Diabetes Metab J.
2021 Mar;45(2):251-259. 10.4093/dmj.2020.0206.
Effects of a DPP-4 Inhibitor and RAS Blockade on Clinical Outcomes of Patients with Diabetes and COVID-19
- Affiliations
-
- 1Department of Endocrinology and Metabolism, Kyung Hee University School of Medicine, Seoul, Korea
- 2Data Science Team, Hanmi Pharm. Co. Ltd., Seoul, Korea
- 3Department of Family Medicine, Supportive Care Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Department of Endocrinology and Metabolism, Ajou University School of Medicine, Suwon, Korea
- KMID: 2514201
- DOI: http://doi.org/10.4093/dmj.2020.0206
Abstract
- Background
Dipeptidyl peptidase-4 inhibitor (DPP-4i) and renin-angiotensin system (RAS) blockade are reported to affect the clinical course of coronavirus disease 2019 (COVID-19) in patients with diabetes mellitus (DM).
Methods
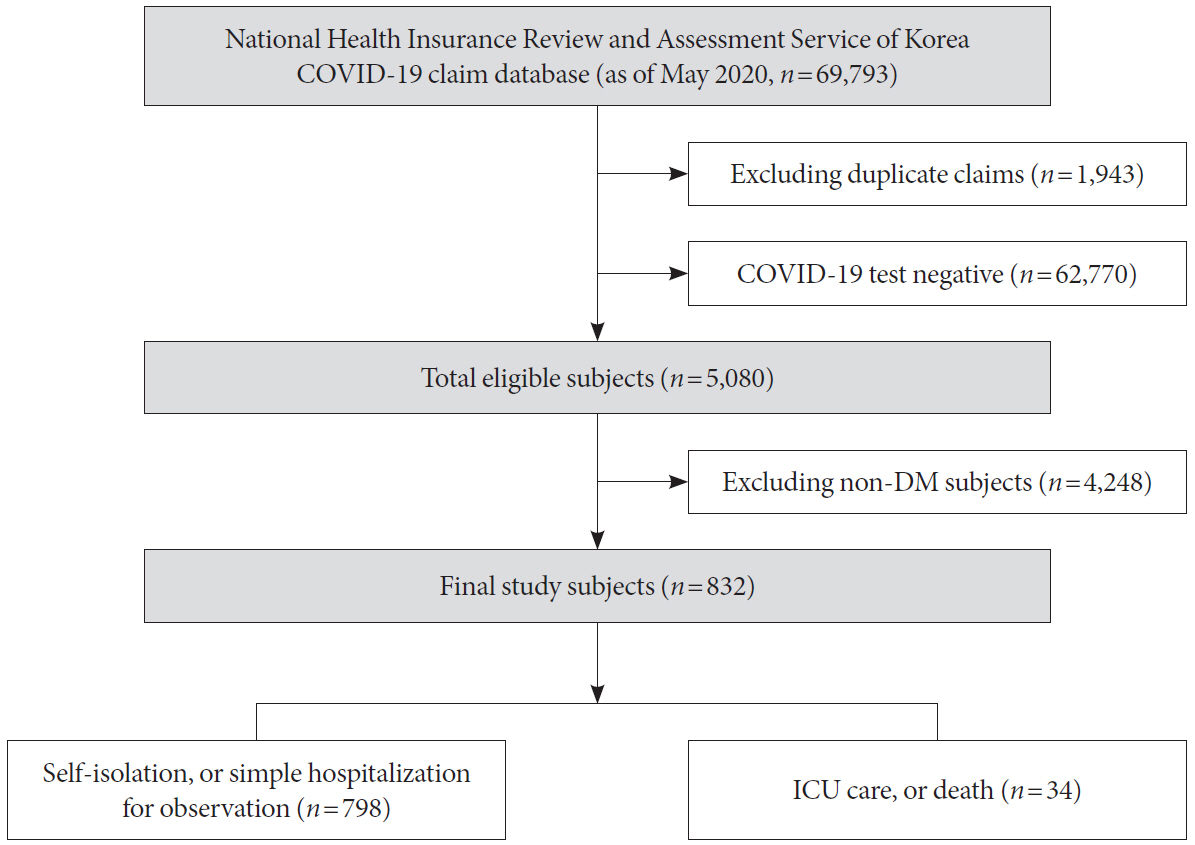
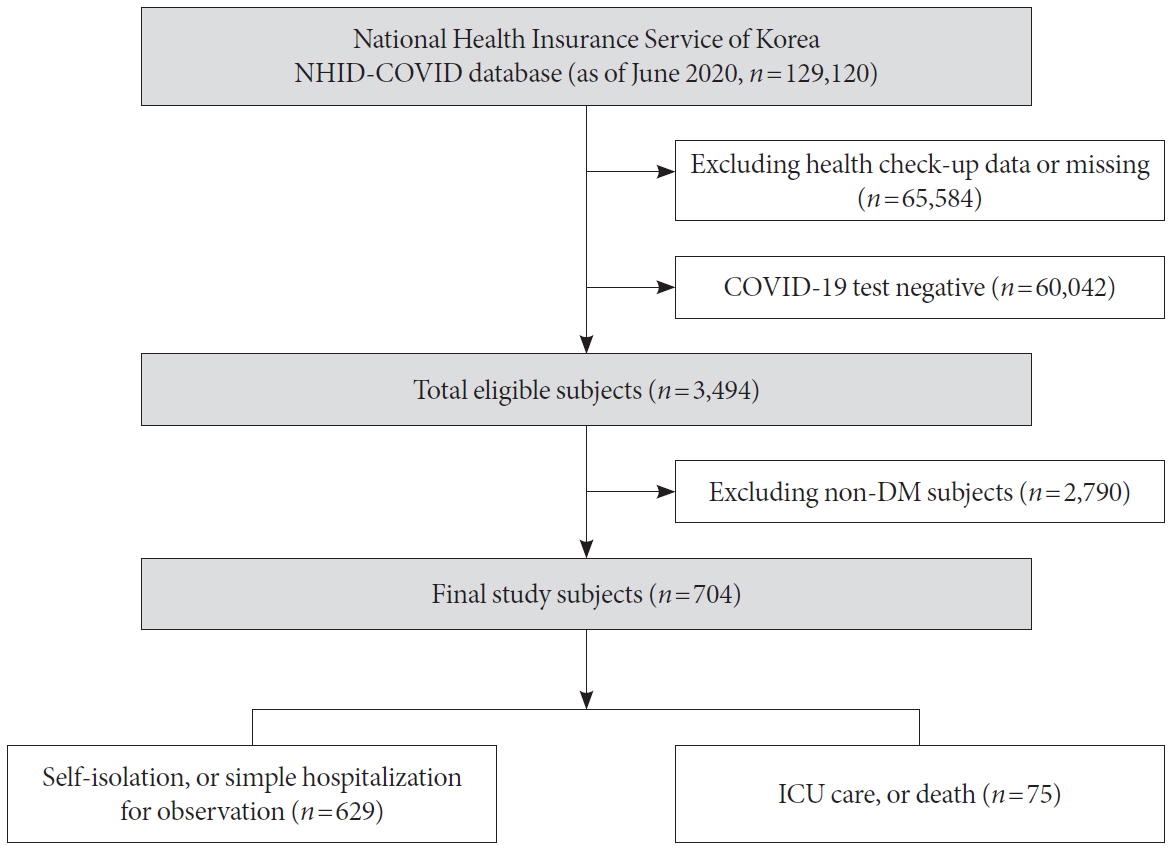
As of May 2020, analysis was conducted on all subjects who could confirm their history of claims related to COVID-19 in the National Health Insurance Review and Assessment Service (HIRA) database in Korea. Using this dataset, we compared the short-term prognosis of COVID-19 infection according to the use of DPP-4i and RAS blockade. Additionally, we validated the results using the National Health Insurance Service (NHIS) of Korea dataset.
Results
Totally, data of 67,850 subjects were accessible in the HIRA dataset. Of these, 5,080 were confirmed COVID-19. Among these, 832 subjects with DM were selected for analysis in this study. Among the subjects, 263 (31.6%) and 327 (39.3%) were DPP4i and RAS blockade users, respectively. Thirty-four subjects (4.09%) received intensive care or died. The adjusted odds ratio for severe treatment among DPP-4i users was 0.362 (95% confidence interval [CI], 0.135 to 0.971), and that for RAS blockade users was 0.599 (95% CI, 0.251 to 1.431). These findings were consistent with the analysis based on the NHIS data using 704 final subjects. The adjusted odds ratio for severe treatment among DPP-4i users was 0.303 (95% CI, 0.135 to 0.682), and that for RAS blockade users was 0.811 (95% CI, 0.391 to 1.682).
Conclusion
This study suggests that DPP-4i is significantly associated with a better clinical outcome of patients with COVID-19.
