkinson J, Bytzer P. Randomised clinical trial: alginate (Gaviscon Advance) vs. placebo as add-on therapy in reflux patients with inadequate response to a once daily proton pump inhibitor. Aliment Pharmacol Ther. 2016; Apr. 43(8):899–909.
Article120. Wilkie MD, Fraser HM, Raja H. Gaviscon® Advance alone versus co-prescription of Gaviscon® Advance and proton pump inhibitors in the treatment of laryngopharyngeal reflux. Eur Arch Otorhinolaryngol. 2018; Oct. 275(10):2515–21.
Article121. Samuels TL, Pearson AC, Wells CW, Stoner GD, Johnston N. Curcumin and anthocyanin inhibit pepsin-mediated cell damage and carcinogenic changes in airway epithelial cells. Ann Otol Rhinol Laryngol. 2013; Oct. 122(10):632–41.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Role of Pepsin in Laryngopharyngeal Reflux
- Is it Necessary to Dissect Level I in Laryngeal and Hypopharyngeal Squamous Cell Carcinoma?
- Virtual Endoscopy Using Spiral CT in Patients with Carcinomas of the Hypopharynx and Larynx
- Occult Neck Metastasis in Larynx and Hypopharynx Squamous Cell Carcinomas Confirmed with Simultaneous Bilateral Elective Neck Dissection
- Hypothyroidism after Treatment for Laryngo-Hypopharyngeal Cancer