Ann Hepatobiliary Pancreat Surg.
2021 Feb;25(1):126-131. 10.14701/ahbps.2021.25.1.126.
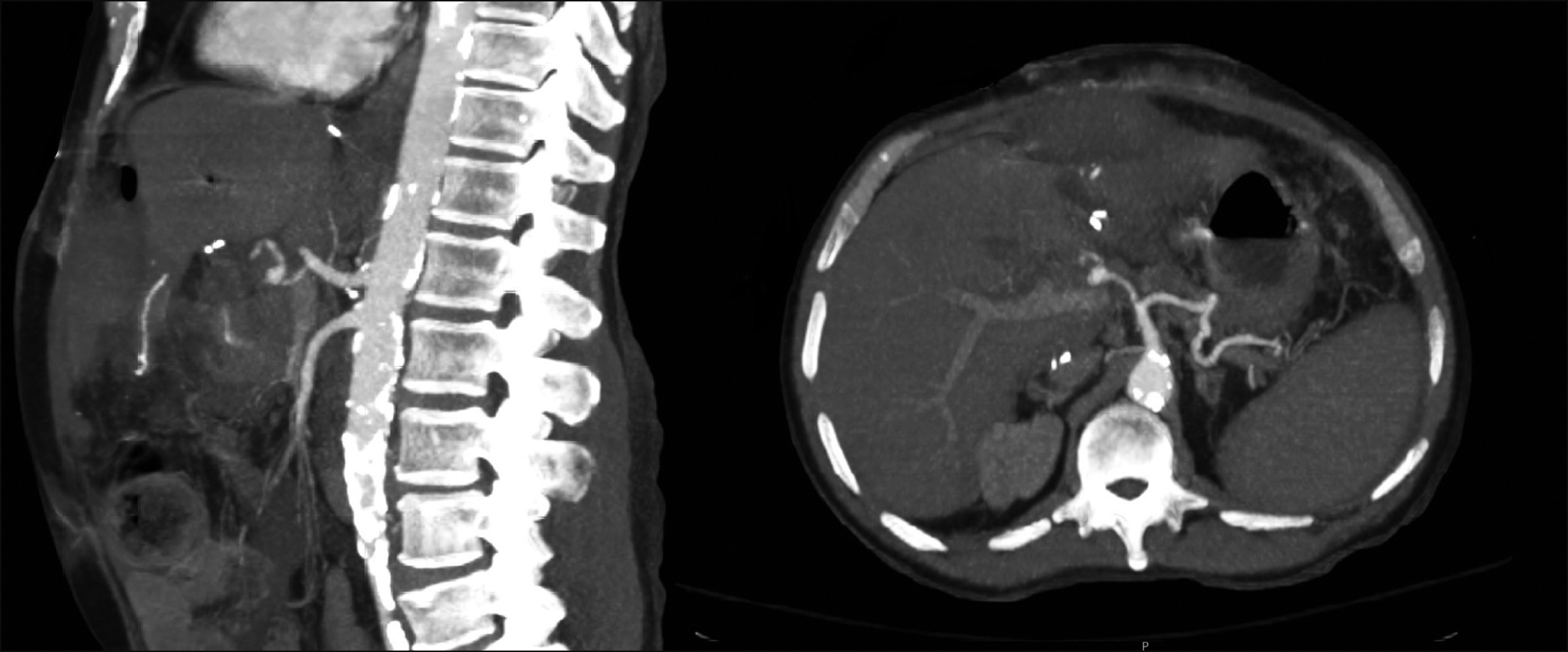
Application of resuscitative endovascular balloon occlusion in post-transplant mycotic hepatic artery pseudoaneurysm rupture in the setting of Aspergillus Constellatus bacteremia
- Affiliations
-
- 1Division of Solid Organ Transplantation, Department of Surgery, UAMS Medical Center, USA
- 2Division of Trauma and Critical Care Surgery, Department of Surgery, UAMS Medical Center, Little Rock, AR, USA
- KMID: 2513186
- DOI: http://doi.org/10.14701/ahbps.2021.25.1.126
Abstract
- Hepatic artery pseudoaneurysm (HAP) is a rare, highly morbid and frequently fatal complication of liver transplantation. Most are a mycotic mediated weakness of the arterial wall, with associated bacterial or fungal infection of ascitic fluid. As it is usually asymptomatic prior to rupture, the majority present in acute hemorrhagic shock and dire extremis. Resuscitative endovascular balloon occlusion (REBOA) was initially developed for the management of noncompressible hemorrhagic shock in trauma; however, remains underutilized and understudied in the non-trauma setting. We present the case of a mycotic hepatic artery pseudoaneurysm rupture due to Streptococcus constellatus and Klebsiella pneumoniae post directed donor orthoptic liver transplant, in which REBOA was employed in the setting of impending exsanguination as a bridge to definitive surgical intervention. Although this patient passed away of multiorgan system failure prior to re-transplant, this case demonstrates the importance of a heightened suspicion of this devastating complication, especially in the setting of bilioenteric reconstruction and perihepatic fluid collection, as well as the benefit of utilizing resuscitative techniques such as REBOA prior to definitive surgical or endovascular therapy to mitigate the high morbidity and mortality of this condition.