Keyword
Figure
Cited by 4 articles
-
Effects of a DPP-4 Inhibitor and RAS Blockade on Clinical Outcomes of Patients with Diabetes and COVID-19 (
Diabetes Metab J 2021;45:251-9)
Guntram Schernthaner
Diabetes Metab J. 2021;45(4):615-616. doi: 10.4093/dmj.2021.0081.Effects of a DPP-4 Inhibitor and RAS Blockade on Clinical Outcomes of Patients with Diabetes and COVID-19 (
Diabetes Metab J 2021;45:251-9)
Sang Youl Rhee
Diabetes Metab J. 2021;45(4):619-620. doi: 10.4093/dmj.2021.0118.Diabetes, Obesity, and COVID-19
Sang Youl Rhee
J Korean Diabetes. 2021;22(3):174-178. doi: 10.4093/jkd.2021.22.3.174.Glucose-Lowering Agents and COVID-19
Ah Reum Khang
J Korean Diabetes. 2022;23(1):1-6. doi: 10.4093/jkd.2022.23.1.1.
Reference
-
1. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020; 382:1708–20.
Article2. Guan WJ, Liang WH, Zhao Y, Liang HR, Chen ZS, Li YM, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020; 55:2000547.
Article3. Guo W, Li M, Dong Y, Zhou H, Zhang Z, Tian C, et al. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metab Res Rev. 2020; 36:e3319.
Article4. Rhee EJ, Kim JH, Moon SJ, Lee WY. Encountering COVID-19 as endocrinologists. Endocrinol Metab (Seoul). 2020; 35:197–205.
Article5. Won KC, Yoon KH. The outbreak of COVID-19 and diabetes in Korea: “we will find a way as we have always done”. Diabetes Metab J. 2020; 44:211–2.
Article6. Moon SJ, Rhee EJ, Jung JH, Han KD, Kim SR, Lee WY, et al. Independent impact of diabetes on the severity of coronavirus disease 2019 in 5,307 patients in South Korea: a nationwide cohort study. Diabetes Metab J. 2020; 44:737–46.
Article7. Noh J, Chang HH, Jeong IK, Yoon KH. Coronavirus disease 2019 and diabetes: the epidemic and the Korean Diabetes Association perspective. Diabetes Metab J. 2020; 44:372–81.
Article8. Drucker DJ. Coronavirus infections and type 2 diabetes-shared pathways with therapeutic implications. Endocr Rev. 2020; 41:bnaa011.
Article9. Guo J, Huang Z, Lin L, Lv J. Coronavirus disease 2019 (COVID-19) and cardiovascular disease: a viewpoint on the potential influence of angiotensin-converting enzyme inhibitors/angiotensin receptor blockers on onset and severity of severe acute respiratory syndrome coronavirus 2 infection. J Am Heart Assoc. 2020; 9:e016219.
Article10. Deacon CF. Physiology and pharmacology of DPP-4 in glucose homeostasis and the treatment of type 2 diabetes. Front Endocrinol (Lausanne). 2019; 10:80.
Article11. Batlle D, Jose Soler M, Ye M. ACE2 and diabetes: ACE of ACEs? Diabetes. 2010; 59:2994–6.
Article12. Oudit GY, Crackower MA, Backx PH, Penninger JM. The role of ACE2 in cardiovascular physiology. Trends Cardiovasc Med. 2003; 13:93–101.
Article13. Gaddam RR, Chambers S, Bhatia M. ACE and ACE2 in inflammation: a tale of two enzymes. Inflamm Allergy Drug Targets. 2014; 13:224–34.
Article14. Tomovic K, Lazarevic J, Kocic G, Deljanin-Ilic M, Anderluh M, Smelcerovic A. Mechanisms and pathways of anti-inflammatory activity of DPP-4 inhibitors in cardiovascular and renal protection. Med Res Rev. 2019; 39:404–22.
Article15. Iacobellis G. COVID-19 and diabetes: can DPP4 inhibition play a role? Diabetes Res Clin Pract. 2020; 162:108125.
Article16. Meng J, Xiao G, Zhang J, He X, Ou M, Bi J, et al. Renin-angiotensin system inhibitors improve the clinical outcomes of COVID-19 patients with hypertension. Emerg Microbes Infect. 2020; 9:757–60.
Article17. Solerte SB, D’Addio F, Trevisan R, Lovati E, Rossi A, Pastore I, et al. Sitagliptin treatment at the time of hospitalization was associated with reduced mortality in patients with type 2 diabetes and COVID-19: a multicenter, case-control, retrospective, observational study. Diabetes Care. 2020; 43:2999–3006.
