Pediatric liver transplantation using a hepatitis B surface antigen-positive donor liver graft for congenital absence of the portal vein
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Pediatrics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2514410
- DOI: http://doi.org/10.4285/kjt.20.0038
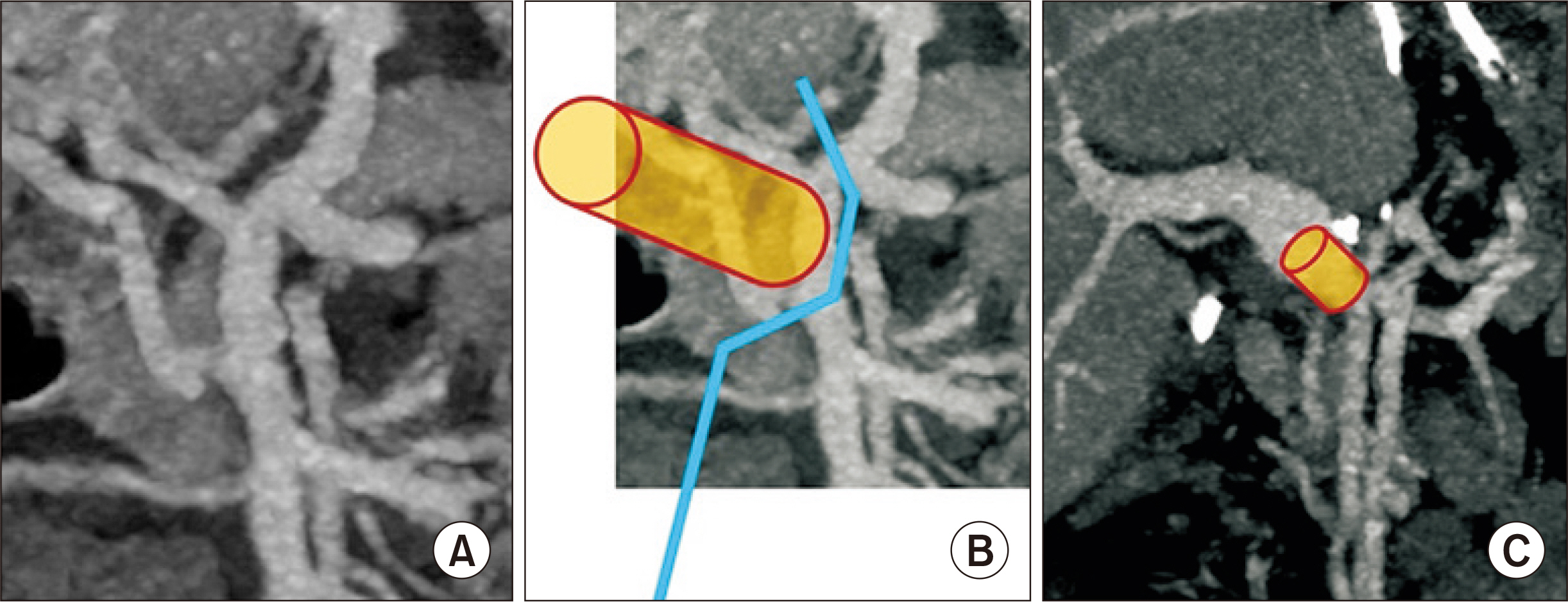
Abstract
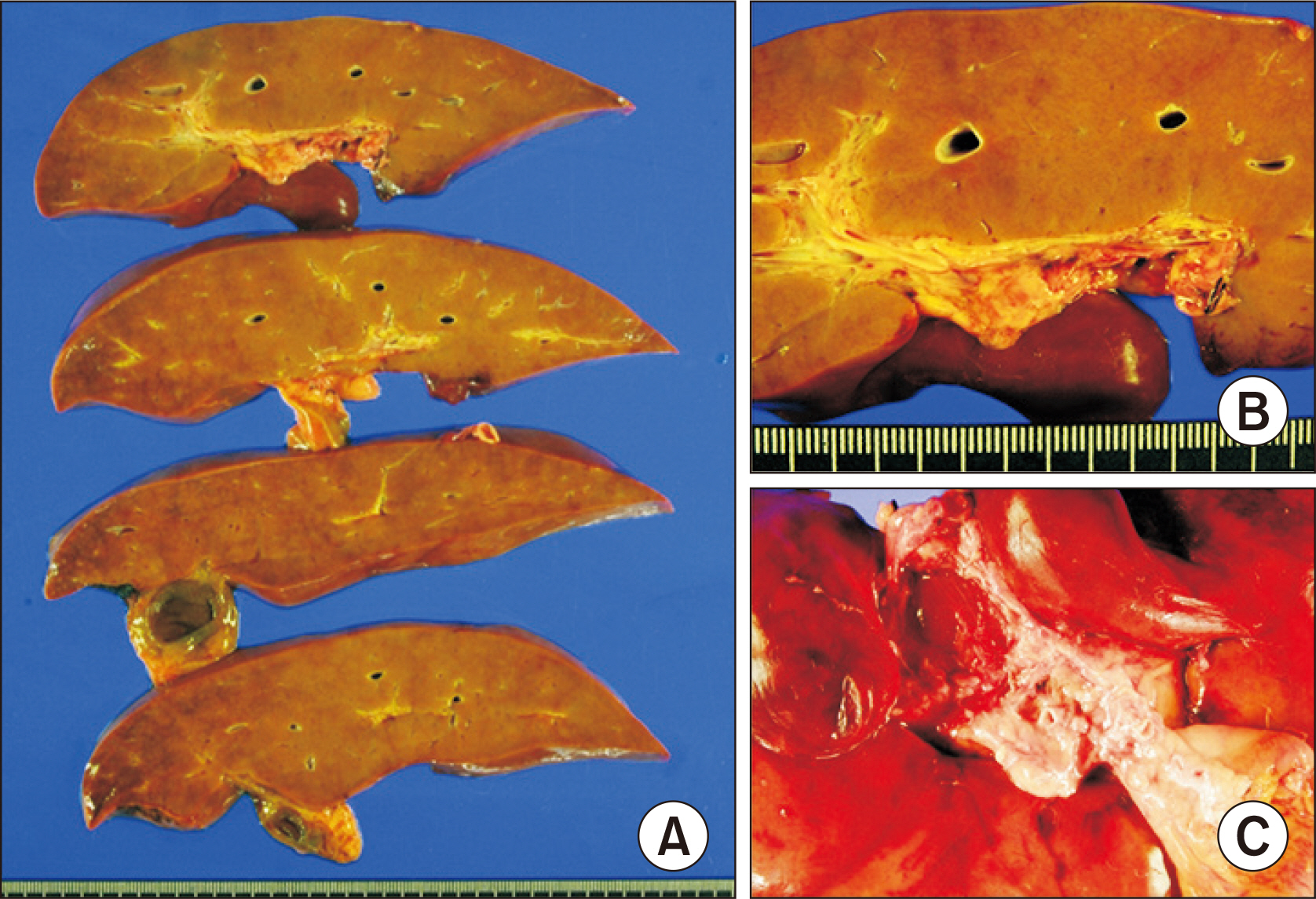
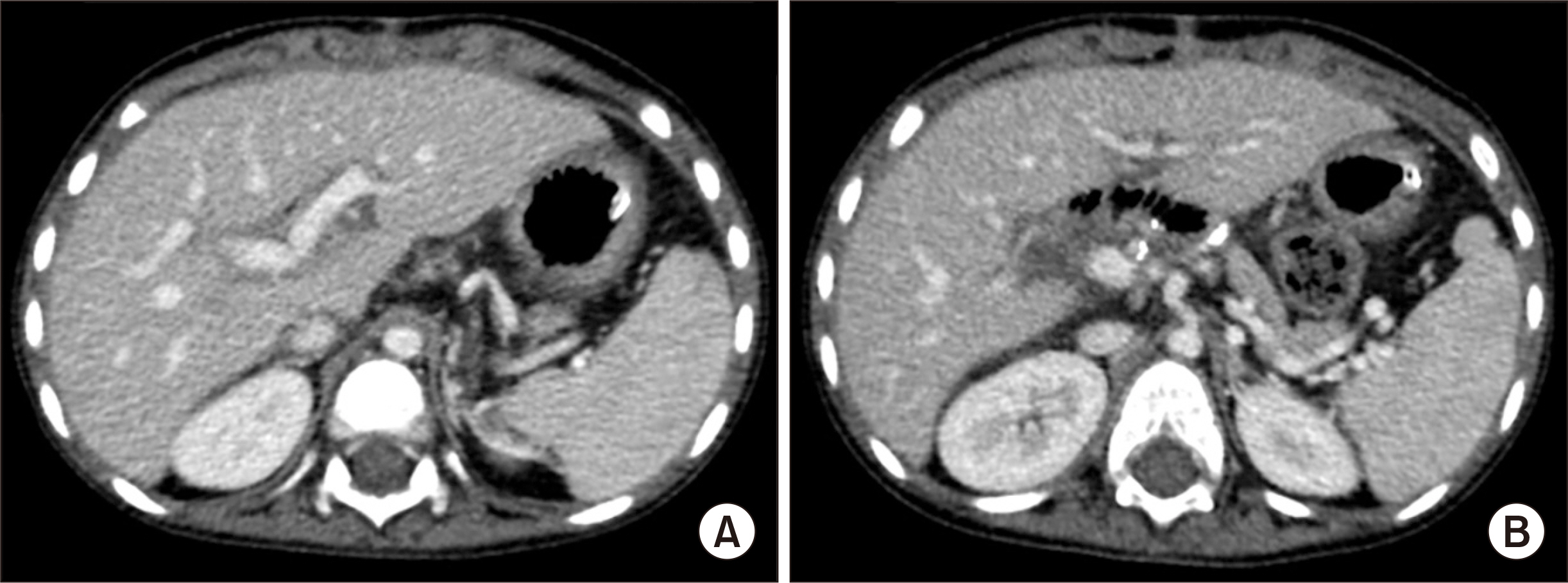
- Congenital absence of the portal vein (CAPV) is a rare venous malformation in which mesenteric venous blood drains directly into systemic circulation. Herein, we report a case of pediatric deceased donor liver transplantation (DDLT) for symptomatic CAPV with whole liver graft from a hepatitis B surface antigen (HBsAg)-positive donor. A 4-year-old boy suffered from CAPV and secondary portal hypertension. He was also diagnosed with DiGeorge syndrome and heart anomalies. After waiting for 4 months, a 5-year-old donor weighing 19 kg with positive HBsAg was allocated to this 4-year-old patient weighing 15 kg. Recipient operation was performed according to the standard procedures of pediatric DDLT. Portal vein reconstruction was performed using interposition of a vascular homograft conduit to the superior mesenteric