Ann Rehabil Med.
2021 Apr;45(2):108-115. 10.5535/arm.20171.
Correlation of Videofluoroscopic Swallowing Study Findings With Radionuclide Salivagram in Chronic Brain-Injured Patients
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Seoul Medical Center, Seoul, Korea
- KMID: 2515391
- DOI: http://doi.org/10.5535/arm.20171
Abstract
Objective
To investigate the correlation between videofluoroscopic swallowing study (VFSS) and radionuclide salivagram findings in chronic brain-injured patients with dysphagia.
Methods
Medical records of chronic brain-injured patients who underwent radionuclide salivagram and VFSS were retrospectively analyzed. Patients were divided into two groups according to salivagram findings. Differences in patient characteristics and clinical factors, including Mini-Mental State Examination (MMSE), Modified Barthel Index (MBI), Functional Ambulatory Category (FAC), feeding method, tracheostomy state, and VFSS findings between the two groups were investigated.
Results
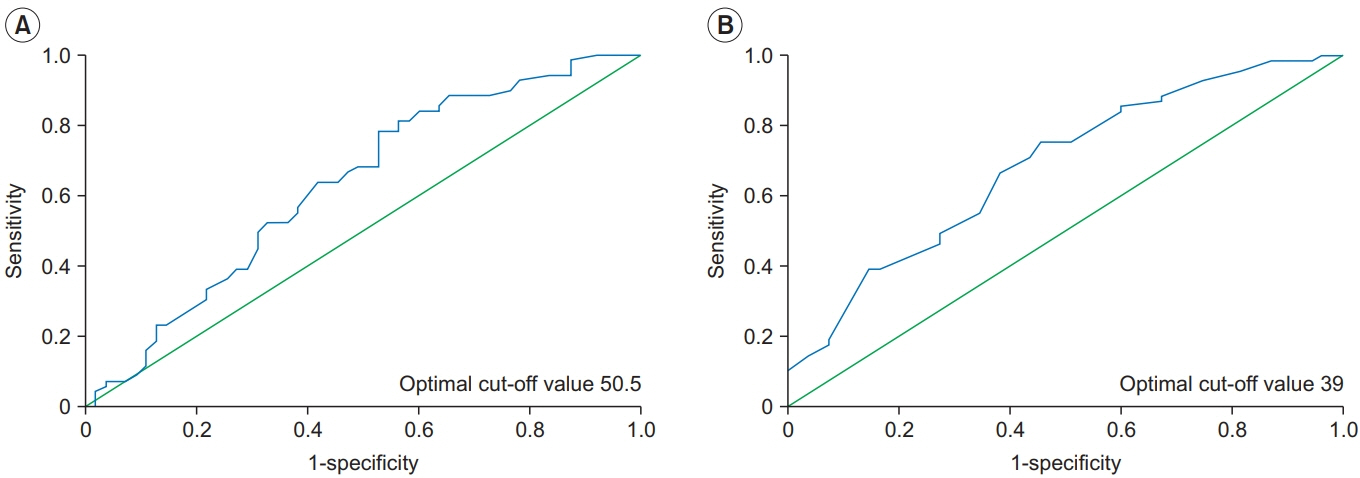
A total of 124 patients were included in this study. There were no significant differences in MMSE, MBI, FAC, feeding method, and presence of tracheostomy between the two groups. However, the incidence of aspiration pneumonia history was significantly higher in the positive salivagram group. The Functional Dysphagia Scale (FDS) was significantly associated with positive salivagram findings, especially in the pharyngeal phase. A multivariate logistic regression analysis showed that laryngeal elevation and epiglottic closure was statistically significant FDS parameter in predicting salivary aspiration on a salivagram (odds ratio=1.100; 95% confidence interval, 1.017–1.190; p=0.018). The receiver operating characteristic (ROC) curve of FDS in the pharyngeal phase showed that an optimum sensitivity and specificity of 55.1% and 65.4%, respectively, when the cut-off value was 39.
Conclusion
In chronic brain-injured patients, inappropriate laryngeal elevation and epiglottic closure is predictive variable for salivary aspiration. Therefore, performing a radionuclide salivagram in patients with FDS of 39 or less in the pharyngeal phase for prevents aspiration pneumonia from salivary aspiration.
Keyword
Figure
Reference
-
1. Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005; 36:2756–63.2. Boesch RP, Daines C, Willging JP, Kaul A, Cohen AP, Wood RE, et al. Advances in the diagnosis and management of chronic pulmonary aspiration in children. Eur Respir J. 2006; 28:847–61.
