J Korean Med Sci.
2021 Mar;36(8):e51. 10.3346/jkms.2021.36.e51.
Prognostic Implications of CT Feature Analysis in Patients with COVID-19: a Nationwide Cohort Study
- Affiliations
-
- 1Department of Radiology and Biomedical Research Institute, Pusan National University Hospital, Busan, Korea
- 2Department of radiology, Soonchunhyang University College of Medicine, Soonchunhyang University Seoul Hospital, Seoul, Korea
- 3Department of Radiology, Chungbuk National University Hospital, Cheongju, Korea
- 4Department of Radiology, Pusan National University Yangsan Hospital, Yangsan, Korea
- 5Department of Radiology, Kosin University Gospel Hospital, Busan, Korea
- 6Department of Radiology, Chonnam National University Hospital, Gwangju, Korea
- 7Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2513530
- DOI: http://doi.org/10.3346/jkms.2021.36.e51
Abstract
- Background
Few studies have classified chest computed tomography (CT) findings of coronavirus disease 2019 (COVID-19) and analyzed their correlations with prognosis. The present study aimed to evaluate retrospectively the clinical and chest CT findings of COVID-19 and to analyze CT findings and determine their relationships with clinical severity.
Methods
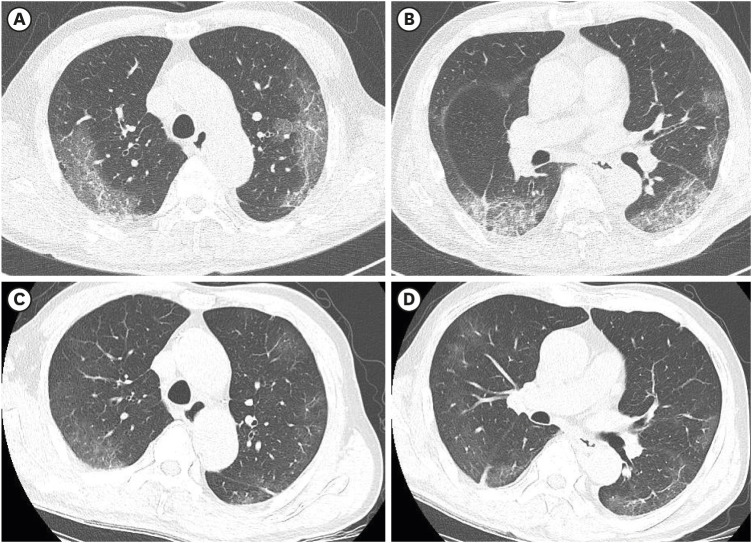
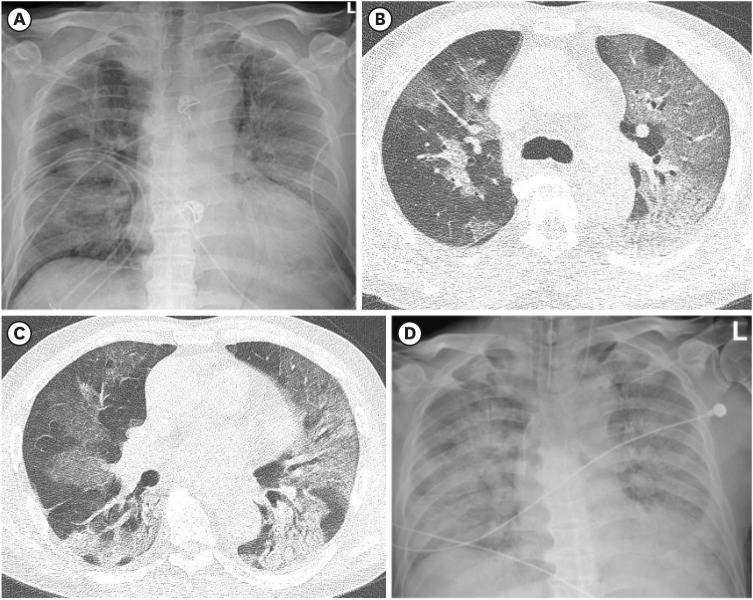
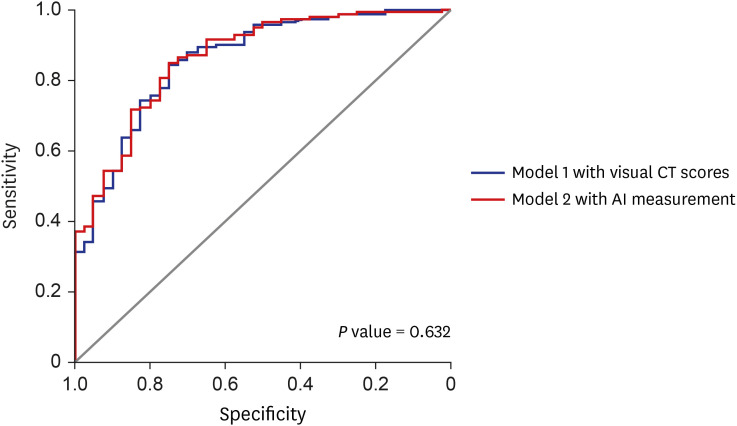
Chest CT and clinical features of 271 COVID-19 patients were assessed. The presence of CT findings and distribution of parenchymal abnormalities were evaluated, and CT patterns were classified as bronchopneumonia, organizing pneumonia (OP), or diffuse alveolar damage (DAD). Total extents were assessed using a visual scoring system and artificial intelligence software. Patients were allocated to two groups based on clinical outcomes, that is, to a severe group (requiring O2 therapy or mechanical ventilation, n = 55) or a mild group (not requiring O2 therapy or mechanical ventilation, n = 216). Clinical and CT features of these two groups were compared and univariate and multivariate logistic regression analyses were performed to identify independent prognostic factors.
