Acute Crit Care.
2021 Feb;36(1):70-74. 10.4266/acc.2020.00234.
A successfully treated case of primary purulent pericarditis complicated by cardiac tamponade and pneumopericardium
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Jeju National University Hospital, Jeju National University School of Medicine, Jeju, Korea
- 2Department of Internal Medicine, Jeju National University Hospital, Jeju National University School of Medicine, Jeju, Korea
- 3Department of Thoracic and Cardiovascular Surgery, Jeju National University Hospital, Jeju National University School of Medicine, Jeju, Korea
- KMID: 2513257
- DOI: http://doi.org/10.4266/acc.2020.00234
Abstract
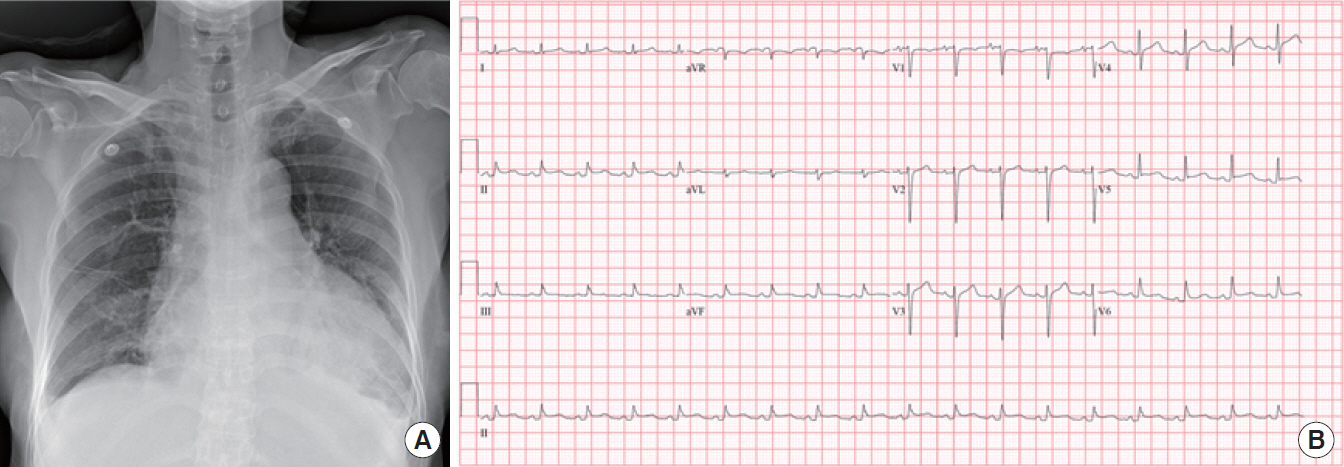
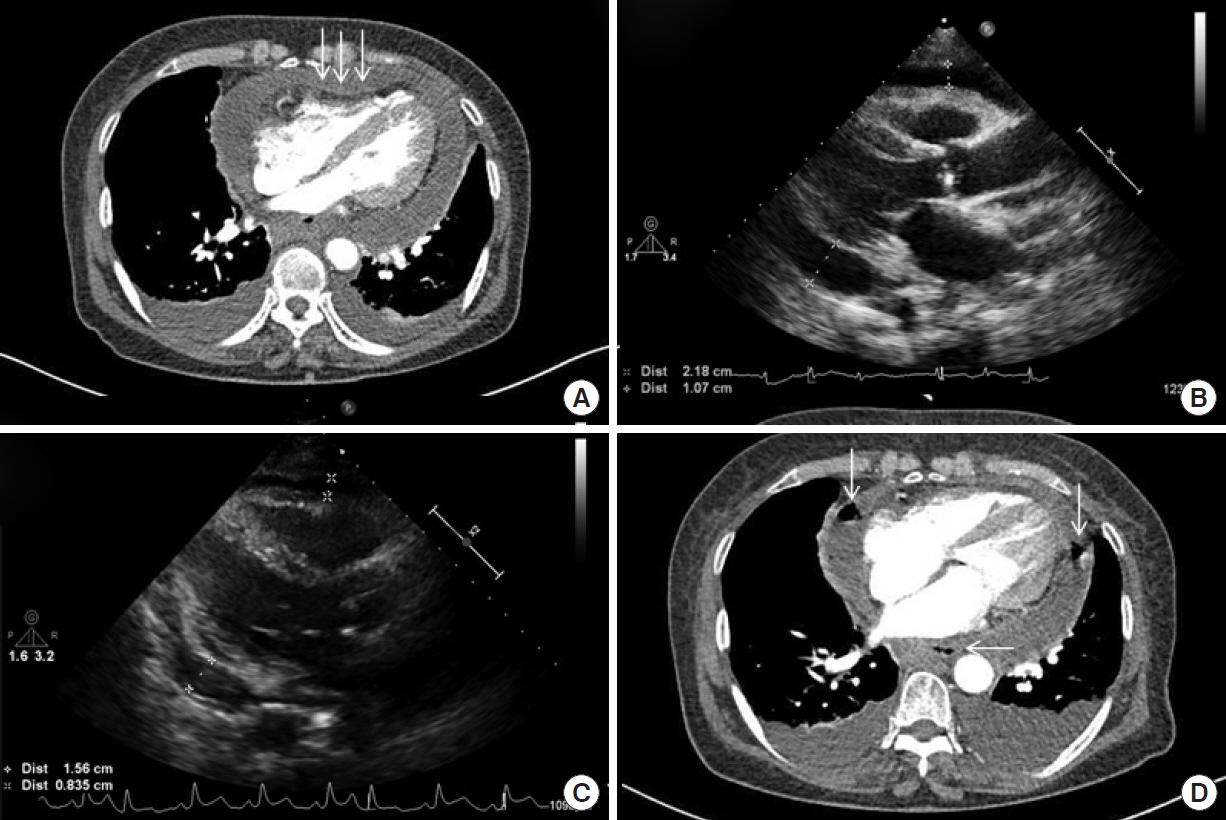
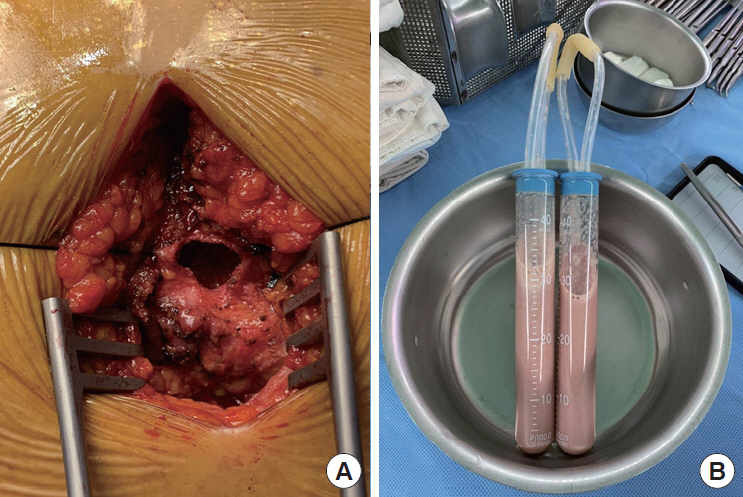
- Acute pericarditis is caused by various factors, but purulent pericarditis is rare. Primary purulent pericarditis in immunocompetent hosts is very rare in the modern antibiotics era. We report a successfully treated case of primary purulent pericarditis complicated with cardiac tamponade and pneumopericardium in an immunocompetent host. A 69-year-old female was referred from another hospital because of pleuritic chest pain with a large amount of pericardial effusion. She was diagnosed with acute pericarditis accompanied by cardiac tamponade. We performed emergency pericardiocentesis, with drainage of 360 ml of bloody pericardial fluid. The culture grew Streptococcus anginosus, confirming the diagnosis of acute purulent pericarditis. We performed pericardiostomy because cardiomegaly and pneumopericardium were aggravated after removal of the pericardial drainage catheter. The patient received antibiotics for a total of 23 days intravenously and was discharged with oral antibiotic therapy. Purulent pericarditis is one of the rare forms of pericarditis and is lifethreatening. A multimodality approach is required for proper diagnosis and treatment of this disease.
Keyword
Figure
Reference
-
