Ann Surg Treat Res.
2021 Mar;100(3):175-185. 10.4174/astr.2021.100.3.175.
Factors associated with long-term graft patency after lower extremity arterial bypasses
- Affiliations
-
- 1Division of Vascular Surgery, Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Surgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2513198
- DOI: http://doi.org/10.4174/astr.2021.100.3.175
Abstract
- Purpose
This study was conducted to determine factors associated with long-term graft patency after lower extremity arterial bypass (LEAB).
Methods
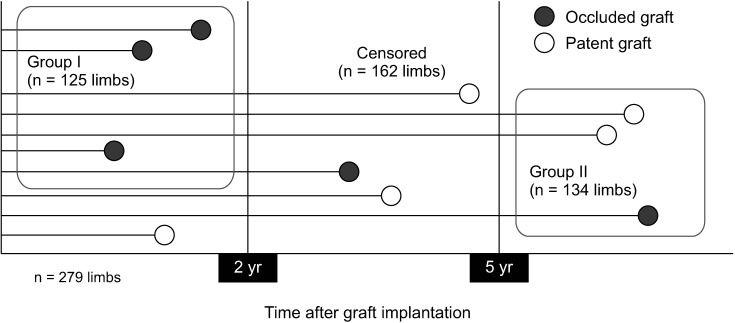
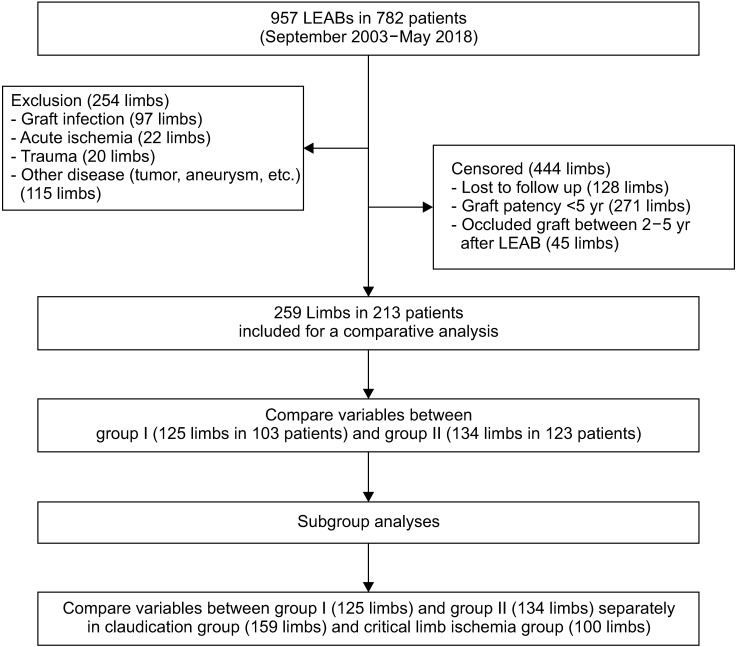
Database of LEABs for patients with chronic arterial occlusive disease (CAOD) at a single institution was retrospectively reviewed. To determine the factors we compared demographic, clinical, and procedural variables between 2 patient groups; group I (graft patency < 2 years) and group II (graft patency ≥ 5 years after LEAB) using univariable and multivariable analyses.