Keyword
Figure
Reference
-
1. Langnas AN, Marujo W, Stratta RJ, Wood RP, Shaw BW Jr. 1991; Vascular complications after orthotopic liver transplantation. Am J Surg. 161:76–82. discussion 82–83. DOI: 10.1016/0002-9610(91)90364-J. PMID: 1987861.
Article2. Leelaudomlipi S, Bramhall SR, Gunson BK, Candinas D, Buckels JA, McMaster P, et al. 2003; Hepatic-artery aneurysm in adult liver transplantation. Transpl Int. 16:257–261. DOI: 10.1111/j.1432-2277.2003.tb00296.x. PMID: 12730806.
Article3. Marshall MM, Muiesan P, Srinivasan P, Kane PA, Rela M, Heaton ND, et al. 2001; Hepatic artery pseudoaneurysms following liver transplantation: incidence, presenting features and management. Clin Radiol. 56:579–587. DOI: 10.1053/crad.2001.0650. PMID: 11446757.
Article4. Volpin E, Pessaux P, Sauvanet A, Sibert A, Kianmanesh R, Durand F, et al. 2014; Preservation of the arterial vascularisation after hepatic artery pseudoaneurysm following orthotopic liver transplantation: long-term results. Ann Transplant. 19:346–352. DOI: 10.12659/AOT.890473. PMID: 25034853.
Article5. Gupta BK, Khaneja SC, Flores L, Eastlick L, Longmore W, Shaftan GW. 1989; The role of intra-aortic balloon occlusion in penetrating abdominal trauma. J Trauma. 29:861–865. DOI: 10.1097/00005373-198906000-00026. PMID: 2661845.
Article6. Morrison JJ, Galgon RE, Jansen JO, Cannon JW, Rasmussen TE, Eliason JL. 2016; A systematic review of the use of resuscitative endovascular balloon occlusion of the aorta in the management of hemorrhagic shock. J Trauma Acute Care Surg. 80:324–334. DOI: 10.1097/TA.0000000000000913. PMID: 26816219.
Article7. Ribeiro Júnior MAF, Maurício AD, Costa CTK, Néder PR, Augusto SS, Di-Saverio S, et al. 2019; Expanding indications and results for the use of resuscitative endovascular balloon occlusion of the aorta - REBOA. Rev Col Bras Cir. 46:e20192334. DOI: 10.1590/0100-6991e-20192334. PMID: 31859727.8. Frongillo F, Lirosi MC, Nure E, Inchingolo R, Bianco G, Silvestrini N, et al. 2015; Diagnosis and management of hepatic artery complications after liver transplantation. Transplant Proc. 47:2150–2155. DOI: 10.1016/j.transproceed.2014.11.068. PMID: 26361665.
Article9. Thorat A, Lee CF, Wu TH, Pan KT, Chu SY, Chou HS, et al. 2017; Endovascular treatment for pseudoaneurysms arising from the hepatic artery after liver transplantation. Asian J Surg. 40:227–231. DOI: 10.1016/j.asjsur.2014.07.001. PMID: 25183291.
Article10. Morinaga Y, Yanagihara K, Gyotoku H, Oshima K, Izumikawa K, Yamasaki N, et al. 2013; Pulmonary artery pseudoaneurysm caused by Streptococcus constellatus. Int J Infect Dis. 17:e1064–e1066. DOI: 10.1016/j.ijid.2013.03.013. PMID: 24128874.