Article18. Messerli FH, Siontis GCM, Rexhaj E. COVID-19 and renin angiotensin blockers: current evidence and recommendations. Circulation. 2020; 141:2042–4.19. Kim JA, Yoon S, Kim LY, Kim DS. Towards actualizing the value potential of Korea Health Insurance Review and Assessment (HIRA) data as a resource for health research: strengths, limitations, applications, and strategies for optimal use of HIRA data. J Korean Med Sci. 2017; 32:718–28.
Article20. Shin DW, Cho B, Guallar E. Korean National Health Insurance database. JAMA Intern Med. 2016; 176:138.
Article21. Ministry of Health and Welfare. Korea Health Insurance Review and Assessment: #opendata4covid19. Available from: https://hira-covid19.net (cited 2021 Jan 19).22. Park SY, Jeong SJ, Ustulin M, Chon S, Woo JT, Lim JE, et al. Incidence of diabetes mellitus in male moderate alcohol drinkers: a community-based prospective cohort study. Arch Med Res. 2019; 50:315–23.23. Rhee SY, Han KD, Kwon H, Park SE, Park YG, Kim YH, et al. Association between glycemic status and the risk of Parkinson disease: a nationwide population-based study. Diabetes Care. 2020; 43:2169–75.
Article24. Raj VS, Mou H, Smits SL, Dekkers DH, Muller MA, Dijkman R, et al. Dipeptidyl peptidase 4 is a functional receptor for the emerging human coronavirus-EMC. Nature. 2013; 495:251–4.
Article25. Yang L, Yuan J, Zhou Z. Emerging roles of dipeptidyl peptidase 4 inhibitors: anti-inflammatory and immunomodulatory effect and its application in diabetes mellitus. Can J Diabetes. 2014; 38:473–9.
Article26. Aroor A, McKarns S, Nistala R, DeMarco V, Gardner M, Garcia-Touza M, et al. DPP-4 inhibitors as therapeutic modulators of immune cell function and associated cardiovascular and renal insulin resistance in obesity and diabetes. Cardiorenal Med. 2013; 3:48–56.
Article27. Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015; 373:2117–28.
Article28. Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Bonaca MP, et al. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet. 2019; 393:31–9.
Article29. ClinicalTrial.gov: Dapagliflozin in respiratory failure in patients with COVID-19 (DARE-19). Available from: https://clinicaltrials.gov/ct2/show/NCT04350593 (cited 2021 Jan 19).30. Goldenberg RM, Berard LD, Cheng AYY, Gilbert JD, Verma S, Woo VC, et al. SGLT2 inhibitor-associated diabetic ketoacidosis: clinical review and recommendations for prevention and diagnosis. Clin Ther. 2016; 38:2654–64.
Article31. Lupsa BC, Inzucchi SE. Use of SGLT2 inhibitors in type 2 diabetes: weighing the risks and benefits. Diabetologia. 2018; 61:2118–25.
Article32. Diaz JH. Hypothesis: angiotensin-converting enzyme inhibitors and angiotensin receptor blockers may increase the risk of severe COVID-19. J Travel Med. 2020; 27:taaa041.
Article33. Kuba K, Imai Y, Rao S, Gao H, Guo F, Guan B, et al. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat Med. 2005; 11:875–9.
Article34. Vaduganathan M, Vardeny O, Michel T, McMurray JJV, Pfeffer MA, Solomon SD. Renin-angiotensin-aldosterone system inhibitors in patients with COVID-19. N Engl J Med. 2020; 382:1653–9.
Article35. Gurwitz D. Angiotensin receptor blockers as tentative SARS-CoV-2 therapeutics. Drug Dev Res. 2020; 81:537–40.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of a DPP-4 Inhibitor and RAS Blockade on Clinical Outcomes of Patients with Diabetes and COVID-19 (Diabetes Metab J 2021;45:251-9)
- Effects of a DPP-4 Inhibitor and RAS Blockade on Clinical Outcomes of Patients with Diabetes and COVID-19 (Diabetes Metab J 2021;45:251-9)
- Dipeptidyl Peptidase-4 Inhibitors and COVID-19-Related Deaths among Patients with Type 2 Diabetes Mellitus: A Meta-Analysis of Observational Studies
- Hypertension and Electrolyte Disorders in Patients with COVID-19
- Glucose-Lowering Agents and COVID-19