Clin Endosc.
2021 Mar;54(2):280-284. 10.5946/ce.2020.117.
Fatal Necrotizing Fasciitis Following Uncomplicated Colonoscopic Polypectomy: A Case Report
- Affiliations
-
- 1Department of Internal Medicine, Kyung Hee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea
- KMID: 2514185
- DOI: http://doi.org/10.5946/ce.2020.117
Abstract
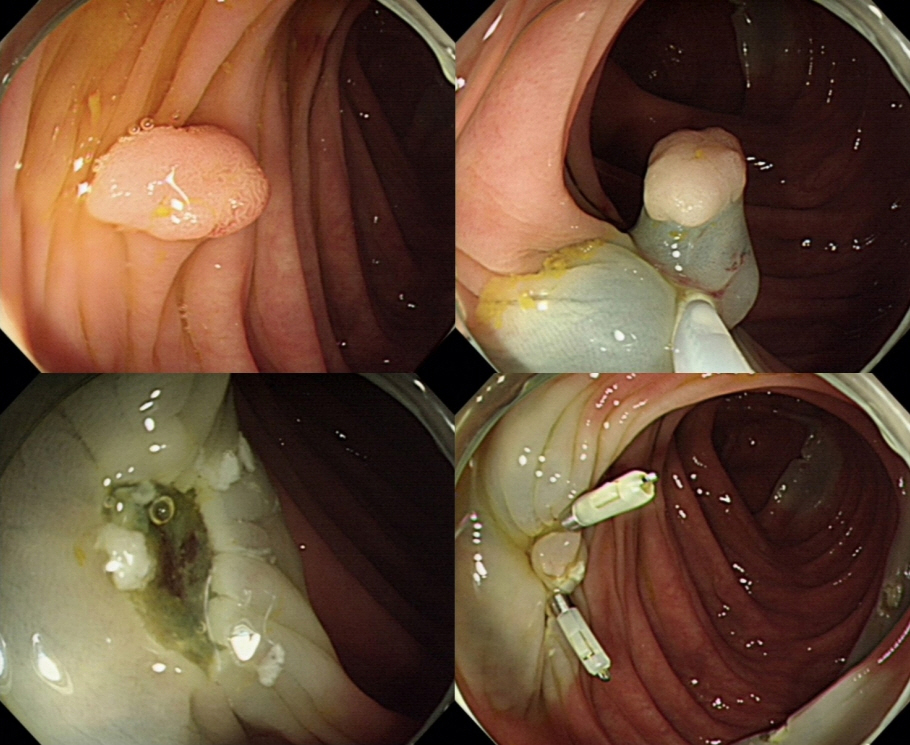
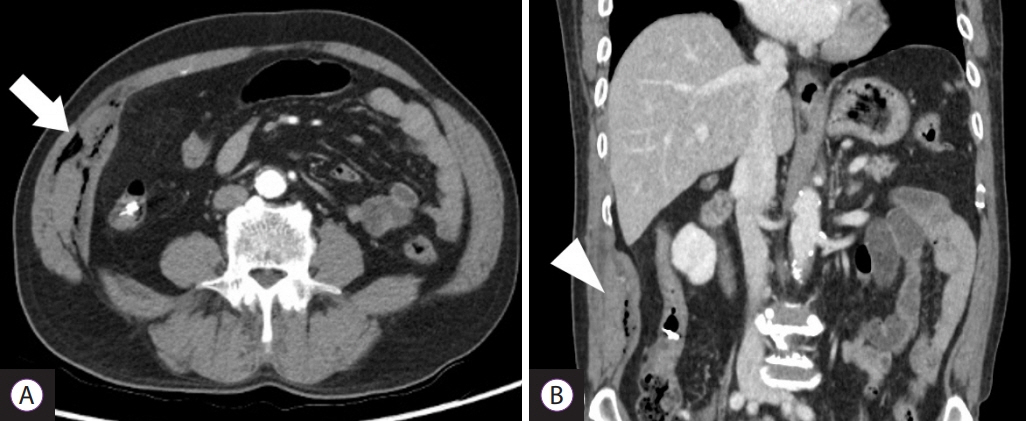
- Necrotizing fasciitis (NF) is a life-threatening infection that can be caused by various procedures or surgery and may develop in healthy elderly patients. Here, we report a case of a 66-year-old man with diabetes mellitus who underwent colonoscopic polypectomy, without complications. However, he visited the emergency department 24 hours after the procedure complaining of abdominal pain. Abdominopelvic computed tomography revealed multiple air bubbles in the right lateral abdominal muscles. After a diagnosis of NF was made, immediate surgical debridement was performed. However, despite three sessions of extensive surgical debridement and best supportive care at the intensive care unit, the patient died because of sepsis and NF-associated multiple-organ failure. In conclusion, physicians should pay special attention to the possibility of NF if a patient with risk factors for NF develops sepsis after colonoscopic polypectomy.
Keyword
Figure
Reference
-
1. Aronoff DM, Bloch KC. Assessing the relationship between the use of nonsteroidal antiinflammatory drugs and necrotizing fasciitis caused by group A streptococcus. Medicine (Baltimore). 2003; 82:225–235.
Article2. Stevens DL, Bryant AE. Necrotizing soft-tissue infections. N Engl J Med. 2017; 377:2253–2265.
Article3. Misiakos EP, Bagias G, Patapis P, Sotiropoulos D, Kanavidis P, Machairas A. Current concepts in the management of necrotizing fasciitis. Front Surg. 2014; 1:36.
Article4. Lamagni TL, Darenberg J, Luca-Harari B, et al. Epidemiology of severe streptococcus pyogenes disease in Europe. J Clin Microbiol. 2008; 46:2359–2367.5. Huang KF, Hung MH, Lin YS, et al. Independent predictors of mortality for necrotizing fasciitis: a retrospective analysis in a single institution. J Trauma. 2011; 71:467–473. discussion 473.
Article6. Wong CH, Chang HC, Pasupathy S, Khin LW, Tan JL, Low CO. Necrotizing fasciitis: clinical presentation, microbiology, and determinants of mortality. J Bone Joint Surg Am. 2003; 85:1454–1460.7. Anaya DA, McMahon K, Nathens AB, Sullivan SR, Foy H, Bulger E. Predictors of mortality and limb loss in necrotizing soft tissue infections. Arch Surg. 2005; 140:151–157. discussion 158.
Article8. Orlando A, Marrone C, Nicoli N, et al. Fatal necrotising fasciitis associated with intramuscular injection of nonsteroidal anti-inflammatory drugs after uncomplicated endoscopic polypectomy. J Infect. 2007; 54:e145–e148.
Article9. Frick S, Cerny A. Necrotizing fasciitis due to streptococcus pneumoniae after intramuscular injection of nonsteroidal anti-inflammatory drugs: report of 2 cases and review. Clin Infect Dis. 2001; 33:740–744.10. MacLean AA, Miller G, Bamboat ZM, Hiotis K. Abdominal wall necrotizing fasciitis from dislodged percutaneous endoscopic gastrostomy tubes: a case series. Am Surg. 2004; 70:827–831.11. Calderon E, Carter E, Ramsey KM, Vande Waa JA, Green WK, Alpert MA. Necrotizing fasciitis: a complication of percutaneous coronary revascularization. Angiology. 2007; 58:360–366.
Article12. Nouira K, Bourkhis S, Maalej S, et al. [Necrotizing fasciitis complicating transthoracic biopsy]. Rev Pneumol Clin. 2007; 63:273–276.13. Pryor JP, Piotrowski E, Seltzer CW, Gracias VH. Early diagnosis of retroperitoneal necrotizing fasciitis. Crit Care Med. 2001; 29:1071–1073.
Article14. Devin B, McCarthy A, Mehran R, Auger C. Necrotizing fasciitis of the retroperitoneum: an unusual presentation of group A streptococcus infection. Can J Surg. 1998; 41:156–160.15. Sarani B, Strong M, Pascual J, Schwab CW. Necrotizing fasciitis: current concepts and review of the literature. J Am Coll Surg. 2009; 208:279–288.
Article16. Zacharias N, Velmahos GC, Salama A, et al. Diagnosis of necrotizing soft tissue infections by computed tomography. Arch Surg. 2010; 145:452–455.
Article17. Anaya DA, Dellinger EP. Necrotizing soft-tissue infection: diagnosis and management. Clin Infect Dis. 2007; 44:705–710.18. Ryssel H, Germann G, Kloeters O, Radu CA, Reichenberger M, Gazyakan E. Necrotizing fasciitis of the extremities: 34 cases at a single centre over the past 5 years. Arch Orthop Trauma Surg. 2010; 130:1515–1522.19. Leiblein M, Marzi I, Sander AL, Barker JH, Ebert F, Frank J. Necrotizing fasciitis: treatment concepts and clinical results. Eur J Trauma Emerg Surg. 2018; 44:279–290.
Article20. Cheng NC, Tai HC, Chang SC, Chang CH, Lai HS. Necrotizing fasciitis in patients with diabetes mellitus: clinical characteristics and risk factors for mortality. BMC Infect Dis. 2015; 15:417.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fatal Necrotizing Fasciitis Due to Pseudomonas aeruginosa After Vaccination : A Case Report
- Fatal Necrotizing Fasciitis Due to Streptococcus pneumoniae: A Case Report
- A Case of Necrotizing Fasciitis and Severe Sepsis Complicated by Emphysematous Gastritis
- A case of necrotizing fasciitis of the abdominal wall complicating a renal biopsy
- Cranio-Cervico-facial Necrotizing fasciitis