Results
Age, lymphocyte count, levels of C-reactive protein, and procalcitonin were significantly different in the two groups. Forty-five of the 271 patients had normal chest CT findings. The most common CT findings among the remaining 226 patients were groundglass opacity (98%), followed by consolidation (53%). CT findings were classified as OP (93%), DAD (4%), or bronchopneumonia (3%) and all nine patients with DAD pattern were included in the severe group. Uivariate and multivariate analyses showed an elevated procalcitonin (odds ratio [OR], 2.521; 95% confidence interval [CI], 1.001–6.303, P = 0.048), and higher visual CT scores (OR, 1.137; 95% CI, 1.042–1.236; P = 0.003) or higher total extent by AI measurement (OR, 1.048; 95% CI, 1.020–1.076; P < 0.001) were significantly associated with a severe clinical course.
Conclusion
CT findings of COVID-19 pneumonia can be classified into OP, DAD, or bronchopneumonia patterns and all patients with DAD pattern were included in severe group. Elevated inflammatory markers and higher CT scores were found to be significant predictors of poor prognosis in patients with COVID-19 pneumonia.
Keyword
Figure
Reference
-
1. World Health Organization. COVID-19 weekly epidemiological update. Updated 2020. Accessed October 30, 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20201020-weekly-epi-update-10.pdf.2. Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, et al. CT Imaging features of 2019 novel coronavirus (2019-nCoV). Radiology. 2020; 295(1):202–207. PMID: 32017661.3. Pan F, Ye T, Sun P, Gui S, Liang B, Li L, et al. Time course of lung changes at chest CT during recovery from coronavirus disease 2019 (COVID-19). Radiology. 2020; 295(3):715–721. PMID: 32053470.4. Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol. 2020; 215(1):87–93. PMID: 32174129.
Article5. Yoon SH, Lee KH, Kim JY, Lee YK, Ko H, Kim KH, et al. Chest radiographic and CT findings of the 2019 novel coronavirus disease (COVID-19): analysis of nine patients treated in Korea. Korean J Radiol. 2020; 21(4):494–500. PMID: 32100485.
Article6. Lee KS. Pneumonia associated with 2019 novel coronavirus: can computed tomographic findings help predict the prognosis of the disease? Korean J Radiol. 2020; 21(3):257–258. PMID: 32056396.
Article7. Kang H, Lee KS, Jeong YJ, Lee HY, Kim KI, Nam KJ. Computed tomography findings of influenza A (H1N1) pneumonia in adults: pattern analysis and prognostic comparisons. J Comput Assist Tomogr. 2012; 36(3):285–290. PMID: 22592609.8. Yoon SH, Ham SY, Nam BD, Chae KJ, Lee D, Yoo JY, et al. Establishment of a nationwide Korean imaging cohort of coronavirus disease 2019. J Korean Med Sci. 2020; 35(46):e413. PMID: 33258333.
Article9. Jeong YJ, Kim YH. Korean imaging cohort of COVID-19: potential role in education and research. J Korean Soc Radiol. 2020; 81(3):608–609.
Article10. Kipps TJ. Chapter 81. Lymphocytosis and lymphocytopenia. In : Lichtman MA, Kipps TJ, Seligsohn U, Kaushansky K, Prchal JT, editors. Williams Hematology. 8th ed. New York, NY: The McGraw-Hill Companies;2010.11. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020; 323(11):1061–1069. PMID: 32031570.