1. Augustin P, Desmard M, Mordant P, Lasocki S, Maury JM, Heming N, et al. Clinical review: intrapericardial fibrinolysis in management of purulent pericarditis. Crit Care. 2011; 15:220.
Article2. Klacsmann PG, Bulkley BH, Hutchins GM. The changed spectrum of purulent pericarditis: an 86 year autopsy experience in 200 patients. Am J Med. 1977; 63:666–73.3. Hall IP. Purulent pericarditis. Postgrad Med J. 1989; 65:444–8.
Article4. Drummond MB, Dasenbrook EC, Pitz MW, Murphy DJ, Fan E. Inhaled corticosteroids in patients with stable chronic obstructive pulmonary disease: a systematic review and meta-analysis. JAMA. 2008; 300:2407–16.5. Parikh SV, Memon N, Echols M, Shah J, McGuire DK, Keeley EC. Purulent pericarditis: report of 2 cases and review of the literature. Medicine (Baltimore). 2009; 88:52–65.6. Skiest DJ, Steiner D, Werner M, Garner JG. Anaerobic pericarditis: case report and review. Clin Infect Dis. 1994; 19:435–40.
Article7. Go C, Asnis DS, Saltzman H. Pneumococcal pericarditis since 1980. Clin Infect Dis. 1998; 27:1338–40.
Article8. Kauffman CA, Watanakunakorn C, Phair JP. Purulent pneumococcal pericarditis: a continuing problem in the antibiotic era. Am J Med. 1973; 54:743–50.9. Ruoff KL. Streptococcus anginosus (“Streptococcus milleri”): the unrecognized pathogen. Clin Microbiol Rev. 1988; 1:102–8.
Article10. Hocken DB, Dussek JE. Streptococcus milleri as a cause of pleural empyema. Thorax. 1985; 40:626–8.
Article11. Ott CL, Hodge S. Gas-forming purulent pericardial effusion. Can J Cardiol. 2009; 25:e337.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cardiac Tamponade by Iatrogenic Pneumopericardium
- Primary Purulent Pericarditis with Cardiac Tamponade due to Oropharyngeal Polymicrobial Infection: A Case Report and Literature Review
- A Case of Cardiac Tamponade in a Patient with Rheumatoid Arthritis
- A Case of Acute Purulent Pericarditis Complicated by Severe Left Ventricular Systolic Dysfunction and Cardiac Tamponade
- A Case of Pericardial Tamponade in a Korean Man with Pericardial Abscess due to Bacteroides fragilis