Results
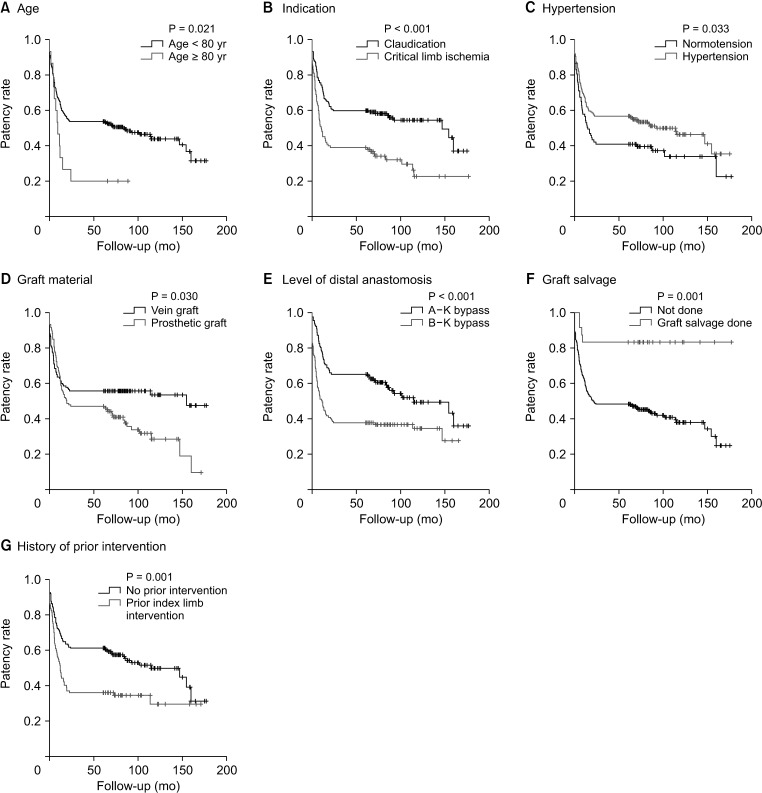
Among 957 LEABs, 259 limbs (group I, 125 limbs and group II, 134 limbs) in 213 patients were included for the analysis. On a univariable analysis, younger age (69 years vs. 66 years, P = 0.024), hypertension (60.8% vs. 74.6%, P = 0.017), claudication (51.2% vs. 70.9%, P = 0.001), absence of prior intervention (50.4% vs. 73.9%, P < 0.001), common femoral artery based bypass (57.6% vs. 70.1%, P = 0.035), above-the knee bypass (36.8% vs. 64.2%, P < 0.001), postoperative graft salvage procedure (3.2% vs. 14.8%, P = 0.001), and statin use (75.2% vs. 88.8, P = 0.004) were associated with long-term patency. On a multivariate analysis hypertension (odds ratio [OR], 1.91; P = 0.038), claudication (OR, 2.08; P = 0.032), no prior intervention (OR, 2.48; P = 0.001), vein graft (OR, 4.36; P = 0.001), above-the knee bypass (OR, 4.68; P < 0.001), and graft salvage procedures (OR, 7.70; P < 0.001) were identified as independent factors.
Conclusion
These factors can be considered in decision making before treatment of patients with CAOD.
Figure
Reference
-
1. Sachs T, Pomposelli F, Hamdan A, Wyers M, Schermerhorn M. Trends in the national outcomes and costs for claudication and limb threatening ischemia: angioplasty vs bypass graft. J Vasc Surg. 2011; 54:1021–1031. PMID: 21880457.
Article2. Antoniou GA, Chalmers N, Georgiadis GS, Lazarides MK, Antoniou SA, Serracino-Inglott F, et al. A meta-analysis of endovascular versus surgical reconstruction of femoropopliteal arterial disease. J Vasc Surg. 2013; 57:242–253. PMID: 23159476.
Article3. Antoniou GA, Georgiadis GS, Antoniou SA, Makar RR, Smout JD, Torella F. Bypass surgery for chronic lower limb ischaemia. Cochrane Database Syst Rev. 2017; 4:CD002000. PMID: 28368090.
Article4. Uhl C, Hock C, Betz T, Töpel I, Steinbauer M. Pedal bypass surgery after crural endovascular intervention. J Vasc Surg. 2014; 59:1583–1587. PMID: 24418639.
Article5. Hossain S, Leblanc D, Farber A, Power AH, DeRose G, Duncan A, et al. Editor's choice: infrainguinal bypass following failed endovascular intervention compared with primary bypass: a systematic review and meta-analysis. Eur J Vasc Endovasc Surg. 2019; 57:382–391. PMID: 30393063.6. Menard MT, Farber A, Assmann SF, Choudhry NK, Conte MS, Creager MA, et al. Design and rationale of the Best Endovascular Versus Best Surgical Therapy for Patients With Critical Limb Ischemia (BEST-CLI) Trial. J Am Heart Assoc. 2016; 5:e003219. PMID: 27402237.
Article7. Popplewell MA, Davies H, Jarrett H, Bate G, Grant M, Patel S, et al. Bypass versus angio plasty in severe ischaemia of the leg - 2 (BASIL-2) trial: study protocol for a randomised controlled trial. Trials. 2016; 17:11. PMID: 26739146.
Article8. Santo VJ, Dargon P, Azarbal AF, Liem TK, Mitchell EL, Landry GJ, et al. Lower extremity autologous vein bypass for critical limb ischemia is not adversely affected by prior endovascular procedure. J Vasc Surg. 2014; 60:129–135. PMID: 24613692.
Article9. Nguyen KP, Moneta G, Landry G. Venous conduits have superior patency compared with prosthetic grafts for femorofemoral bypass. Ann Vasc Surg. 2018; 52:126–137. PMID: 29783030.
Article10. Almasri J, Adusumalli J, Asi N, Lakis S, Alsawas M, Prokop LJ, et al. A systematic review and meta-analysis of revascularization outcomes of infrainguinal chronic limb-threatening ischemia. J Vasc Surg. 2018; 68:624–633. PMID: 29804736.
Article11. Heo SH, Park YJ, Woo SY, Kim DI, Kim YW. Comparison of long-term results of above-the-knee femoro-popliteal bypass with autogenous vein and polytetrafluoroethylene grafts. Ann Surg Treat Res. 2015; 88:28–34. PMID: 25553322.
Article12. Mills JL Sr, Conte MS, Armstrong DG, Pomposelli FB, Schanzer A, Sidawy AN, et al. The Society for Vascular Surgery Lower Extremity Threatened Limb Classification System: risk stratification based on wound, ischemia, and foot infection (WIfI). J Vasc Surg. 2014; 59:220–234. PMID: 24126108.
Article13. Gerhard-Herman MD, Gornik HL, Barrett C, Barshes NR, Corriere MA, Drachman DE, et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017; 135:e726–e779. PMID: 27840333.
Article14. Egorova NN, Guillerme S, Gelijns A, Morrissey N, Dayal R, McKinsey JF, et al. An analysis of the outcomes of a decade of experience with lower extremity revascularization including limb salvage, lengths of stay, and safety. J Vasc Surg. 2010; 51:878–885. PMID: 20045618.
Article15. Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, et al. ACC/AHA 2005 practice guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation. 2006; 113:e463–e654. PMID: 16549646.
Article16. Conte MS, Bradbury AW, Kolh P, White JV, Dick F, Fitridge R, et al. Global vascular guidelines on the management of chronic limb-threatening ischemia. Eur J Vasc Endovasc Surg. 2019; 58(1S):S1–S109. PMID: 31182334.17. Dosluoglu HH, Lall P, Harris LM, Dryjski ML. Long-term limb salvage and survival after endovascular and open revascularization for critical limb ischemia after adoption of endovascular-first approach by vascular surgeons. J Vasc Surg. 2012; 56:361–371. PMID: 22560307.
Article18. Whyman MR, Fowkes FG, Kerracher EM, Gillespie IN, Lee AJ, Housley E, et al. Randomised controlled trial of percutaneous transluminal angioplasty for intermittent claudication. Eur J Vasc Endovasc Surg. 1996; 12:167–172. PMID: 8760978.
Article19. Greenhalgh RM, Belch JJ, Brown LC, Gaines PA, Gao L, Reise JA, et al. The adjuvant benefit of angioplasty in patients with mild to moderate intermittent claudication (MIMIC) managed by supervised exercise, smoking cessation advice and best medical therapy: results from two randomised trials for stenotic femoropopliteal and aortoiliac arterial disease. Eur J Vasc Endovasc Surg. 2008; 36:680–688. PMID: 19022184.20. Nordanstig J, Taft C, Hensäter M, Perlander A, Osterberg K, Jivegård L. Improved quality of life after 1 year with an invasive versus a noninvasive treatment strategy in claudicants: one-year results of the Invasive Revascularization or Not in Intermittent Claudication (IRONIC) Trial. Circulation. 2014; 130:939–947. PMID: 25095886.21. Feinglass J, McCarthy WJ, Slavensky R, Manheim LM, Martin GJ. Functional status and walking ability after lower extremity bypass grafting or angioplasty for intermittent claudication: results from a prospective outcomes study. J Vasc Surg. 2000; 31(1 Pt 1):93–103. PMID: 10642712.
Article22. Malgor RD, Alahdab F, Elraiyah TA, Rizvi AZ, Lane MA, Prokop LJ, et al. A systematic review of treatment of intermittent claudication in the lower extremities. J Vasc Surg. 2015; 61(3 Suppl):54S–73S. PMID: 25721067.
Article23. Jones WS, Dolor RJ, Hasselblad V, Vemulapalli S, Subherwal S, Schmit K, et al. Comparative effectiveness of endovascular and surgical revascularization for patients with peripheral artery disease and critical limb ischemia: systematic review of revascularization in critical limb ischemia. Am Heart J. 2014; 167:489–498. PMID: 24655697.24. Siablis D, Kitrou PM, Spiliopoulos S, Katsanos K, Karnabatidis D. Paclitaxel-coated balloon angioplasty versus drug-eluting stenting for the treatment of infrapopliteal long-segment arterial occlusive disease: the IDEAS randomized controlled trial. JACC Cardiovasc Interv. 2014; 7:1048–1056. PMID: 25234679.25. Abu Dabrh AM, Steffen MW, Asi N, Undavalli C, Wang Z, Elamin MB, et al. Bypass surgery versus endovascular interventions in severe or critical limb ischemia. J Vasc Surg. 2016; 63:244–253. PMID: 26372187.
Article26. Bradbury AW, Adam DJ, Bell J, Forbes JF, Fowkes FG, Gillespie I, et al. Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) trial: a survival prediction model to facilitate clinical decision making. J Vasc Surg. 2010; 51(5 Suppl):52S–68S. PMID: 20435262.
Article27. Adam DJ, Beard JD, Cleveland T, Bell J, Bradbury AW, Forbes JF, et al. Bypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomised controlled trial. Lancet. 2005; 366:1925–1934. PMID: 16325694.
Article28. van der Zaag ES, Legemate DA, Prins MH, Reekers JA, Jacobs MJ. Angioplasty or bypass for superficial femoral artery disease?: a randomised controlled trial. Eur J Vasc Endovasc Surg. 2004; 28:132–137. PMID: 15234692.
Article29. Kim YW, Lee JH, Kim HG, Huh S. Factors affecting the long-term patency of crossover femorofemoral bypass graft. Eur J Vasc Endovasc Surg. 2005; 30:376–380. PMID: 15890541.
Article30. Meecham L, Patel S, Bate GR, Bradbury AW. Editor's choice: a comparison of clinical outcomes between primary bypass and secondary bypass after failed plain balloon angioplasty in the Bypass versus Angioplasty for Severe Ischaemia of the Limb (BASIL) Trial. Eur J Vasc Endovasc Surg. 2018; 55:666–671. PMID: 29599067.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Graft Patency Rates between the Diabetic and Non-diabetic Patients after Infrainguinal Arterial Bypasses
- Impact of Diabetes Mellitus on Early Graft Patency of Peripheral Arterial Occlusive Disease
- Outcomes of Infrainguinal Arterial Bypasses for the Patients with Atherosclerotic Lower Extremity Arterial Occlusive Disease
- Comparisons between prosthetic vascular graft and saphenous vein graft in femoro-popliteal bypass
- Comparison of Long-Term Results of Leg Arterial Bypasses between the Patients with Chronic Critical Limb Ischemia and Claudication