Article3. Kang Y, Chun MH, Lee SJ. Evaluation of salivary aspiration in brain-injured patients with tracheostomy. Ann Rehabil Med. 2013; 37:96–102.
Article4. Kim SB, Lee SJ, Lee KW, Lee JH, Kim DW. Usefulness of early videofluoroscopic swallowing study in acute stroke patients with dysphagia. Ann Rehabil Med. 2018; 42:42–51.
Article5. Aviv JE, Sacco RL, Mohr JP, Thompson JL, Levin B, Sunshine S, et al. Laryngopharyngeal sensory testing with modified barium swallow as predictors of aspiration pneumonia after stroke. Laryngoscope. 1997; 107:1254–60.
Article6. Croghan JE, Burke EM, Caplan S, Denman S. Pilot study of 12-month outcomes of nursing home patients with aspiration on videofluoroscopy. Dysphagia. 1994; 9:141–6.
Article7. Smith Hammond CA, Goldstein LB, Horner RD, Ying J, Gray L, Gonzalez-Rothi L, et al. Predicting aspiration in patients with ischemic stroke: comparison of clinical signs and aerodynamic measures of voluntary cough. Chest. 2009; 135:769–77.8. Yu KJ, Moon H, Park D. Different clinical predictors of aspiration pneumonia in dysphagic stroke patients related to stroke lesion: a STROBE-complaint retrospective study. Medicine (Baltimore). 2018; 97:e13968.9. Kim GE, Sung IY, Ko EJ, Choi KH, Kim JS. Comparison of videofluoroscopic swallowing study and radionuclide salivagram for aspiration pneumonia in children with swallowing difficulty. Ann Rehabil Med. 2018; 42:52–8.
Article10. Baikie G, South MJ, Reddihough DS, Cook DJ, Cameron DJ, Olinsky A, et al. Agreement of aspiration tests using barium videofluoroscopy, salivagram, and milk scan in children with cerebral palsy. Dev Med Child Neurol. 2005; 47:86–93.
Article11. Park D, Woo SB, Lee DH, Yu KJ, Cho JY, Kim JM, et al. The correlation between clinical characteristics and radionuclide salivagram findings in patients with brain lesions: a preliminary study. Ann Rehabil Med. 2017; 41:915–23.
Article12. Yu KJ, Park D. Clinical characteristics of dysphagic stroke patients with salivary aspiration: a STROBE-compliant retrospective study. Medicine (Baltimore). 2019; 98:e14977.13. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996; 11:93–8.
Article14. Jang DH, Choi KH, Kim DH, Lim CM, Kim JS. Comparison between the radionuclide salivagram and videofluoroscopic swallowing study methods for evaluating patients with aspiration pneumonia. Ann Nucl Med. 2013; 27:247–52.
Article15. Han TR, Paik NJ, Park JW. Quantifying swallowing function after stroke: a functional dysphagia scale based on videofluoroscopic studies. Arch Phys Med Rehabil. 2001; 82:677–82.
Article16. Lee HG, Oh SH, Lee YJ, Kim JS, Choi KH, Cho YA, et al. The use of radionuclide salivagram and videofluoroscopic swallow study in the evaluation of aspiration pneumonia in children. Pediatr Gastroenterol Hepatol Nutr. 2012; 15:160–5.
Article17. Kang IS, Kwon JG, Lee SU, Lee ZI, Park GY, Park HW. Detection of saliva aspiration using salivagram in bedridden patients with brain lesion. J Korean Acad Rehabil Med. 2010; 34:503–7.18. Jafari S, Prince RA, Kim DY, Paydarfar D. Sensory regulation of swallowing and airway protection: a role for the internal superior laryngeal nerve in humans. J Physiol. 2003; 550(Pt 1):287–304.
Article19. Seo HG, Oh BM, Han TR. Longitudinal changes of the swallowing process in subacute stroke patients with aspiration. Dysphagia. 2011; 26:41–8.
Article20. Choi JS, Bang H, Lee GJ, Seo HG, Oh BM, Han TR. Epiglottic retroflexion is a key indicator of functional recovery of post-stroke dysphagia. Ann Rehabil Med. 2020; 44:1–10.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Videofluoroscopic Swallowing Study and Radionuclide Salivagram for Aspiration Pneumonia in Children With Swallowing Difficulty
- Evaluation of Salivary Aspiration in Brain-Injured Patients With Tracheostomy
- The Correlation Between Clinical Characteristics and Radionuclide Salivagram Findings in Patients With Brain Lesions: A Preliminary Study
- Detection of Saliva Aspiration Using Salivagram in Bedridden Patients with Brain Lesion
- Changes of Respiratory Patterns Associated with Swallowing in Brain-injured Patients