Korean J Gastroenterol.
2021 Apr;77(4):194-198. 10.4166/kjg.2021.032.
Ruptured Pancreaticoduodenal Artery Aneurysm with Pancreatitis Treated Using Endovascular and Endoscopic Methods
- Affiliations
-
- 1Department of Surgery, Wonkwang University School of Medicine, Iksan, Korea
- KMID: 2515141
- DOI: http://doi.org/10.4166/kjg.2021.032
Abstract
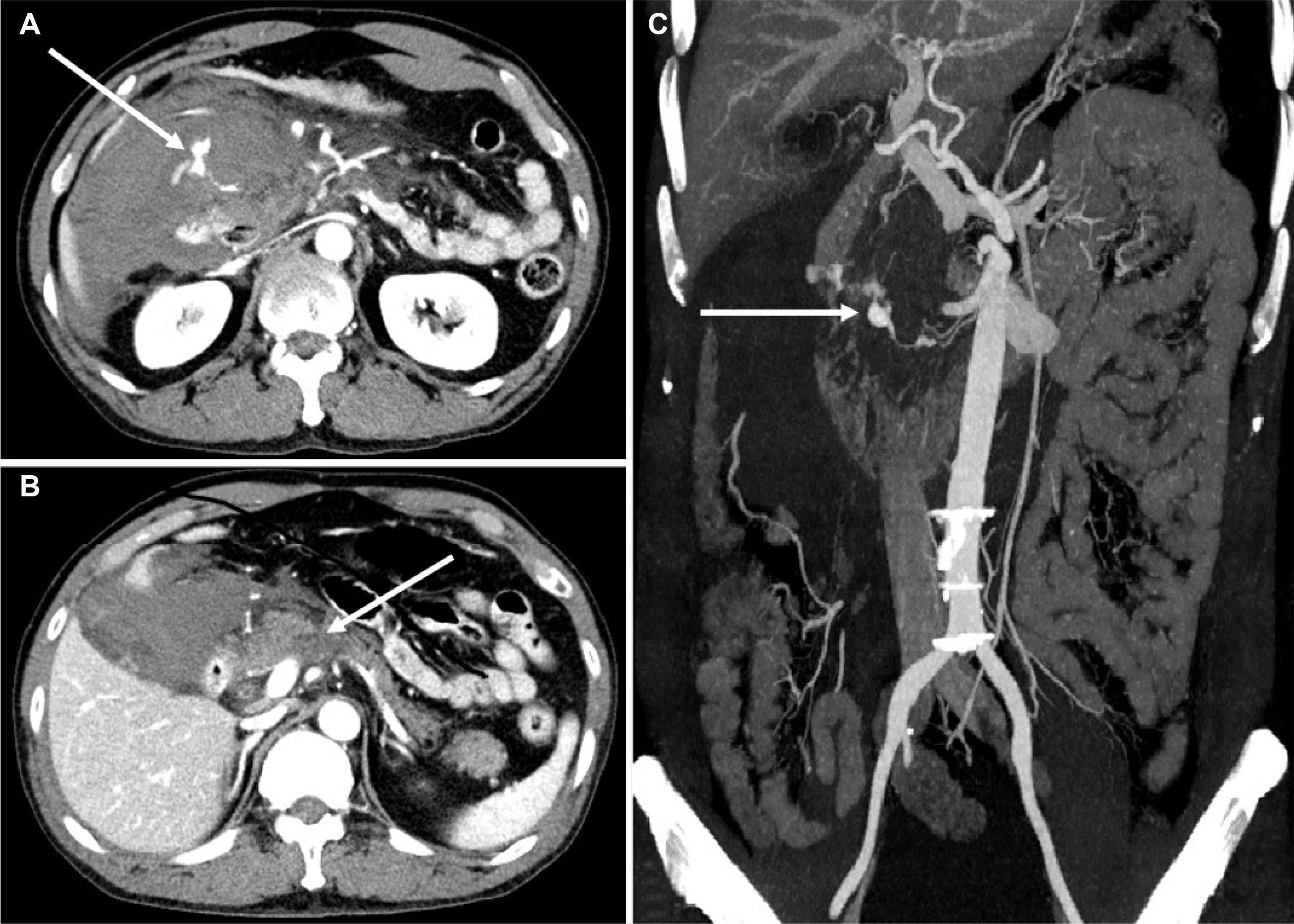
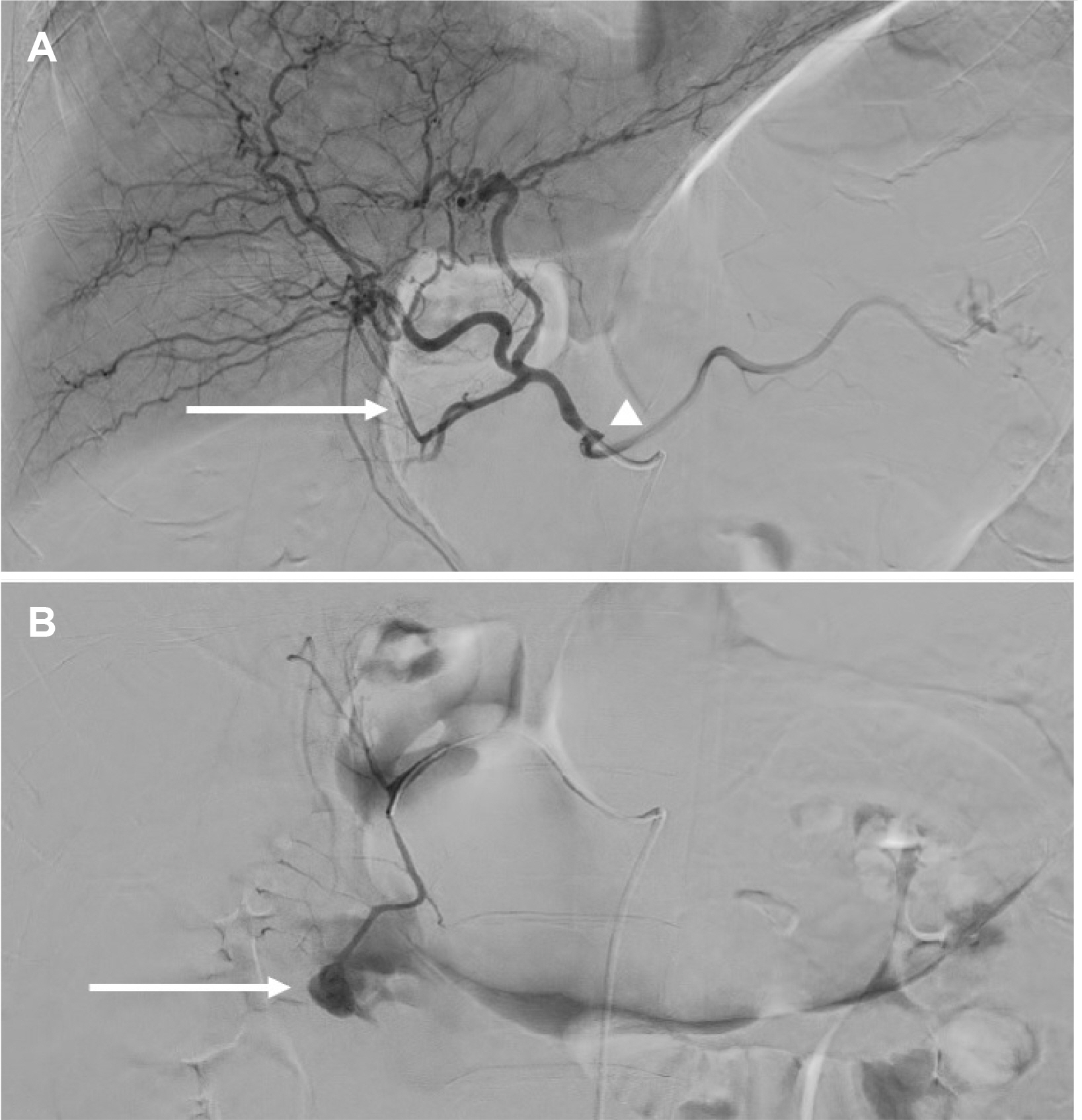
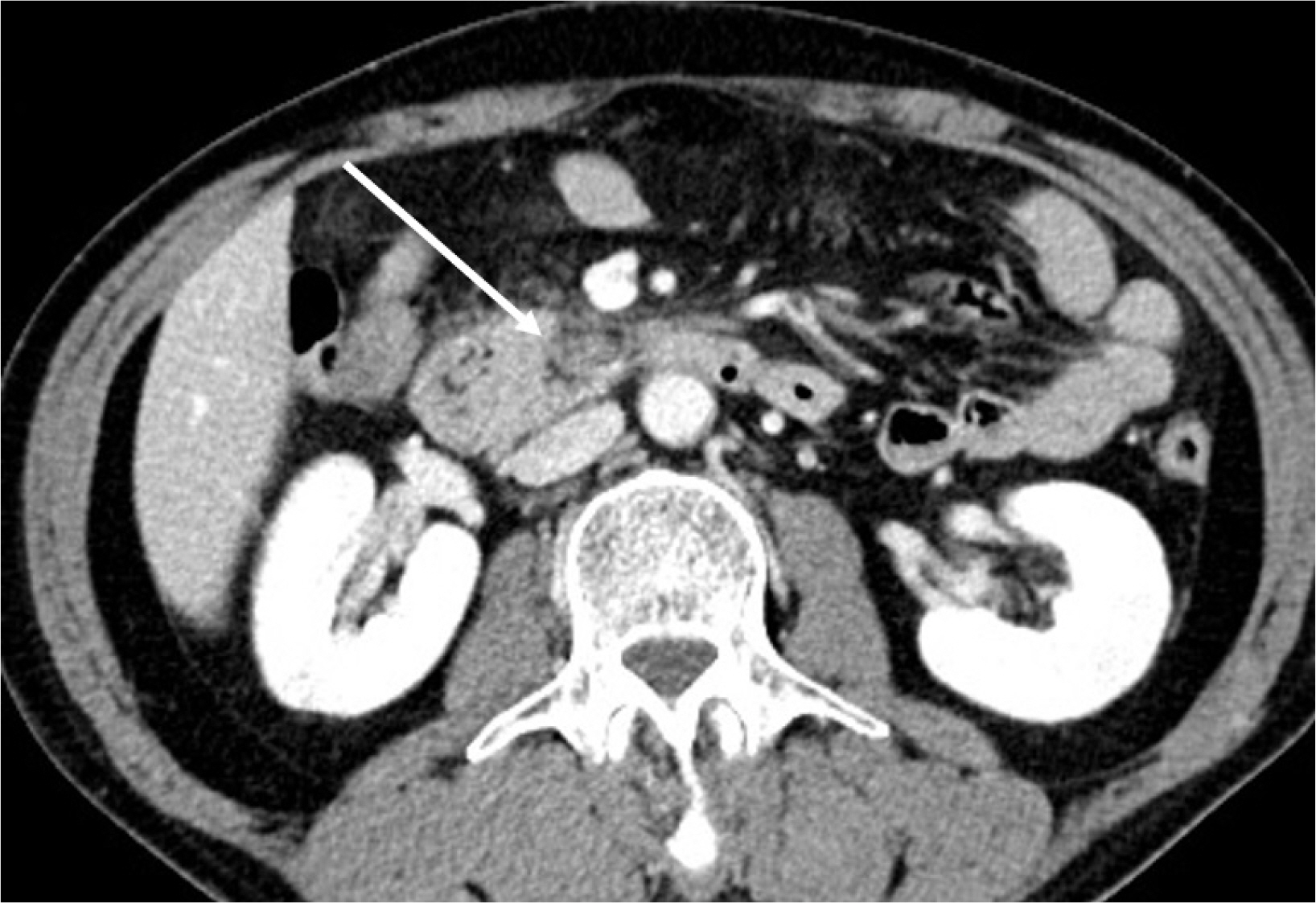
- Pancreaticoduodenal artery aneurysm (PDAA) is a rare form of abdominal visceral aneurysm that accounts for approximately 2% of all cases. Most cases of PDAA are associated with celiac artery stenosis (CAS). Regardless of the size, there is a risk of rupture. Therefore, treatment should be performed immediately after discovery, even though the need to treat the accompanying CAS, if present, is controversial. The authors report a case of ruptured PDAA and accompanying pancreatitis treated using endovascular and endoscopic methods without treatment of CAS. A 50-year-old man was admitted to the emergency department of Wonkwang University Hospital with epigastric pain and hypovolemic shock. CT revealed a ruptured PDAA and a large volume hemoperitoneum. Emergency angiography was performed, and angioembolization of the PDAA was performed successfully. Follow-up CT revealed infection and pancreatitis, which were treated by surgical drainage and pancreatic duct stenting with ERCP. Because the degree of stenosis was not severe, it was decided to follow-up the accompanying CAS. After discharge, the patient was followed up without complications.