Article12. Lippi G, Plebani M. Procalcitonin in patients with severe coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chim Acta. 2020; 505:190–191. PMID: 32145275.
Article13. Li K, Wu J, Wu F, Guo D, Chen L, Fang Z, et al. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Invest Radiol. 2020; 55(6):327–331. PMID: 32118615.
Article14. Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner Society: glossary of terms for thoracic imaging. Radiology. 2008; 246(3):697–722. PMID: 18195376.
Article15. Lang M, Som A, Carey D, Reid N, Mendoza DP, Flores EJ, et al. Pulmonary vascular manifestations of COVID-19 pneumonia. Radiol Cardiothorac Imaging. 2020; 2(3):e200277.16. Ajlan AM, Ahyad RA, Jamjoom LG, Alharthy A, Madani TA. Middle East respiratory syndrome coronavirus (MERS-CoV) infection: chest CT findings. AJR Am J Roentgenol. 2014; 203(4):782–787. PMID: 24918624.
Article17. Antonio GE, Ooi CG, Wong KT, Tsui EL, Wong JS, Sy AN, et al. Radiographic-clinical correlation in severe acute respiratory syndrome: study of 1373 patients in Hong Kong. Radiology. 2005; 237(3):1081–1090. PMID: 16304120.
Article18. Das KM, Lee EY, Langer RD, Larsson SG. Middle East respiratory syndrome coronavirus: what does a radiologist need to know? AJR Am J Roentgenol. 2016; 206(6):1193–1201. PMID: 26998804.
Article19. Ketai L, Paul NS, Wong KT. Radiology of severe acute respiratory syndrome (SARS): the emerging pathologic-radiologic correlates of an emerging disease. J Thorac Imaging. 2006; 21(4):276–283. PMID: 17110851.20. Wong KT, Antonio GE, Hui DS, Lee N, Yuen EH, Wu A, et al. Thin-section CT of severe acute respiratory syndrome: evaluation of 73 patients exposed to or with the disease. Radiology. 2003; 228(2):395–400. PMID: 12738877.
Article21. Hosseiny M, Kooraki S, Gholamrezanezhad A, Reddy S, Myers L. Radiology perspective of coronavirus disease 2019 (COVID-19): lessons from severe acute respiratory syndrome and Middle East respiratory syndrome. AJR Am J Roentgenol. 2020; 214(5):1078–1082. PMID: 32108495.
Article22. Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N, et al. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020; 295(3):200463. PMID: 32077789.
Article23. Koo HJ, Lim S, Choe J, Choi SH, Sung H, Do KH. Radiographic and CT features of viral pneumonia. Radiographics. 2018; 38(3):719–739. PMID: 29757717.
Article24. Hall CB. Respiratory syncytial virus and parainfluenza virus. N Engl J Med. 2001; 344(25):1917–1928. PMID: 11419430.
Article25. Hui DS, Memish ZA, Zumla A. Severe acute respiratory syndrome vs. the Middle East respiratory syndrome. Curr Opin Pulm Med. 2014; 20(3):233–241. PMID: 24626235.
Article26. Davarpanah AH, Asgari R, Moharamzad Y, Mahdavi A, Abrishami A, Nekooghadam S, et al. Risk factors for poor outcome in patients with severe viral pneumonia on Chest CT during the COVID-19 outbreak: a perspective from Iran. SN Compr Clin Med. 2020; 1–11.
Article27. Park B, Park J, Lim JK, Shin KM, Lee J, Seo H, et al. Prognostic implication of volumetric quantitative CT analysis in patients with COVID-19: a multicenter study in Daegu, Korea. Korean J Radiol. 2020; 21(11):1256–1264. PMID: 32767868.
Article28. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020; 395(10223):507–513. PMID: 32007143.
Article29. Chon Y, Kim JY, Suh YJ, Lee JY, Park JS, Moon SM, et al. Adverse initial CT findings associated with poor prognosis of coronavirus disease. J Korean Med Sci. 2020; 35(34):e316. PMID: 32864912.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes in Expenditures of the National Health Insurance of Korea during the COVID-19 Pandemic and the Financial Implications Thereof
- Impact of Mediastinal Lymphadenopathy on the Severity of COVID-19 Pneumonia: A Nationwide Multicenter Cohort Study
- Insomnia Disorder Among Coronavirus Disease Survivors: A South Korean Nationwide Cohort Study
- Pulmonary Contusion Similar to COVID-19 Pneumonia
- Prognostic Factors for Survival or Severity After COVID-19 Infection in Cancer Patients: A Systematic Review and Meta-Analysis