Article11. Raja NS, Nikolova A, Raudsepp T, Weston-Smith SG, Rumbold A, Shaikh H, et al. 2017; Streptococcus constellatus causing mycotic aneurysm in a patient with diffuse large B-cell lymphoma. J Microbiol Infect Dis. 7:213–216. DOI: 10.5799/jmid.369278.
Article12. Qian Y, Zhang H, Chen X, Zhang J, Xia Q. 2020; Graft hepatic artery rupture due to carbapenem-resistant Klebsiella pneumoniae infection after liver transplant. Exp Clin Transplant. 18:529–532. DOI: 10.6002/ect.2018.0384. PMID: 31424357.
Article13. Sadeghi M, Dogan EM, Karlsson C, Jansson K, Seilitz J, Skoog P, et al. 2020; Total resuscitative endovascular balloon occlusion of the aorta causes inflammatory activation and organ damage within 30 minutes of occlusion in normovolemic pigs. BMC Surg. 20:43. DOI: 10.1186/s12893-020-00700-3. PMID: 32122358. PMCID: PMC7053141.
Article14. Forte DM, Do WS, Weiss JB, Sheldon RR, Kuckelman JP, Eckert MJ, et al. 2019; Titrate to equilibrate and not exsanguinate! Characterization and validation of a novel partial resuscitative endovascular balloon occlusion of the aorta catheter in normal and hemorrhagic shock conditions. J Trauma Acute Care Surg. 87:1015–1025. DOI: 10.1097/TA.0000000000002378. PMID: 31135770.
Article15. Bonham CA, Kapur S, Geller D, Fung JJ, Pinna A. 1999; Excision and immediate revascularization for hepatic artery pseudoaneurysm following liver transplantation. Transplant Proc. 31:443. DOI: 10.1016/S0041-1345(98)01698-4. PMID: 10083180.
Article16. Boleslawski E, Bouras AF, Truant S, Liddo G, Herrero A, Badic B, et al. 2013; Hepatic artery ligation for arterial rupture following liver transplantation: a reasonable option. Am J Transplant. 13:1055–1062. DOI: 10.1111/ajt.12135. PMID: 23398886.
Article17. Tulsyan N, Kashyap VS, Greenberg RK, Sarac TP, Clair DG, Pierce G, et al. 2007; The endovascular management of visceral artery aneurysms and pseudoaneurysms. J Vasc Surg. 45:276–283. discussion 283DOI: 10.1016/j.jvs.2006.10.049. PMID: 17264002.
Article18. Patel JV, Weston MJ, Kessel DO, Prasad R, Toogood GJ, Robertson I. 2003; Hepatic artery pseudoaneurysm after liver transplantation: treatment with percutaneous thrombin injection. Transplantation. 75:1755–1757. DOI: 10.1097/01.TP.0000063936.94587.10. PMID: 12777870.
Article19. Pedersoli F, Isfort P, Keil S, Goerg F, Zimmermann M, Liebl M, et al. 2016; Stentgraft implantation for the treatment of postoperative hepatic artery pseudoaneurysm. Cardiovasc Intervent Radiol. 39:575–581. DOI: 10.1007/s00270-015-1274-1. PMID: 26797022.
Article20. Sachdev U, Baril DT, Ellozy SH, Lookstein RA, Silverberg D, Jacobs TS, et al. 2006; Management of aneurysms involving branches of the celiac and superior mesenteric arteries: a comparison of surgical and endovascular therapy. J Vasc Surg. 44:718–724. DOI: 10.1016/j.jvs.2006.06.027. PMID: 17011997.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Balloon Tamponade Treatment of a Stent-graft Related Rupture with a Splenic Artery Pseudoaneurysm: A Case Report
- Resuscitative Endovascular Balloon Occlusion of the Aorta for an Iliac Artery Aneurysm: Case Report
- A Case of Management of Carotid Artery Rupture by Detachable Balloon Embolization
- Technical Pitfalls in the Endovascular Treatment of Traumatic Pseudoaneurysm of the Internal Carotid Artery: Case Report
- Jejunal Migration of the Stent-Graft Used for Common Hepatic Artery Pseudoaneurysm