Figure
Reference
-
1. Stanley JC, Wakefield TW, Graham LM, Whitehouse WM Jr, Zelenock GB, Lindenauer SM. 1986; Clinical importance and management of splanchnic artery aneurysms. J Vasc Surg. 3:836–840. DOI: 10.1016/0741-5214(86)90059-5.
Article2. Corey MR, Ergul EA, Cambria RP, et al. 2016; The natural history of splanchnic artery aneurysms and outcomes after operative intervention. J Vasc Surg. 63:949–957. DOI: 10.1016/j.jvs.2015.10.066. PMID: 26792545.
Article3. de Perrot M, Berney T, Deléaval J, Bühler L, Mentha G, Morel P. 1999; Management of true aneurysms of the pancreaticoduodenal arteries. Ann Surg. 229:416–420. DOI: 10.1097/00000658-199903000-00016. PMID: 10077055. PMCID: PMC1191708.
Article4. Kalva SP, Athanasoulis CA, Greenfield AJ, et al. 2007; Inferior pancreaticoduodenal artery aneurysms in association with celiac axis stenosis or occlusion. Eur J Vasc Endovasc Surg. 33:670–675. DOI: 10.1016/j.ejvs.2006.12.021. PMID: 17276102.
Article5. Yoon HJ, Choi JS, Shin WY, Lee KY, Ahn SI. 2020; Causal relationship between celiac stenosis and pancreaticoduodenal artery aneurysm: interpretation by simulation using an electric circuit. Biomed Res Int. 2020:2738726. DOI: 10.1155/2020/2738726. PMID: 32596287. PMCID: PMC7298276.
Article6. Sakatani A, Doi Y, Kitayama T, et al. 2016; Pancreaticoduodenal artery aneurysm associated with coeliac artery occlusion from an aortic intramural hematoma. World J Gastroenterol. 22:4259–4263. DOI: 10.3748/wjg.v22.i16.4259. PMID: 27122676. PMCID: PMC4837443.
Article7. Coll DP, Ierardi R, Kerstein MD, Yost S, Wilson A, Matsumoto T. 1998; Aneurysms of the pancreaticoduodenal arteries: a change in management. Ann Vasc Surg. 12:286–291. DOI: 10.1007/s100169900155. PMID: 9588518.
Article8. Ricci G, Riu P, Attinà GM, et al. 2017; Endovascular treatment of ruptured pancreaticoduodenal artery aneurysm: the importance of collateral vessels. A case report. Int J Surg Case Rep. 41:205–208. DOI: 10.1016/j.ijscr.2017.10.036. PMID: 29096344. PMCID: PMC5686227.
Article9. Murata S, Tajima H, Fukunaga T, et al. 2006; Management of pancreaticoduodenal artery aneurysms: results of superselective transcatheter embolization. AJR Am J Roentgenol. 187:W290–W298. DOI: 10.2214/AJR.04.1726. PMID: 16928907.
Article10. Takeuchi Y, Morikage N, Samura M, et al. 2017; Treatment options for celiac stenosis and pancreaticoduodenal artery aneurysms. Ann Vasc Surg. 41:281.e21–281.e23. DOI: 10.1016/j.avsg.2016.10.036. PMID: 28238917.
Article11. Sgroi MD, Kabutey NK, Krishnam M, Fujitani RM. 2015; Pancreaticoduodenal artery aneurysms secondary to median arcuate ligament syndrome may not need celiac artery revascularization or ligament release. Ann Vasc Surg. 29:122.e1–122.e1227. DOI: 10.1016/j.avsg.2014.05.020. PMID: 24930977.
Article12. Sugae T, Fujii T, Kodera Y, et al. 2012; Classification of the celiac axis stenosis owing to median arcuate ligament compression, based on severity of the stenosis with subsequent proposals for management during pancreatoduodenectomy. Surgery. 151:543–549. DOI: 10.1016/j.surg.2011.08.012. PMID: 22001637.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anterior Superior Pancreaticoduodenal Artery Aneurysm Rupture Associated with Abdominal Pain
- Endovascular Coil Trapping of a Ruptured Dissecting Aneurysm of the Vertebral Artery Using Detachable Coils and Micro-Tornado(R) Coils
- Rupture of an Idiopathic Aneurysm of the Inferior Pancreaticoduodenal Artery Leading to an Intra-Abdominal Bleeding
- Endovascular Treatment of Multiple Pancreaticoduodenal Artery Aneurysms Associated with Celiac Artery Stenosis: A Case Report
- Retroperitoneal Hematoma Caused by Ruptured Pancreaticoduodenal Artery Aneurysm