Diabetes Metab J.
2020 Dec;44(6):897-907. 10.4093/dmj.2020.0199.
Does Diabetes Increase the Risk of Contracting COVID-19? A Population-Based Study in Korea
- Affiliations
-
- 1Research and Analysis Team, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 2Research Institute of National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 3Department of Big Data, National Health Insurance Service, Wonju, Korea
- 4Medical Library, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 5Department of Otolaryngology-Head and Neck Surgery, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 6Department of Pathology, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 7Department of Physical Medicine and Rehabilitation, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 8Division of Endocrinology and Metabolism, Department of Internal Medicine, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- KMID: 2513053
- DOI: http://doi.org/10.4093/dmj.2020.0199
Abstract
- Background
This study aimed to determine the infection risk of coronavirus disease 2019 (COVID-19) in patients with diabetes (according to treatment method).
Methods
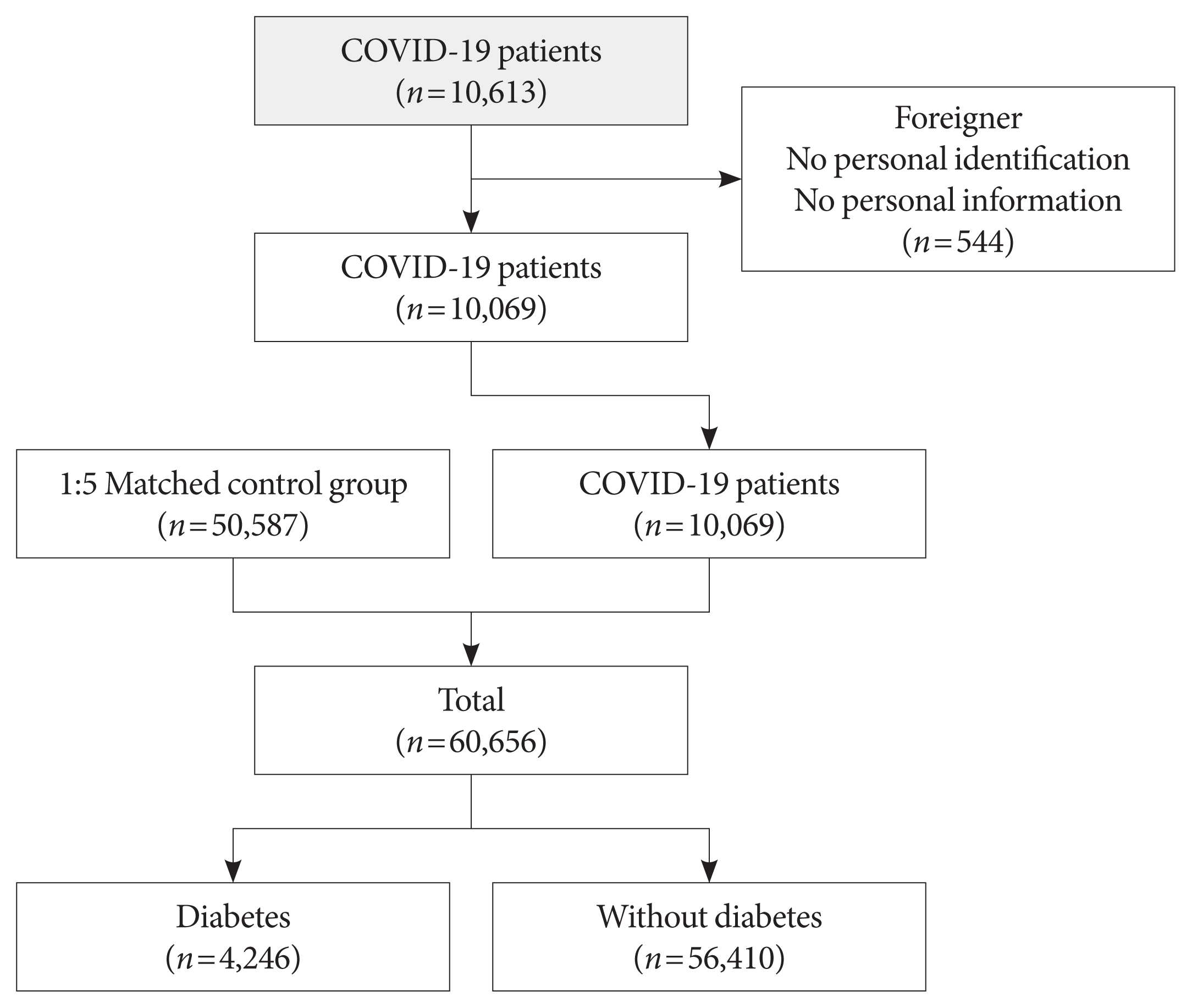
Claimed subjects to the Korean National Health Insurance claims database diagnosed with COVID-19 were included. Ten thousand sixty-nine patients with COVID-19 between January 28 and April 5, 2020, were included. Stratified random sampling of 1:5 was used to select the control group of COVID-19 patients. In total 50,587 subjects were selected as the control group. After deleting the missing values, 60,656 subjects were included.
