J Rhinol.
2021 Mar;28(1):61-65. 10.18787/jr.2020.00340.
Resection of Ewing Sarcoma in the Paranasal Sinus Via the Endoscopic Modified Lothrop (Draf III) Approach
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Korea University, College of Medicine, Seoul, Korea
- KMID: 2513845
- DOI: http://doi.org/10.18787/jr.2020.00340
Abstract
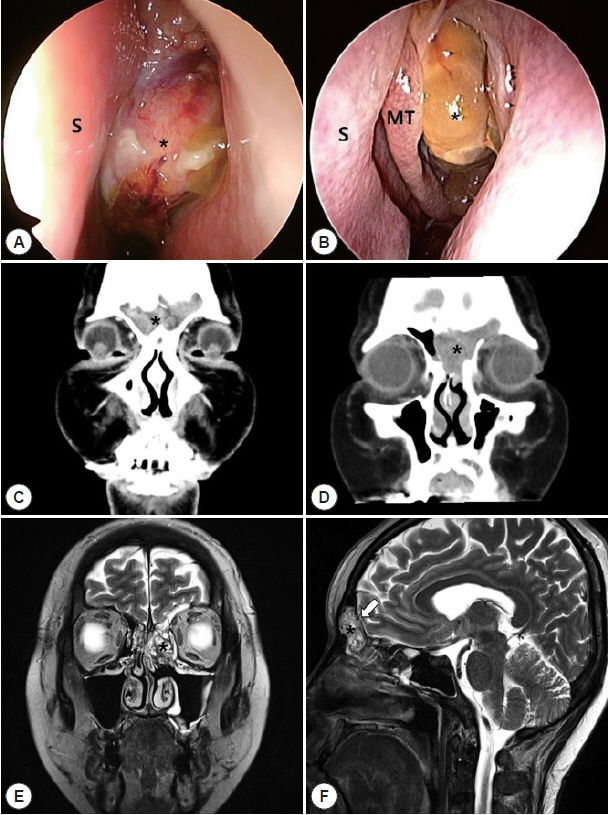
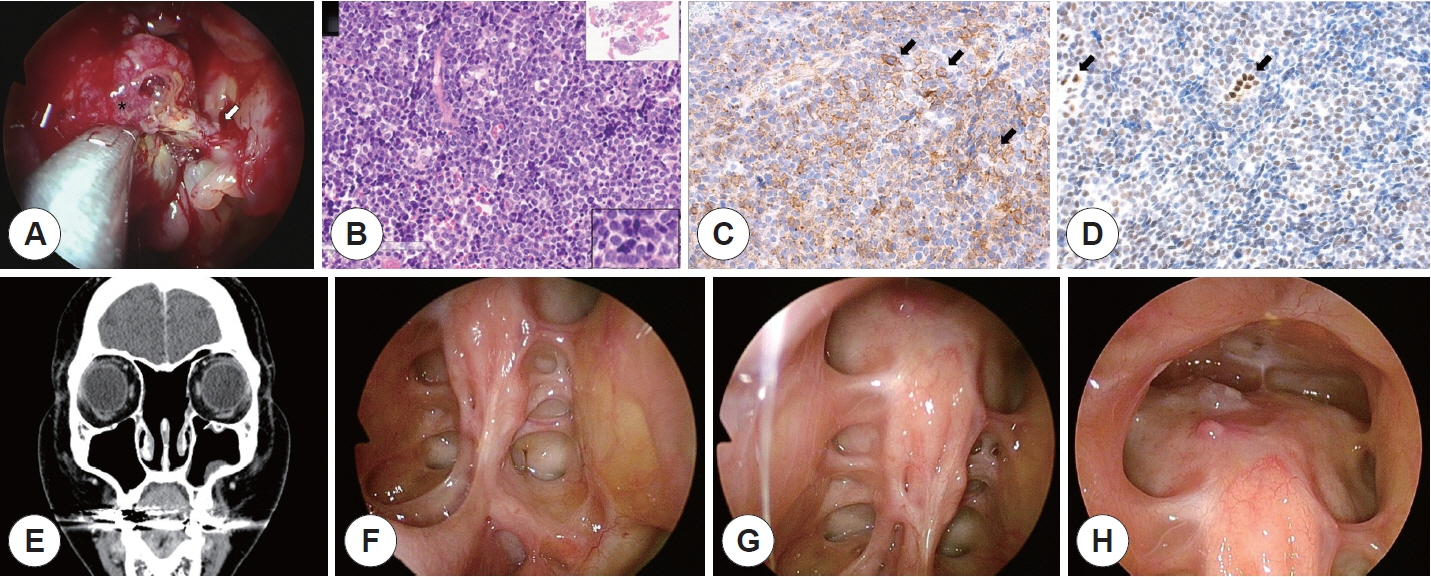
- Ewing sarcoma is a rare type of bone tumor that typically occurs in the head and neck regions. Appropriate management strategies remain controversial. Herein, we report a case of Ewing sarcoma originating from the ethmoid sinus in a 38-year-old woman. The patient initially presented with unilateral nasal obstruction. Pathologic examination revealed a tumor composed of small round blue cells under hematoxylin and eosin staining with positive expressions for CD-99, CK, and FLI-1. The patient was successfully treated with neoadjuvant chemotherapy followed by complete surgical excision via the endoscopic modified Lothrop (Draf III) approach, adjuvant chemotherapy, and radiation therapy. There was no recurrence or complication up to the writing of this article. This study presents an appropriate management strategy for an extensive case of Ewing sarcoma invading the frontal sinus using an endoscopic approach.
