Yeungnam Univ J Med.
2021 Apr;38(2):152-156. 10.12701/yujm.2020.00241.
Diplopia developed by cervical traction after cervical spine surgery
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, School of Medicine, Kyungpook National University, Kyungpook National University Chilgok Hospital, Daegu, Korea
- 2Department of Ophthalmology, Gyeongsang National University Hospital, Gyeongsang National University College of Medicine, Jinju, Korea
- 3Department of Anesthesiology and Pain Medicine, Kyungpook National University Hospital, Daegu, Korea
- 4Department of Anesthesiology and Pain Medicine, School of Medicine, Kyungpook National University, Kyungpook National University Hospital, Daegu, Korea
- 5Department of Neurosurgery, School of Medicine, Kyungpook National University, Kyungpook National University Chilgok Hospital, Daegu, Korea
- KMID: 2515190
- DOI: http://doi.org/10.12701/yujm.2020.00241
Abstract
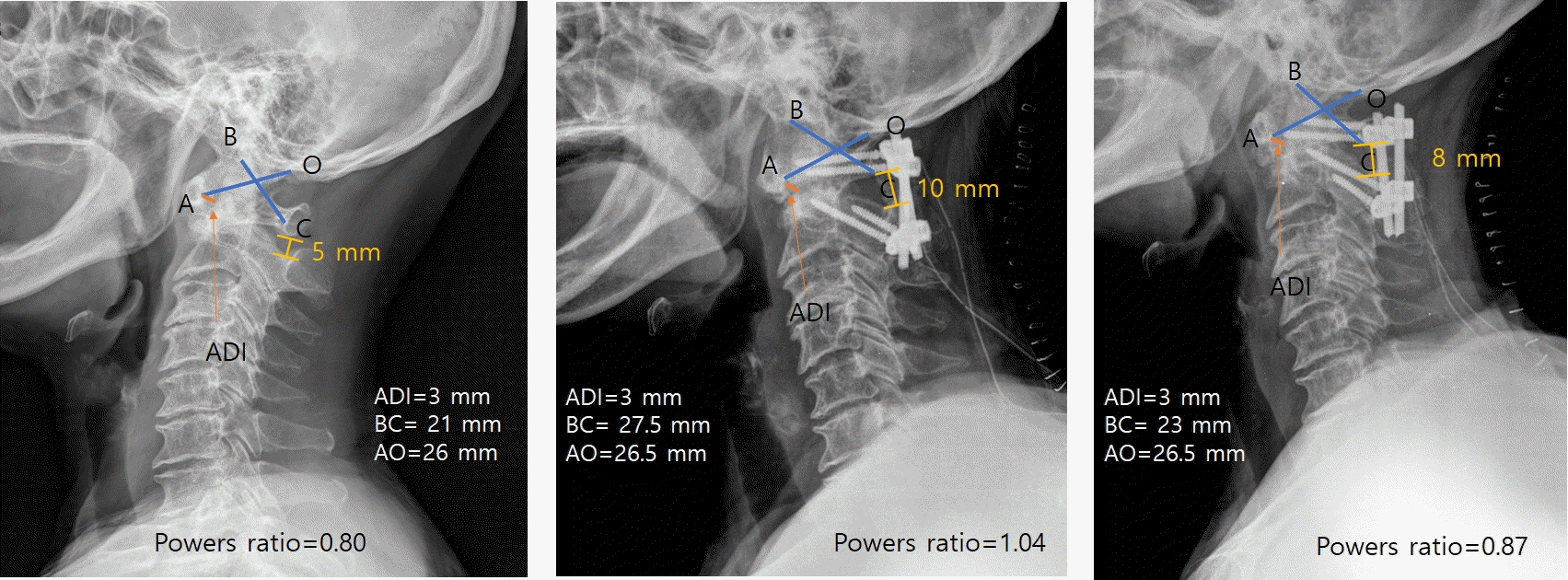
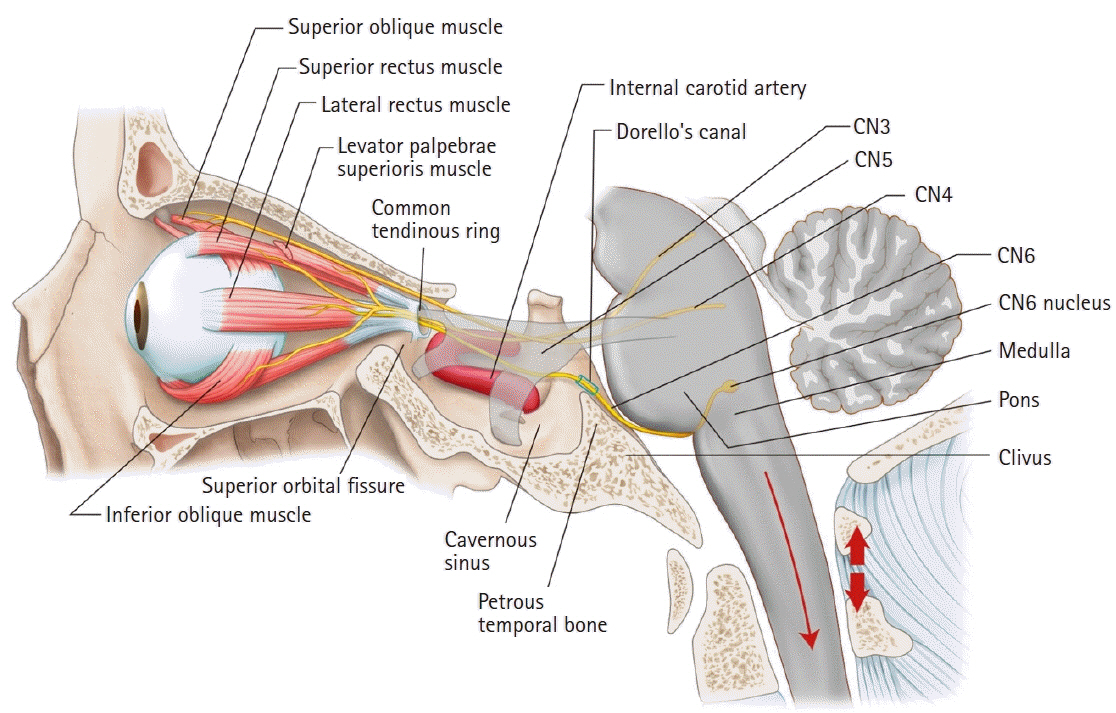
- Diplopia is a rare complication of spine surgery. The abducens nerve is one of the cranial nerves most commonly related to diplopia caused by traction injury. We report a case of a 71-year-old woman who presented with diplopia developing from abducens nerve palsy after C1–C2 fixation and fusion due to atlantoaxial subluxation with cord compression. As soon as we discovered the symptoms, we suspected excessive traction by the instrument and subsequently performed reoperation. Subsequently, the patient’s symptoms improved. In other reported cases we reviewed, most were transient. However, we thought that our rapid response also helped the patient’s fast recovery in this case. The mechanisms by which postoperative diplopia develops vary and, thus, remain unclear. We should pay attention to the fact that the condition is sometimes an indicator of an underlying, life-threatening condition. Therefore, all patients with postoperative diplopia should undergo thorough ophthalmological and neurological evaluations as well as careful observation by a multidisciplinary team.