Results
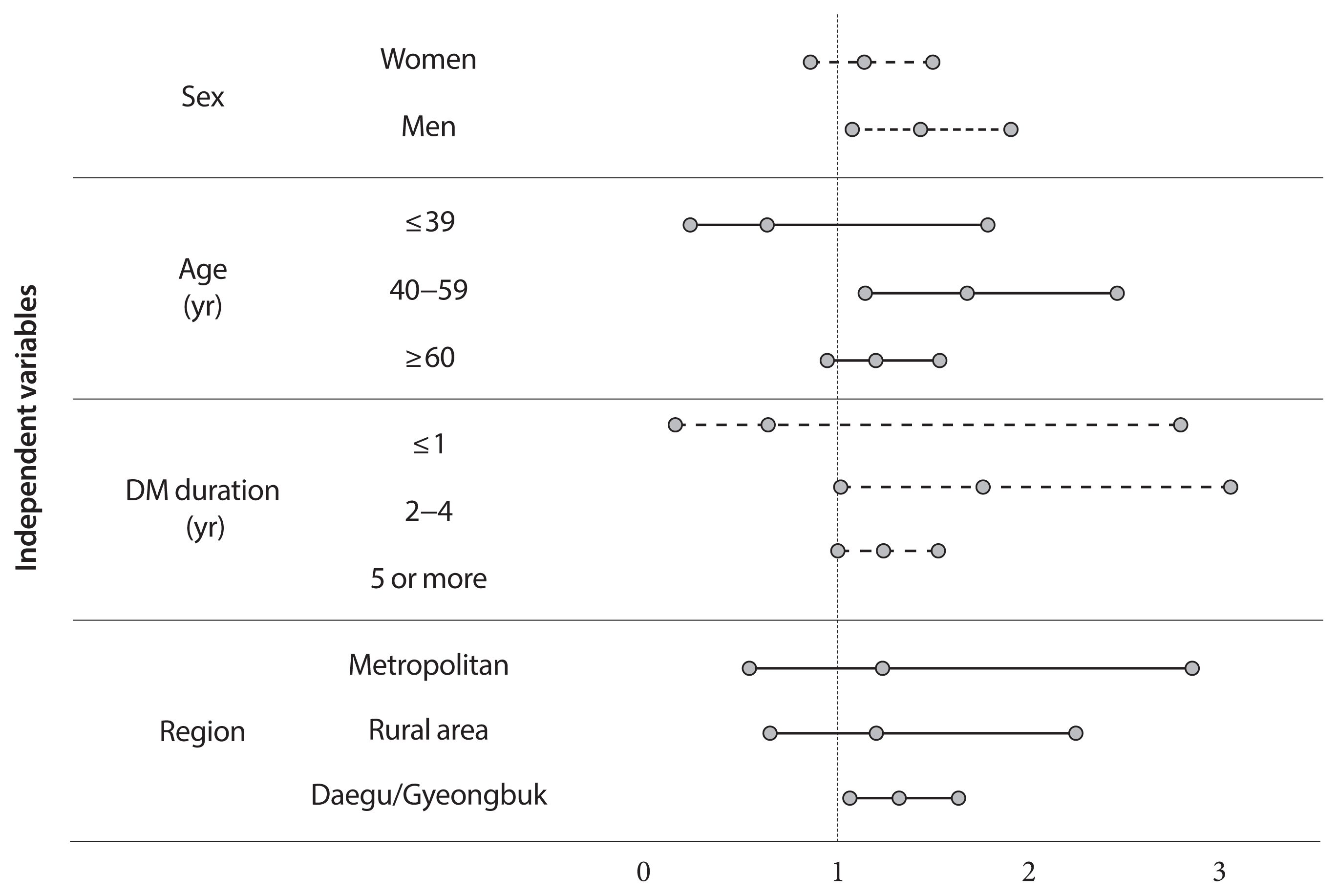
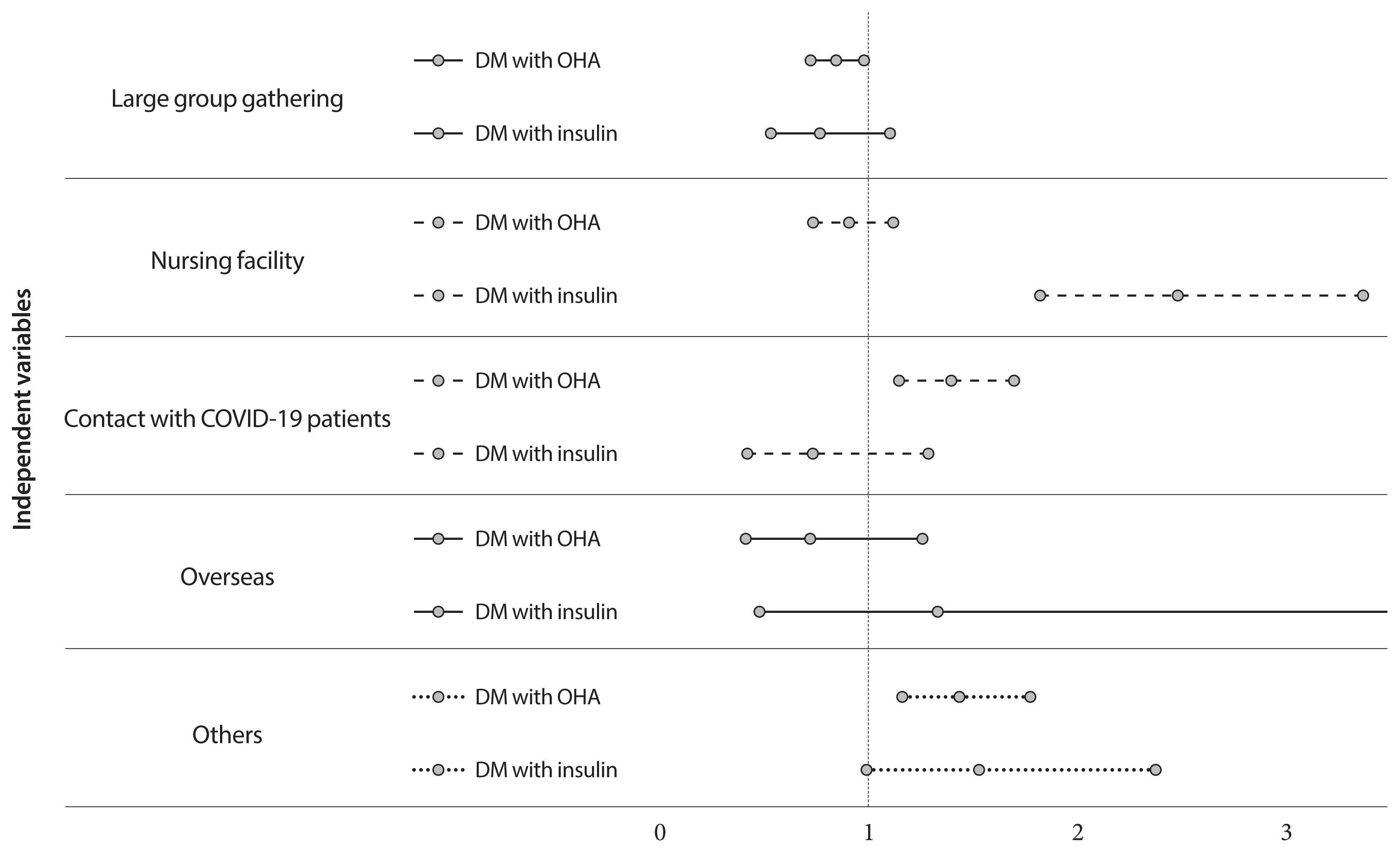
Adjusted odds ratio (OR) indicated that diabetic insulin users had a higher risk of COVID-19 than subjects without diabetes (OR, 1.25; 95% confidence interval [CI], 1.03 to 1.53; P=0.0278). In the subgroup analysis, infection risk was higher among diabetes male insulin users (OR, 1.42; 95% CI, 1.07 to 1.89), those between 40 and 59 years (OR, 1.66; 95% CI, 1.13 to 2.44). The infection risk was higher in diabetic insulin users with 2 to 4 years of morbidity (OR, 1.744; 95% CI, 1.003 to 3.044).
Conclusion
Some diabetic patients with certain conditions would be associated with a higher risk of acquiring COVID-19, highlighting their need for special attention. Efforts are warranted to ensure that diabetic patients have minimal exposure to the virus. It is important to establish proactive care and screening tests for diabetic patients suspected with COVID-19 for timely disease diagnosis and management.
Keyword
Figure
Cited by 1 articles
-
Impact of Diabetes on COVID-19 Susceptibility: A Nationwide Propensity Score Matching Study
Han Na Jang, Sun Joon Moon, Jin Hyung Jung, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee
Endocrinol Metab. 2024;39(5):813-818. doi: 10.3803/EnM.2024.2014.
Reference
-
1. World Health Organization. Novel coronavirus: China. 2020. Available from: https://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/(cited 2020 Dec 1).2. Badawi A, Ryoo SG. Prevalence of diabetes in the 2009 influenza A (H1N1) and the Middle East respiratory syndrome coronavirus: a systematic review and meta-analysis. J Public Health Res. 2016; 5:733.
Article3. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020; 323:1239–42.4. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020; 395:1054–62.
Article5. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, Colagiuri S, Guariguata L, Motala AA, Ogurtsova K, Shaw JE, Bright D, Williams R. IDF Diabetes Atlas Committee. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019; 157:107843.
Article6. Kim BY, Won JC, Lee JH, Kim HS, Park JH, Ha KH, Won KC, Kim DJ, Park KS. Diabetes fact sheets in Korea, 2018: an appraisal of current status. