J Cerebrovasc Endovasc Neurosurg.
2021 Mar;23(1):6-15. 10.7461/jcen.2021.E2020.07.002.
Surgical revascularization for Moyamoya disease in the United States: A cost-effectiveness analysis
- Affiliations
-
- 1Department of Neurological Surgery, University of California, San Diego, CA, USA
- 2Department of Neurology, University of California, San Diego, CA, USA
- 3Department of Radiation Medicine and Applied Sciences, University of California, San Diego, CA, USA
- KMID: 2514333
- DOI: http://doi.org/10.7461/jcen.2021.E2020.07.002
Abstract
Objective
Moyamoya disease (MMD) is a vasculopathy of the internal carotid arteries with ischemic and hemorrhagic sequelae. Surgical revascularization confers upfront peri-procedural risk and costs in exchange for long-term protective benefit against hemorrhagic disease. The authors present a cost-effectiveness analysis (CEA) of surgical versus non-surgical management of MMD.
Methods
A Markov Model was used to simulate a 41-year-old suffering a transient ischemic attack (TIA) secondary to MMD and now faced with operative versus nonoperative treatment options. Health utilities, costs, and outcome probabilities were obtained from the CEA registry and the published literature. The primary outcome was incremental cost-effectiveness ratio which compared the quality adjusted life years (QALYs) and costs of surgical and nonsurgical treatments. Base-case, one-way sensitivity, two-way sensitivity, and probabilistic sensitivity analyses were performed with a willingness to pay threshold of $50,000.
Results
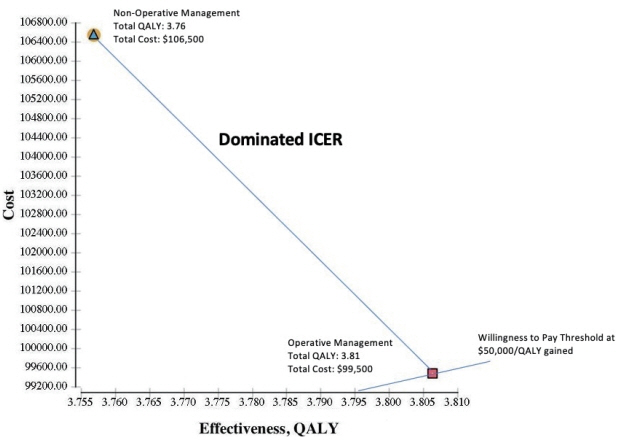
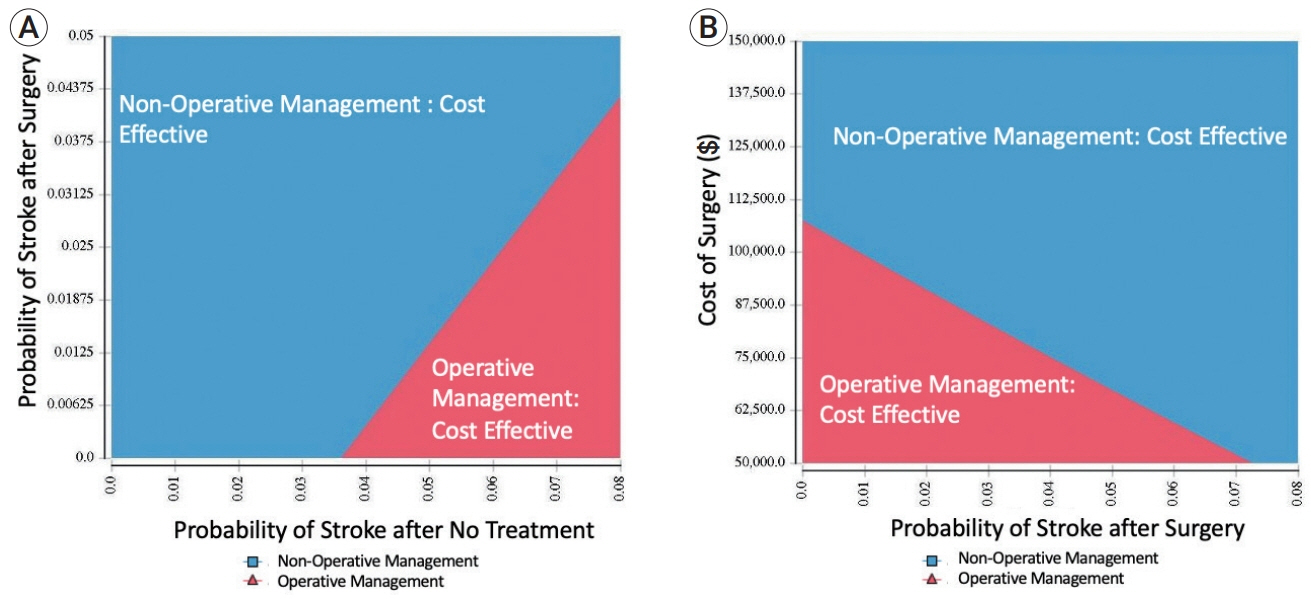
The base case model yielded 3.81 QALYs with a cost of $99,500 for surgery, and 3.76 QALYs with a cost of $106,500 for nonsurgical management. One-way sensitivity analysis demonstrated the greatest sensitivity in assumptions to cost of surgery and cost of admission for hemorrhagic stroke, and probabilities of stroke with no surgery, stroke after surgery, poor surgical outcome, and death after surgery. Probabilistic sensitivity analyses demonstrated that surgical revascularization was the cost-effective strategy in over 87.4% of simulations.
Conclusions
Considering both direct and indirect costs and the postoperative QALY, surgery is considerably more cost-effective than non-surgical management for adults with MMD.
Figure
Reference
-
1. Baaj AA, Agazzi S, Sayed ZA, Toledo M, Spetzler RF, van Loveren H. Surgical management of moyamoya disease: a review. Neurosurg Focus. 2009; Apr. 26(4):E7.2. Braithwaite RS, Meltzer DO, King JT Jr, Leslie D, Roberts MS. What does the value of modern medicine say about the $50,000 per quality-adjusted life-year decision rule? Med Care. 2008; Apr. 46(4):349–56.
Article3. Bureau of Labor Statistics. CPI Inflation Calculator. Databases, Tables & Calculators by Subject: United States Department of Labor;2016.4. Centers for Disease Control and Prevention. Datasets and Related Documentation for Mortality Data. National Series for Health Statistics.5. Concato J, Feinstein AR. Monte Carlo methods in clinical research: applications in multivariable analysis. J Investig Med. 1997; Aug. 45(6):394–400.6. Deng X, Gao F, Zhang D, Zhang Y, Wang R, Wang S, et al. Direct versus indirect bypasses for adult ischemic-type moyamoya disease: a propensity score-matched analysis. J Neurosurg. 2018; Jun. 128(6):1785–91.
Article7. EC/IC Bypass Study Group. Failure of extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke. Results of an international randomized trial. N Engl J Med. 1985; Nov. 313(19):1191–200.8. Grysiewicz RA, Thomas K, Pandey DK. Epidemiology of ischemic and hemorrhagic stroke: incidence, prevalence, mortality, and risk factors. Neurol Clin. 2008; Nov. 26(4):871–95, vii.
Article9. Guzman R, Lee M, Achrol A, Bell-Stephens T, Kelly M, Do HM, et al. Clinical outcome after 450 revascularization procedures for moyamoya disease. Clinical article. J Neurosurg. 2009; Nov. 111(5):927–35.10. Han JS, Abou-Hamden A, Mandell DM, Poublanc J, Crawley AP, Fisher JA, et al. Impact of extracranial-intracranial bypass on cerebrovascular reactivity and clinical outcome in patients with symptomatic moyamoya vasculopathy. Stroke. 2011; Nov. 42(11):3047–54.
Article11. Houkin K, Kamiyama H, Abe H, Takahashi A, Kuroda S. Surgical therapy for adult moyamoya disease. Can surgical revascularization prevent the recurrence of intracerebral hemorrhage? Stroke. 1996; Aug. 27(8):1342–6.12. Hunink MG. In search of tools to aid logical thinking and communicating about medical decision making. Med Decis Making. 2001; Jul-Aug. 21(4):267–77.
Article13. Kainth D, Chaudhry SA, Kainth H, Suri FK, Qureshi AI. Epidemiological and clinical features of moyamoya disease in the USA. Neuroepidemiology. 2013; 40(4):282–7.
Article14. Kawaguchi S, Okuno S, Sakaki T. Effect of direct arterial bypass on the prevention of future stroke in patients with the hemorrhagic variety of moyamoya disease. J Neurosurg. 2000; Sep. 93(3):397–401.
Article15. Li J, Zhao Y, Zhao M, Cao P, Liu X, Ren H, et al. High variance of intraoperative blood pressure predicts early cerebral infarction after revascularization surgery in patients with Moyamoya disease. Neurosurg Rev. 2020; Apr. 43(2):759–69.
Article16. Li Q, Gao Y, Xin W, Zhou Z, Rong H, Qin Y, et al. Meta-analysis of the prognosis of different treatments of symptomatic moyamoya disease. World Neurosurg. 2019; Jul. 127:354–61.17. Liu X, Zhang D, Shuo W, Zhao Y, Wang R, Zhao J. Long term outcome after conservative and surgical treatment of haemorrhagic moyamoya disease. J Neurol Neurosurg Psychiatry. 2013; Mar. 84(3):258–65.
Article18. Luengo-Fernandez R, Gray AM, Bull L, Welch S, Cuthbertson F, Rothwell PM, et al. Quality of life after TIA and stroke ten-year results of the Oxford Vascular Study. Neurology. 2013; Oct. 81(18):1588–95.
Article19. Miao W, Zhao PL, Zhang YS, Liu HY, Chang Y, Ma J, et al. Epidemiological and clinical features of Moyamoya disease in Nanjing, China. Clin Neurol Neurosurg. 2010; Apr. 112(3):199–203.
Article20. milstein a, galvin rs, delbanco sf, salber p, buck cr jr. improving the safety of health care: the leapfrog initiative. eff Clin Pract. 2000; Nov-Dec. 3(6):313–6.21. Miyamoto S, Yoshimoto T, Hashimoto N, Okada Y, Tsuji I, Tominaga T, et al. Effects of extracranial-intracranial bypass for patients with hemorrhagic moyamoya disease: results of the Japan Adult Moyamoya Trial. Stroke. 2014; May. 45(5):1415–21.22. Nelson RE, Saltzman GM, Skalabrin EJ, Demaerschalk BM, Majersik JJ. The cost-effectiveness of telestroke in the treatment of acute ischemic stroke. Neurology. 2011; Oct. 77(17):1590–8.
Article23. Park SE, Kim JS, Park EK, Shim KW, Kim DS. Direct versus indirect revascularization in the treatment of moyamoya disease. J Neurosurg. 2018; Aug. 129(2):480–9.
Article24. Rivero-Arias O, Ouellet M, Gray A, Wolstenholme J, Rothwell PM, Luengo-Fernandez R. Mapping the modified Rankin scale (mRS) measurement into the generic EuroQol (EQ-5D) health outcome. Med Decis Making. 2010; MayJun. 30(3):341–54.
Article25. Scott RM, Smith JL, Robertson RL, Madsen JR, Soriano SG, Rockoff MA. Long-term outcome in children with moyamoya syndrome after cranial revascularization by pial synangiosis. J Neurosurg. 2004; Feb. 100(2 Suppl Pediatrics):142–9.
Article26. Starke RM, Crowley RW, Maltenfort M, Jabbour PM, Gonzalez LF, Tjoumakaris SI, et al. Moyamoya disorder in the United States. Neurosurgery. 2012; Jul. 71(1):93–9.
Article27. Suzuki J, Takaku A. Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol. 1969; Mar. 20(3):288–99.28. Takahashi JC, Miyamoto S. Moyamoya disease: recent progress and outlook. Neurol Med Chir (Tokyo). 2010; 50(9):824–32.
Article29. Titsworth WL, Scott RM, Smith ER. National analysis of 2454 pediatric Moyamoya admissions and the effect of hospital volume on outcomes. Stroke. 2016; May. 47(5):1303–11.
Article30. Wali AR, Brandel MG, Santiago-Dieppa DR, Rennert RC, Steinberg JA, Hirshman BR, et al. Markov modeling for the neurosurgeon: a review of the literature and an introduction to cost-effectiveness research. Neurosurg Focus. 2018; May. 44(5):E20.
Article31. Wali AR, Park CC, Santiago-Dieppa DR, Vaida F, Murphy JD, Khalessi AA. Pipeline embolization device versus coiling for the treatment of large and giant unruptured intracranial aneurysms: a cost-effectiveness analysis. Neurosurg Focus. 2017; Jun. 42(6):E6.
Article32. Wouters A, Smets I, Van den Noortgate W, Steinberg GK, Lemmens R. Cerebrovascular events after surgery versus conservative therapy for moyamoya disease: a meta-analysis. Acta Neurol Belg. 2019; Sep. 119(3):305–13.
Article33. Yu L, Ma L, Huang Z, Shi Z, Wang R, Zhao Y, et al. Revascularization surgery in patients with ischemic-type Moyamoya disease: predictors for postoperative stroke and long-term outcomes. World Neurosurg. 2019; Aug. 128:e582–96.
Article34. Zeifert PD, Karzmark P, Bell-Stephens TE, Steinberg GK, Dorfman LJ. Neurocognitive performance after cerebral revascularization in adult moyamoya disease. Stroke. 2017; Jun. 48(6):1514–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neuroimaging Diagnosis and Treatment of Moyamoya Disease
- Moyamoya Disease: Treatment and Outcomes
- Surgical Results of Encephaloduroarteriomyosynangiosis(EDAMS) for Moyamoya Desease
- Indirect revascularization surgery for moyamoya disease in children and its special considerations
- Cost-Utility Analysis of Non-Contrast Abbreviated Magnetic Resonance Imaging for Hepatocellular Carcinoma Surveillance in Cirrhosis