Ann Surg Treat Res.
2021 Mar;100(3):137-143. 10.4174/astr.2021.100.3.137.
Post-resection prognosis of patients with hepatic epithelioid hemangioendothelioma
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2513194
- DOI: http://doi.org/10.4174/astr.2021.100.3.137
Abstract
- Purpose
Epithelioid hemangioendothelioma (EHE) is a rare borderline vascular tumor. This retrospective, single-center study evaluated the outcomes of hepatic resection (HR) in patients with hepatic EHE.
Methods
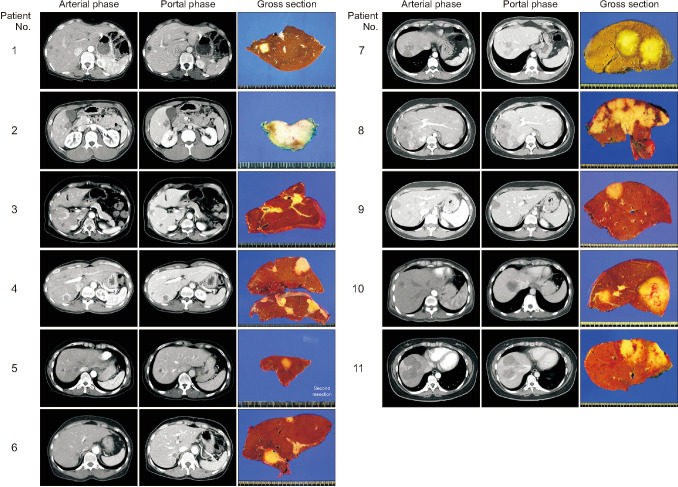
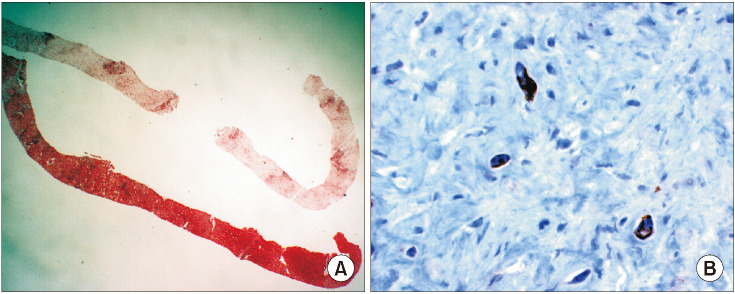
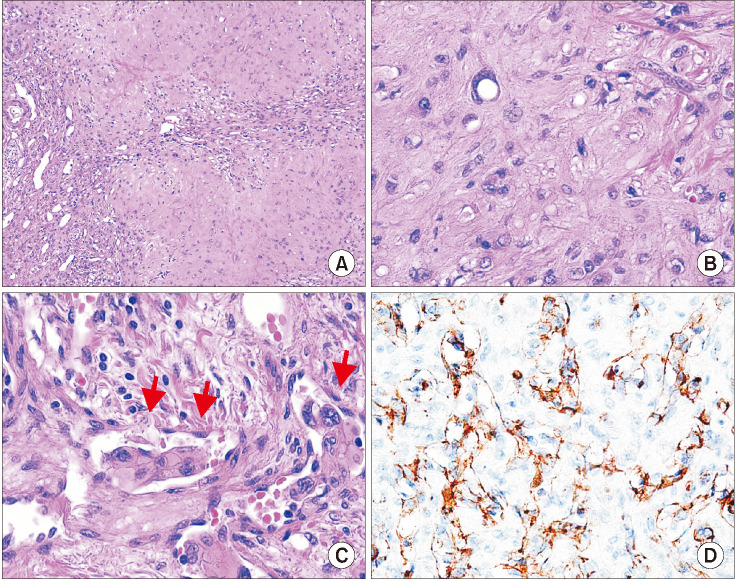
Over the 10-year period from 2009 to 2018, 11 patients with hepatic EHE underwent HR, accounting for 0.1% of the 11,979 adults who underwent HR at our center. Diagnosis of hepatic EHE was confirmed by immunohistochemical staining for CD34, CD31, and factor VIII-related antigen.
Results
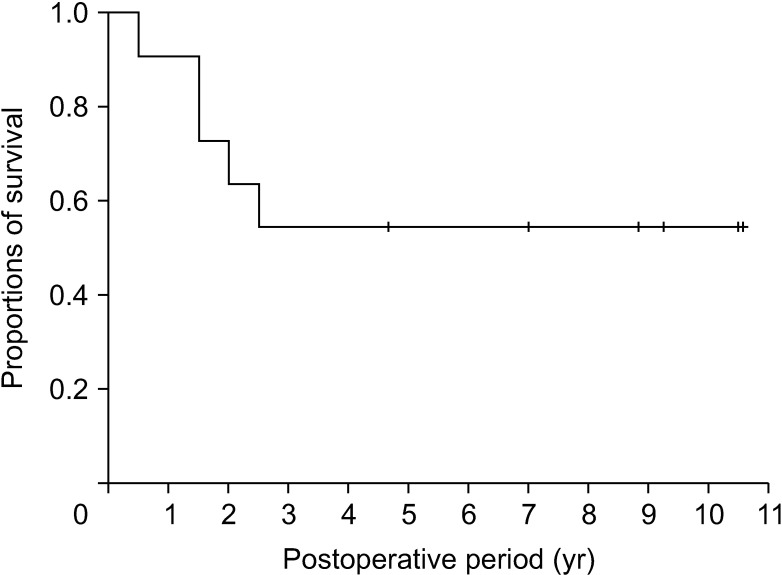
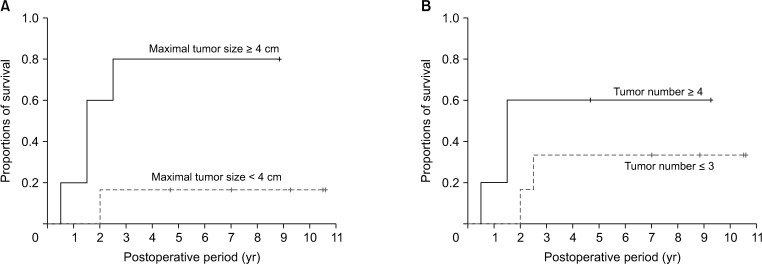
The 11 patients included 9 females (81.8%) and 2 males (18.2%) with mean age of 43.5 ± 13.6 years. Preoperative imaging resulted in a preliminary diagnosis of suspected liver metastasis or EHE, with 9 patients (81.8%) undergoing liver biopsy. No patient presented with abnormally elevated concentrations of liver tumor markers. The extents of HR were determined by tumor size and location from trisectionectomy to partial hepatectomy. All patients recovered uneventfully from HR. Five patients showed tumor recurrence, with 4 receiving locoregional treatments for recurrent lesions. The 1-, 3-and 5-year disease-free survival rates were 90.9%, 54.5%, and 54.5%, respectively. Currently, all patients remain alive and are doing well. Univariate analysis on tumor recurrence showed that tumor size ≥ 4 cm was significantly associated with tumor recurrence (P = 0.032), but tumor number ≥ 4 was not related to (P = 0.24).
Conclusion
Hepatic EHE is a rare form of primary liver tumor often misdiagnosed as a metastatic tumor. Because of its malignant potential, HR is indicated if possible. HR plus, when necessary, treatment of recurrence yields favorable overall survival rates in patients with hepatic EHE.
Figure
Cited by 1 articles
-
Living donor liver transplantation in an infant patient with progressive familial intrahepatic cholestasis along with hepatocellular carcinoma: a case report
Jung-Man Namgoong, Shin Hwang, Dae-Yeon Kim, Chul-Soo Ahn, Hyunhee Kwon, Suhyeon Ha, Kyung Mo Kim, Seak Hee Oh
Korean J Transplant. 2022;36(1):73-78. doi: 10.4285/kjt.21.0007.
Reference
-
1. Sardaro A, Bardoscia L, Petruzzelli MF, Portaluri M. Epithelioid hemangioendothelioma: an overview and update on a rare vascular tumor. Oncol Rev. 2014; 8:259. PMID: 25992243.
Article2. Mertens F, Unni KK, Fletcher CD. World Health Organization classification of tumors: Pathology and genetics of tumors of soft tissue and bone. Lyon: IRAC Press;2002. p. 155.3. Lau K, Massad M, Pollak C, Rubin C, Yeh J, Wang J, et al. Clinical patterns and outcome in epithelioid hemangioendothelioma with or without pulmonary involvement: insights from an internet registry in the study of a rare cancer. Chest. 2011; 140:1312–1318. PMID: 21546438.4. Ishak KG, Sesterhenn IA, Goodman ZD, Rabin L, Stromeyer FW. Epithelioid hemangioendothelioma of the liver: a clinicopathologic and follow-up study of 32 cases. Hum Pathol. 1984; 15:839–852. PMID: 6088383.
Article5. Makhlouf HR, Ishak KG, Goodman ZD. Epithelioid hemangioendothelioma of the liver: a clinicopathologic study of 137 cases. Cancer. 1999; 85:562–582. PMID: 10091730.6. Mehrabi A, Kashfi A, Fonouni H, Schemmer P, Schmied BM, Hallscheidt P, et al. Primary malignant hepatic epithelioid hemangioendothelioma: a comprehensive review of the literature with emphasis on the surgical therapy. Cancer. 2006; 107:2108–2121. PMID: 17019735.7. Wang LR, Zhou JM, Zhao YM, He HW, Chai ZT, Wang M, et al. Clinical experience with primary hepatic epithelioid hemangioendothelioma: retrospective study of 33 patients. World J Surg. 2012; 36:2677–2683. PMID: 22890877.
Article8. Lin J, Ji Y. CT and MRI diagnosis of hepatic epithelioid hemangioendothelioma. Hepatobiliary Pancreat Dis Int. 2010; 9:154–158. PMID: 20382586.9. Ben-Haim M, Roayaie S, Ye MQ, Thung SN, Emre S, Fishbein TA, et al. Hepatic epithelioid hemangioendothelioma: resection or transplantation, which and when? Liver Transpl Surg. 1999; 5:526–531. PMID: 10545542.
Article10. Imanishi H, Kawata M, Yanagihara M, Nakayama N, Sato T, Furukawa Y, et al. Epithelioid hemangioendothelioma of the liver associated with thrombocytopenia and coagulopathy. Hepatogastroenterology. 2002; 49:1673–1675. PMID: 12397762.11. Jung DH, Hwang S, Hong SM, Kim KH, Lee YJ, Ahn CS, et al. Clinicopathological features and prognosis of hepatic epithelioid hemangioendothelioma after liver resection and transplantation. Ann Transplant. 2016; 21:784–790. PMID: 28031549.
Article12. Jeong SW, Woo HY, You CR, Huh WH, Bae SH, Choi JY, et al. A case of hepatic epithelioid hemangioendothelioma that caused extrahepatic metastases without intrahepatic recurrence after hepatic resection. Korean J Hepatol. 2008; 14:525–531. PMID: 19119248.
Article13. Cho HD, Hwang S, Lee YJ, Park KM, Kim KH, Kim JC, et al. Changes in the types of liver diseases requiring hepatic resection: a single-institution experience of 9016 cases over a 10-year period. Korean J Hepatobiliary Pancreat Surg. 2016; 20:49–52. PMID: 27212990.
Article14. Hwang S, Ha TY, Song GW, Jung DH, Ahn CS, Moon DB, et al. Quantified risk assessment for major hepatectomy via the indocyanine green clearance rate and liver volumetry combined with standard liver volume. J Gastrointest Surg. 2015; 19:1305–1314. PMID: 25947549.
Article15. Hwang S, Lee YJ, Kim KH, Ahn CS, Moon DB, Ha TY, et al. The impact of tumor size on long-term survival outcomes after resection of solitary hepatocellular carcinoma: single-institution experience with 2,558 patients. J Gastrointest Surg. 2015; 19:1281–1290. PMID: 25956724.
Article16. Hwang S, Lee YJ, Song GW, Park KM, Kim KH, Ahn CS, et al. Prognostic impact of tumor growth type on 7th AJCC staging system for intrahepatic cholangiocarcinoma: a single-center experience of 659 cases. J Gastrointest Surg. 2015; 19:1291–1304. PMID: 25820487.
Article17. Yoon YI, Hwang S, Lee YJ, Kim KH, Ahn CS, Moon DB, et al. Postresection outcomes of combined hepatocellular carcinoma-cholangiocarcinoma, hepatocellular carcinoma and intrahepatic cholangiocarcinoma. J Gastrointest Surg. 2016; 20:411–420. PMID: 26628072.
Article18. Miettinen M, Fletcher CD, Kindblom LG, Zimmermann A, Tsui WM. Mesenchymal tumours of the liver. In : Bosman FT, Carneiro F, Hruban RH, Theise ND, editors. WHO Classification of tumours of the digestive system. Lyon: IARC Press;2010. p. 241–250.19. Grotz TE, Nagorney D, Donohue J, Que F, Kendrick M, Farnell M, et al. Hepatic epithelioid haemangioendothelioma: is transplantation the only treatment option? HPB (Oxford). 2010; 12:546–553. PMID: 20887322.
Article20. Cao L, Hong J, Zhou L, Ye Y, Liu Y, Yu J, et al. Selection of treatment for hepatic epithelioid hemangioendothelioma: a single-center experience. World J Surg Oncol. 2019; 17:183. PMID: 31699108.
Article21. Simpson ND, Ahmed AM, Simpson PW, Parkar JA, Keeffe EB, Ahmed A. Living donor liver transplantation in a patient with hepatic epithelioid hemangioendothelioma. J Clin Gastroenterol. 2003; 37:349–350. PMID: 14506396.
Article22. Galvão FH, Bakonyi-Neto A, Machado MA, Farias AQ, Mello ES, Diz ME, et al. Interferon alpha-2B and liver resection to treat multifocal hepatic epithelioid hemangioendothelioma: a relevant approach to avoid liver transplantation. Transplant Proc. 2005; 37:4354–4358. PMID: 16387119.
Article23. Cardinal J, de Vera ME, Marsh JW, Steel JL, Geller DA, Fontes P, et al. Treatment of hepatic epithelioid hemangioendothelioma: a single-institution experience with 25 cases. Arch Surg. 2009; 144:1035–1039. PMID: 19917940.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of hepatic epithelioid hemangioendothelioma that caused extrahepatic metastases without intrahepatic recurrence after hepatic resection
- A Case of Hepatic Epithelioid Hemangioendothelioma Treated with Radiofrequency Ablation
- Epithelioid Hemangioendothelioma of the Liver: A Case Report
- A Case of Epithelioid Hemangioendothelioma on the Choana
- Epithelioid hemangioendothelioma of the liver