Acute Crit Care.
2021 Feb;36(1):75-77. 10.4266/acc.2020.00955.
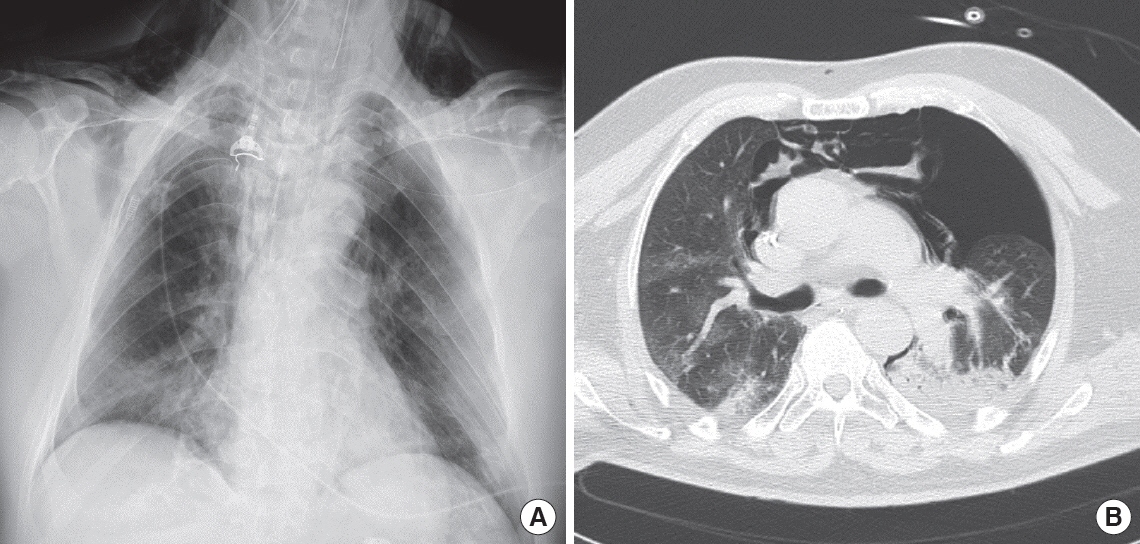
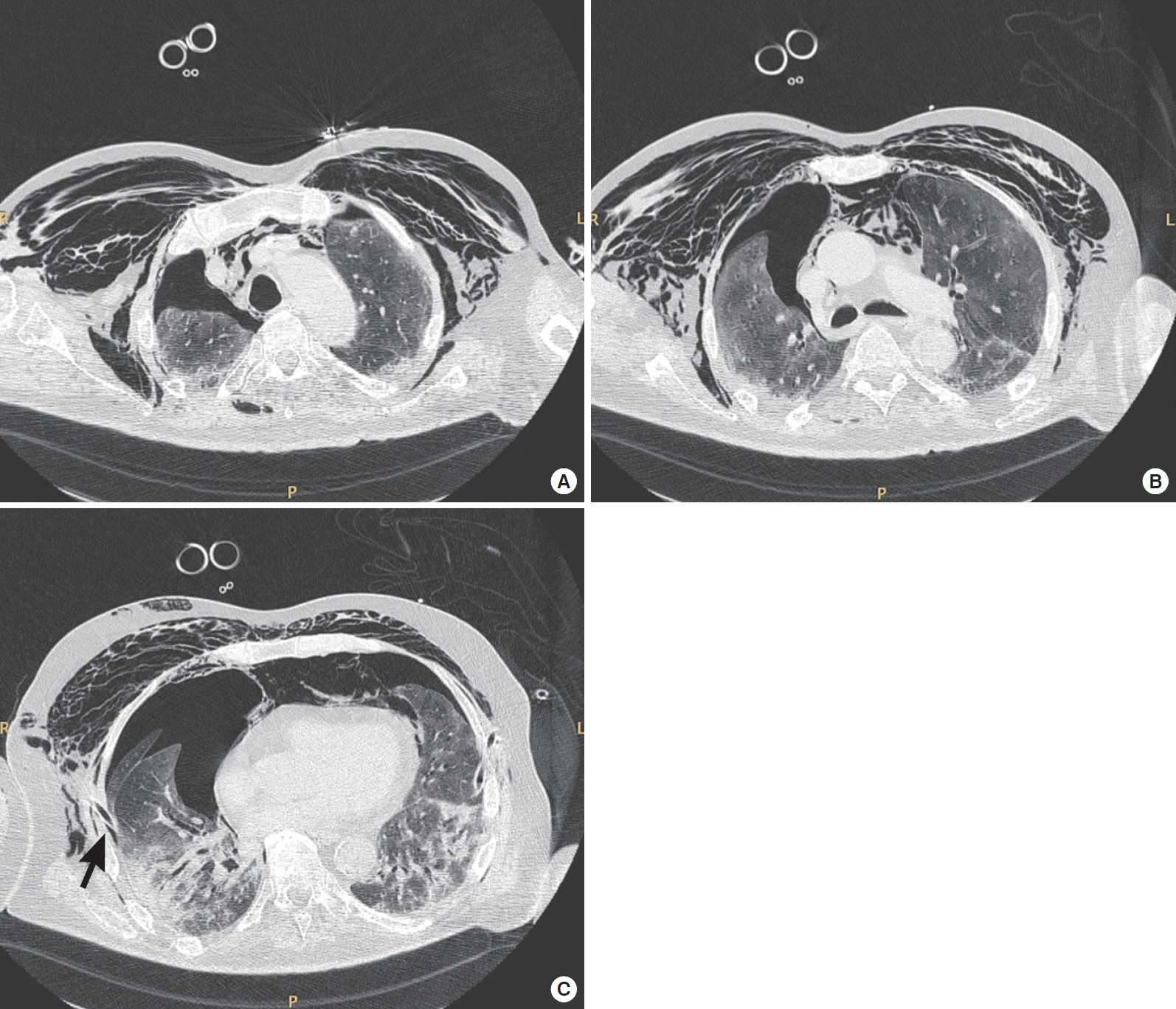
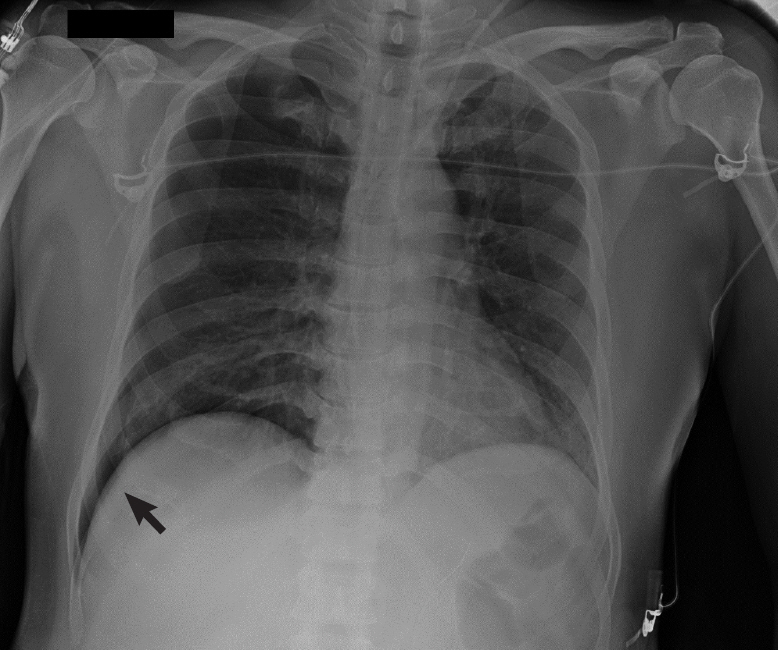
Pneumothorax and pulmonary air leaks as ventilator-induced injuries in COVID-19
- Affiliations
-
- 1Intensive Care Unit U.O.C. Anestesia e Rianimazione, Department of Surgery, University Hospital of Padua, Padua, Italy
- KMID: 2513258
- DOI: http://doi.org/10.4266/acc.2020.00955
Figure
Reference
-
1. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020; 395:507–13.
Article2. Benson JC, Carlson ML, Lane JI. MRI of the internal auditory canal, labyrinth, and middle ear: how we do it. Radiology. 2020; 297:252–65.
Article3. Bradley BT, Maioli H, Johnston R, Chaudhry I, Fink SL, Xu H, et al. Histopathology and ultrastructural findings of fatal COVID-19 infections in Washington State: a case series. Lancet. 2020; 396:320–32.
Article4. Mead J, Takishima T, Leith D. Stress distribution in lungs: a model of pulmonary elasticity. J Appl Physiol. 1970; 28:596–608.
Article5. Cruces P, Retamal J, Hurtado DE, Erranz B, Iturrieta P, González C, et al. A physiological approach to understand the role of respiratory effort in the progression of lung injury in SARS-CoV-2 infection. Crit Care. 2020; 24:494.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Obstruction of Ventilator Exhalational Valve due to High Moisture Content in compressed Air - A case report
- Pneumomediastinum, Pneumoperitoneum and Subcutaneous Emphysema without Pneumothorax during Endotrocheal Ventilator Anesthesis
- Treatment of Prolonged Air-leak after Bilobectomy by Artificial Pneumoperitoneum
- Effect of High Frequency Ventilation on Tension Pneumothorax Induced by Conventional Ventilator
- COVID-19 Vaccination for Pilots and Air Traffic Controllers