vein-splenic vein confluence. The patient recovered uneventfully from DDLT. He has been administered with lamivudine to prevent hepatitis B virus infection. This patient has been doing well for 5 years after DDLT without growth retardation. In conclusion, CAPV patients can have various vascular anomalies, thus combined vascular anomalies should be thoroughly assessed before and during liver transplantation operation. The most effective reconstruction techniques should be used to achieve satisfactory results following liver transplantation.
Keyword
Figure
Cited by 4 articles
-
Living donor liver transplantation in a pediatric patient with congenital absence of the portal vein
Jung-Man Namgoong, Shin Hwang, Gil-Chun Park, Hyunhee Kwon, Kyung Mo Kim, Seak Hee Oh
Ann Hepatobiliary Pancreat Surg. 2021;25(3):401-407. doi: 10.14701/ahbps.2021.25.3.401.Living donor liver transplantation with graft dextro-rotation and vein interposition in a pediatric patient with congenital absence of the portal vein
Jung-Man Namgoong, Shin Hwang, Gil-Chun Park, Sang-Hoon Kim, Kyung Mo Kim, Seak Hee Oh
Ann Liver Transplant. 2023;3(1):35-43. doi: 10.52604/alt.23.0004.Living donor liver transplantation with direct collateral portal vein anastomosis in a pediatric patient with congenital absence of the portal vein
