Ann Pediatr Endocrinol Metab.
2021 Mar;26(1):19-23. 10.6065/apem.2040170.085.
Complete androgen insensitivity syndrome and risk of gonadal malignancy: systematic review
- Affiliations
-
- 1Interdisciplinary Group for the Study of Sex Determination and Differentiation (GIEDDS), State University of Campinas (UNICAMP), Campinas/São Paulo, Brazil
- 2Department of Pediatrics, State University of Campinas (UNICAMP), Campinas/São Paulo, Brazil
- 3Department of Pediatrics, Federal University of Uberlândia (UFU), Uberlândia/Minas Gerais, Brazil
- 4Department of Medical Genetics, State University of Campinas (UNICAMP), Campinas/São Paulo, Brazil
- KMID: 2514148
- DOI: http://doi.org/10.6065/apem.2040170.085
Abstract
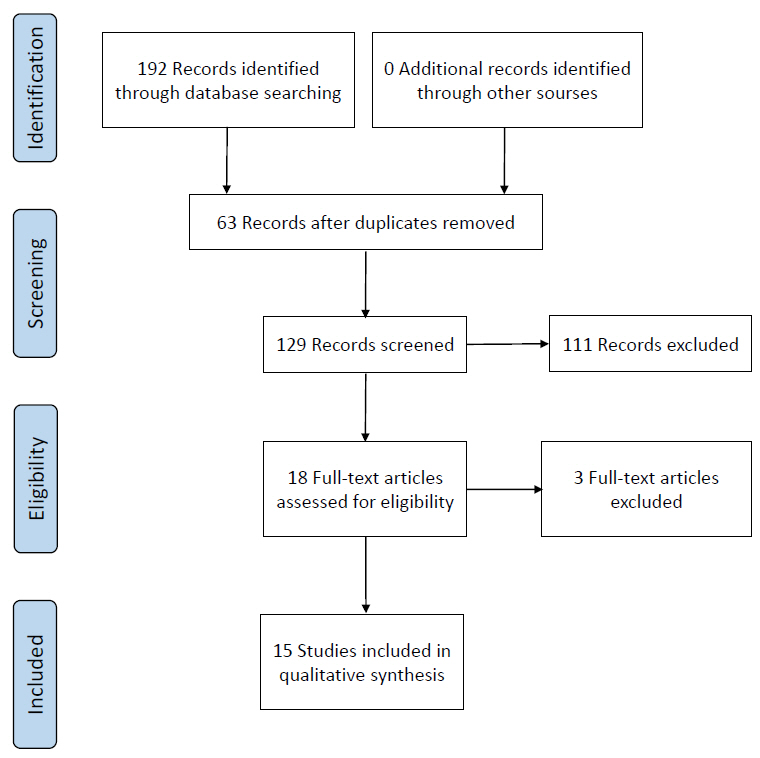
- Complete androgen insensitivity syndrome (CAIS) is a rare condition characterized by 46,XY karyotype, female external genitalia, absence of uterus, and testes located intra-abdominally, in the inguinal ring or in the labia majora. In the present study, the frequency of testicular malignancy in prepubertal and pubertal patients with CAIS who underwent gonadectomy or gonadal biopsy were evaluated. Systematic review was performed using electronic databases according to the PRISMA-P (Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols) guidelines. The samples included 15 articles published between 1998 and 2019. From a total of 456 patients who underwent gonadectomy or gonadal biopsy, 6.14% had a premalignant lesion and most were postpubertal (82.14%). A malignant lesion was found in 1.3% and all were postpubertal. Because the risk of malignancy is very low in prepubertal patients with CAIS, gonadectomy may be delayed until puberty is complete, allowing it to progress naturally; however, close follow-up of the patient is required.
Figure
Reference
-
References
1. Oakes MB, Eyvazzadeh AD, Quint E, Smith YR. Complete androgen insensitivity syndrome – a review. J Pediatr Adolesc Gynecol. 2008; 21:305–10.2. Mongan NP, Tadokoro-Cuccaro R, Bunch T, Hughes IA. Androgen Insensitivity Syndrome. Best Pract Res Clin Endocrinol Metab. 2015; 29:569–80.
Article3. Hannema SE, Scott IS, Rajpert-De Meyts E, Skakkebæk NE, Coleman N, Hughes IA. Testis development in the complete androgen insensitivity syndrome. J Pathol. 2006; 208:518–27.4. Cools M, Drop SL, Wolffenbuttel KP, Oosterhuis JW, Looijenga LH. Germ cell tumors in the intersex gonad: old paths, new directions, moving frontiers. Endocr Rev. 2006; 27:468–84.
Article5. Chaudhry S, Tadokoro-Cuccaro R, Hannema SE, Acerini CL, Hughes IA. Frequency of gonadal tumours in complete androgen insensitivity syndrome (CAIS): a retrospective case-series analysis. J Pediatr Urol. 2017; 13:498.
Article6. Gidekel S, Pizov G, Bergman Y, Pikarsky E. Oct-3/4 is a dose-dependent oncogenic fate determinant. Cancer Cell. 2003; 4:361–70.
Article7. Deans R, Creighton SM, Liao LM, Conway GS. Timing of gonadectomy in adult women with complete androgen insensitivity syndrome (CAIS): patient preferences and clinical evidences. Clin Endocrinol. 2012; 76:894–8.8. Döhnert U, Wünsch L, Hiort O. Gonadectomy in complete androgen insensitivity syndrome: why and when? Sex Dev. 2017; 11:171–4.
Article9. Lee PA, Nordenström A, Houk CP, Ahmed SF, Auchus R, Baratz A, et al. Global disorders of sex development update since 2006: perceptions, approach and care. Horm Res Paediatr. 2016; 85:158–80.