Figure
Reference
-
References
1. Whaley JT, Indelicato DJ, Morris CG, Hinerman RW, Amdur RJ, Mendenhall WM, et al. Ewing tumors of the head and neck. Am J Clin Oncol. 2010; 33(4):321–6.2. Vaccani JP, Forte V, de Jong AL, Taylor G. Ewing’s sarcoma of the head and neck in children. International Journal of Pediatric Otorhinolaryngology. 1999; 48(3):209–16.3. Sripathi Rao B, Rai G, Hassan S, Nadaf A. Ewing’s sarcoma of the mandible. National Journal of Maxillofacial Surgery. 2011; 2(2):184–8.4. Peersman B, Vanhoenacker FM, Heyman S, Herendael BV, Stam M, Brys P, et al. Ewing’s sarcoma: imaging features. JBR-BTR. 2007; 90(5):368–76.5. Desai SS, Jambhekar NA. Pathology of Ewing’s sarcoma/PNET: Current opinion and emerging concepts. Indian J Orthop. 2010; 44(4):363–8.6. Bailey K, Cost C, Davis I, Glade-Bender J, Grohar P, Houghton P, et al. Emerging novel agents for patients with advanced Ewing sarcoma: a report from the Children’s Oncology Group (COG) New Agents for Ewing Sarcoma Task Force. F1000Res. 2019; 8.7. Burchill SA. Ewing’s sarcoma: diagnostic, prognostic, and therapeutic implications of molecular abnormalities. J Clin Pathol. 2003; 56(2):96–102.8. kovar h, amatruda j, brunet e, burdach s, cidre-aranaz f, enrique de alava e, et al. the second european interdisciplinary ewing sarcoma research summit--a joint effort to deconstructing the multiple layers of a complex disease. oncotarget. 2016; 7(8):8613–24.9. Ferguson JL, Turner SP. Bone Cancer: Diagnosis and Treatment Principles. American Family Physician. 2018; 98(4):205–13.10. Shen J, Chan N, Wrobel BB. The endoscopic modified lothrop procedure: Review of single institution experience and long-term outcomes. Laryngoscope Investigative Otolaryngology. 2018; 3(2):105–9.11. Agrawal A, Dulani R, Mahadevan A, Vagaha SJ, Vagha J, Shankar SK. Primary Ewing’s sarcoma of the frontal bone with intracranial extension. Journal of Cancer Research and Therapeutics. 2009; 5(3):208–9.12. Alobid I, Bernal-Sprekelsen M, Alós L, Benítez P, Traserra J, Mullol J. Peripheral primitive neuroectodermal tumour of the left maxillary sinus. Acta Oto-Laryngologica. 2003; 123(6):776–8.13. Thariat J, Italiano A, Peyrade F, Birtwisle-Peyrottes I, Gastaud L, Dassonville O, et al. Very Late Local Relapse of Ewing’s Sarcoma of the Head and Neck treated with Aggressive Multimodal Therapy. Sarcoma. 2008; 2008:854141.14. Lepera D, Volpi L, Facco C, Turri-Zanoni M, Battaglia P, Bernasconi B, et al. Endoscopic Treatment of Ewing Sarcoma of the Sinonasal Tract. The Journal of Craniofacial Surgery. 2016; 27(4):1001–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Extended Draf IIb Procedures in the Treatment of Frontal Sinus Pathology
- Frontal Sinus Stenting in Endoscopic Sinus Surgery
- Resection of Impacted Bilateral Huge Frontal Osteoma Via Endoscopic Modified Lothrop Approach
- Extraskeletal Primary Ewing's Sarcoma in the Nasal Cavity: A Case Report
- Primary Intradural Extraosseous Ewing's Sarcoma