Jung-Man Namgoong, Shin Hwang, Gil-Chun Park, Do Young Lee, Kyung Mo Kim, Seak Hee Oh
Ann Liver Transplant. 2023;3(2):128-135. doi: 10.52604/alt.23.0013.Living donor liver transplantation with pericholedochal collateral vein anastomosis in a pediatric patient with congenital absence of the portal vein
Jung-Man Namgoong, Shin Hwang, Gil-Chun Park, Sujin Kang, Kyung Mo Kim, Seak Hee Oh
Ann Liver Transplant. 2023;3(2):118-127. doi: 10.52604/alt.23.0016.
Reference
-
1. Shinkai M, Ohhama Y, Nishi T, Yamamoto H, Fujita S, Take H, et al. 2001; Congenital absence of the portal vein and role of liver transplantation in children. J Pediatr Surg. 36:1026–31. DOI: 10.1053/jpsu.2001.24731. PMID: 11431769.
Article2. Sumida W, Kaneko K, Ogura Y, Tainaka T, Ono Y, Seo T, et al. 2006; Living donor liver transplantation for congenital absence of the portal vein in a child with cardiac failure. J Pediatr Surg. 41:e9–12. DOI: 10.1016/j.jpedsurg.2006.07.014. PMID: 17101345.
Article3. Watanabe A. 2000; Portal-systemic encephalopathy in non-cirrhotic patients: classification of clinical types, diagnosis and treatment. J Gastroenterol Hepatol. 15:969–79. DOI: 10.1046/j.1440-1746.2000.02283.x. PMID: 11059925.
Article4. Morgan G, Superina R. 1994; Congenital absence of the portal vein: two cases and a proposed classification system for portasystemic vascular anomalies. J Pediatr Surg. 29:1239–41. DOI: 10.1016/0022-3468(94)90812-5. PMID: 7807356.
Article5. Mistinova J, Valacsai F, Varga I. 2010; Congenital absence of the portal vein: case report and a review of literature. Clin Anat. 23:750–8. DOI: 10.1002/ca.21007. PMID: 20533511.6. Emre S, Arnon R, Cohen E, Morotti RA, Vaysman D, Shneider BL. 2007; Resolution of hepatopulmonary syndrome after auxiliary partial orthotopic liver transplantation in Abernethy malformation: a case report. Liver Transpl. 13:1662–8. DOI: 10.1002/lt.21349. PMID: 18044784.
Article7. Hwang S, Kim DY, Ahn CS, Moon DB, Kim KM, Park GC, et al. 2013; Computational simulation-based vessel interposition reconstruction technique for portal vein hypoplasia in pediatric liver transplantation. Transplant Proc. 45:255–8. DOI: 10.1016/j.transproceed.2012.05.090. PMID: 23375311.
Article8. Matsuura T, Soejima Y, Taguchi T. 2010; Auxiliary partial orthotopic living donor liver transplantation with a small-for-size graft for congenital absence of the portal vein. Liver Transpl. 16:1437–9. DOI: 10.1002/lt.22179. PMID: 21117255.
Article9. Law YM, Mack CL, Sokol RJ, Rice M, Parsley L, Ivy D. 2011; Cardiopulmonary manifestations of portovenous shunts from congenital absence of the portal vein: pulmonary hypertension and pulmonary vascular dilatation. Pediatr Transplant. 15:E162–8. DOI: 10.1111/j.1399-3046.2010.01355.x. PMID: 20565694. PMCID: PMC3203339.
Article10. Uchida H, Sakamoto S, Shigeta T, Hamano I, Kanazawa H, Fukuda A, et al. 2012; Living donor liver transplantation with renoportal anastomosis for a patient with congenital absence of the portal vein. Case Rep Surg. 2012:670289. DOI: 10.1155/2012/670289. PMID: 23091767. PMCID: PMC3471411.
Article11. Gordon-Burroughs S, Balogh J, Weiner MA, Monsour HP Jr, Schwartz MR, Gaber AO, et al. 2014; Liver transplantation in an adult with adenomatosis and congenital absence of the portal vein: a case report. Transplant Proc. 46:2418–21. DOI: 10.1016/j.transproceed.2014.04.012. PMID: 25242797.
Article12. Brasoveanu V, Ionescu MI, Grigorie R, Mihaila M, Bacalbasa N, Dumitru R, et al. 2015; Living donor liver transplantation for unresectable liver adenomatosis associated with congenital absence of portal vein: a case report and literature review. Am J Case Rep. 16:637–44. DOI: 10.12659/AJCR.895235. PMID: 26386552. PMCID: PMC4581685.
Article13. Li P, Hidaka M, Hamada T, Ikeda S, Ono S, Maruya Y, et al. 2020; Living donor liver transplantation for congenital absence of portal vein in portal venous reconstruction with a great saphenous vein graft. Surg Case Rep. 6:153. DOI: 10.1186/s40792-020-00916-8. PMID: 32601822. PMCID: PMC7324451.
Article14. Matsumoto N, Matsusaki T, Hiroi K, Kaku R, Yoshida R, Umeda Y, et al. 2020; Pediatric living donor liver transplantation for congenital absence of the portal vein with pulmonary hypertension: a case report. Transplant Proc. 52:630–3. DOI: 10.1016/j.transproceed.2019.11.032. PMID: 32029317.
Article15. Hwang S, Kim DY, Namgoong JM, Kim KM, Oh SH, Kim KH, et al. 2020; Living donor liver retransplantation for primary non-function of liver graft following multivisceral transplantation in a pediatric patient. Ann Hepatobiliary Pancreat Surg. 24:198–202. DOI: 10.14701/ahbps.2020.24.2.198. PMID: 32457267. PMCID: PMC7271102.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Living donor liver transplantation with graft dextro-rotation and vein interposition in a pediatric patient with congenital absence of the portal vein
- Living donor liver transplantation with direct collateral portal vein anastomosis in a pediatric patient with congenital absence of the portal vein
- Living donor liver transplantation in a pediatric patient having intrahepatic portocaval shunt with congenital absence of the intrahepatic portal vein
- Living donor liver transplantation with proximal splenic vein ligation in a pediatric patient with congenital absence of the portal vein
- Congenital Absence of the Horizontal Segment of the Left Portal Vein