Figure
Reference
-
References
1. Metzner J, Posner KL, Lam MS, Domino KB. Closed claims’ analysis. Best Pract Res Clin Anaesthesiol. 2011; 25:263–76.
Article2. Abd-Elsayed AA, Barsoum W, Bell G, Farag E. Diplopia following spine surgery: a case series. Open Neurosurg J. 2011; 4:14–5.
Article3. Cho DC, Jung ES, Chi YC. Abducens nerve palsy after lumbar spinal fusion surgery with inadvertent dural tearing. J Korean Neurosurg Soc. 2009; 46:581–3.
Article4. Joo JD, Yoon SH, Kim KJ, Jahng TA, Kim HJ. Isolated abducens nerve palsy due to cerebrospinal fluid leakage following lumbar discectomy: a rare clinical entity. Eur Spine J. 2013; 22(Suppl 3):S421–3.
Article5. Khurana A, Brousil J, Russo A, Evans A, Quraishi NA, Boszczyk BM. Intracranial hypotension with a sixth cranial nerve palsy subsequent to massive thoracic CSF hygroma: a rare complication of thoracic disc excision. Eur Spine J. 2013; 22:2047–54.
Article6. Nakagawa H, Kamimura M, Uchiyama S, Takahara K, Itsubo T, Miyasaka T. Abducens nerve palsy as a rare complication of spinal surgery: a case report. J Orthop Sci. 2003; 8:869–71.
Article7. Sandon LH, Choi G, Park E, Lee HC. Abducens nerve palsy as a postoperative complication of minimally invasive thoracic spine surgery: a case report. BMC Surg. 2016; 16:47.
Article8. Thomas A, Shetty AP, Rajasekaran S. Abducens nerve palsy associated with pseudomeningocele after lumbar disc surgery: a case report. Spine (Phila Pa 1976). 2012; 37:E511–3.9. Barsoum WK, Mayerson J, Bell GR. Cranial nerve palsy as a complication of operative traction. Spine (Phila Pa 1976). 1999; 24:585–6.
Article10. Althomali AT. Diplopia after general anesthesia a post-operative complication or mere coincidence? case report. J Eye Cataract Surg. 2016; 2:11.
Article11. Schievink WI. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA. 2006; 295:2286–96.
Article12. Blumenfeld H. Neuroanatomy through clinical cases. 2nd ed. Sunderland (MA): Sinauer Associates;2010. p. 566–70.13. Miller NR, Subramanian PS, Patel VR, Walsh FB, Hoyt WF. Walsh & Hoyt's clinical neuro-ophthalmology: the essentials. 3rd ed. Philadelphia (PA): Lippincott Williams & Wilkins;2016. p. 365–7.14. Romero FR, Ramos JG, Chaddad-Neto F, Bethencourt JM, de Oliveira E. Microsurgical anatomy and injuries of the abducens nerve. Arq Neuropsiquiatr. 2009; 67:96–101.
Article15. Dengler BA, Bartanusz V. Bilateral abducens nerve palsy following ligamentous C1-C2 distraction. Eur Spine J. 2014; 23(Suppl 2):248–52.
Article16. Master CL, Scheiman M, Gallaway M, Goodman A, Robinson RL, Master SR, et al. Vision diagnoses are common after concussion in adolescents. Clin Pediatr (Phila). 2016; 55:260–7.
Article17. Kumar N, Jivan S, Topping N, Morrell AJ. Blindness and rectus muscle damage following spinal surgery. Am J Ophthalmol. 2004; 138:889–91.
Article18. Hassen GW, Kalantari H. Diplopia from subacute bilateral subdural hematoma after spinal anesthesia. West J Emerg Med. 2012; 13:108–10.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The application of the Halo-pelvic apparatus in Quadriplegia with Unstable fracture-dislocation of cervical spine
- Fracture and Dislocation of the Cervical Spine: Report of 4 Cases
- Neurological Changes after Closed Reduction of Cervical Spine Injury Using Skull Traction
- Concepts and Techniques to Prevent Cervical Spine Deformity After Spine Surgery: A Narrative Review
- Clinical application of Halo body Jacket in the Cervical Spine Lesion