Article10. Moher D, Liberati A, Tetzlaff J, Altman DG; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLoS Med. 2009; 6:e1000097.
Article11. Kriplani A, Abbi M, Ammini AC, Kriplani AK, Kucheria K, Tak kar K. L aparos copic gonadectomy in male pseudohermaphrodites. Eur J Obstet Gynecol Reprod Biol. 1998; 81:37–41.12. Ahmed SF, Cheng A, Dovey L, Hawkins JR, Martin H, Rowland J. Phenotypic features, androgen receptor binding, and mutational analysis in 278 clinical cases reported as androgen insensitivity syndrome. J Clin Endocrinol Metab. 2000; 85:658–65.
Article13. Yalinkaya A, Yayla M. Laparoscopy-assisted transinguinal extracorporeal gonadectomy in six patients with Androgen Insensitivity Syndrome. Fertil Steril. 2003; 80:429–33.
Article14. Cools M, van Aerde K, Kersemaekers AMF, Boter M, Drop SL, Wolffenbuttel KP, et al. Morphological and immunohistochemical differences between gonadal maturation delay and early germ cell neoplasia in patients with undervirilization syndromes. J Clin Endocrinol Metab. 2005; 90:5295–303.
Article15. Cheikhelard A, Morel Y, Thibaud E, Lortat-Jacob S, Jaubert F, Polak M, et al. Long-term follow-up and comparison between genotype and phenotype in 29 cases of Complete Androgen Insensitivity Syndrome. J Urol. 2008; 180:1496–501.
Article16. Purves JT, Miles-Thomas J, Migeon C, Gearhart JP. Complete androgen insensitivity: the role of the surgeon. J Urol. 2008; 180:1716–9.
Article17. Kravarusic D, Seguier-Lipszyc E, Feigin E, Nimri R, Nagelberg N, Freud E. Androgen insensitivity syndrome: risk of malignancy and timing of surgery in a paediatric and adolescent population. Afr J Paediatr Surg. 2011; 8:194–8.
Article18. Dobanovacki D, Jokic RR, Vuckovic N, Privrodski JDJ, Katanic DJ, Tatic MR, et al. Complete androgen insensitivity syndrome: review of four cases. Cent Eur J Med. 2012; 7:729–32.
Article19. Wünsch L, Holterhus PM, Wessel L, Hiort O. Patients with disorders of sex development (DSD) at risk of gonadal tumour development: management based on laparoscopic biopsy and molecular diagnosis. BJU Int. 2012; 110:E958–65.
Article20. Esposito C, Escolino M, Bagnara V, Eckoldt-Wolke F, Baglaj M, Saxena A, et al. Risk of malignancy and need of surgery in pediatric patients with Morris or Y-chromosome Turner: a multicenter survey. J Pediatr Adolesc Gynecol. 2015; 28:333–6.21. Liu AX, Shi HY, Cai ZJ, Liu A, Zhang D, Huang HF, et al. Increased risk of gonadal malignancy and prophylactic gonadectomy: a study of 102 phenotypic female patients with Y chromosome or Y-derived sequences. Hum Reprod. 2014; 29:1413–9.
Article22. Wang Z, Sa YL, Ye XX, Zhang J, Xu YM. Complete Androgen Insensitivity Syndrome in juveniles and adults with female phenotypes. J Obstet Gynaecol Res. 2014; 40:2044–50.
Article23. Tian Q. Gonadal tumour risk in 292 phenotypic female patients with Disorders of Sex Development containing Y chromosome or Y-derived sequence. Clin Endocrinol. 2017; 86:621–7.
Article24. Countant R, de Casson FB, Rouleau S, Douay O, Mathieu E, Gatelais F, et al. Divergent effect of endogenous and exogenous sex steroids on the insulin like growth factor response to growth hormone in short normal adolescents. J Clin Endocrinol Metab. 2004; 89:6185–92.25. Perry RJ, Farquharson T, Ahmed SF. The role of sex steroids in controlling pubertal growth. Clin Endocrinol. 2008; 68:4–15.
Article26. Ferlin A, Selice R, Carraro U, Foresta C. Testicular function and bone metabolism – beyond testosterone. Nat Rev Endocrinol. 2013; 9:548–54.
Article27. Tack LJW, Maris E, Looijenga LHJ, Hannema SE, Audi L, Köhler B, et al. Management of gonads in adults with androgen insensitivity: an International survey. Horm Res Paediatr. 2018; 90:236–46.
Article28. Wisniewski AB, Migeon CJ, Meyer-Bahlburg HFL, Gearhart JP, Berkovitz GD, Brown TR, et al. Complete androgen insensitivity syndrome: long-term medical, surgical, and psychosexual outcome. J Clin Endocrinol Metab. 2000; 85:2664–9.
Article29. Slowikowska-Hilczer J, Romer TE, Kula K. Neoplastic potential of germ cells in relation to disturbances of gonadal organogenesis and changes in karyotype. J Androl. 2013; 24:270–8.
Article30. Jones TD, Ulbright TM, Eble JN, Baldridge LA, Cheng L. OCT4 staining in testicular tumors: a sensitive and specific marker for seminoma and embryonal carcinoma. Am J Surg Pathol. 2004; 28:935–40.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Laparoscopic Gonadectomy in Complete Androgen Insensitivity Syndrome
- Pelviscopic Gonadectomy in two cases of Complete Androgen Insensitivity Syndrome
- A Case Report of Complete Androgen Insensitivity Syndrome
- Female with 46, XY karyotype
- A Case of Complete Androgen Insensitivity Syndrome with Bilateral Inguinal Gonads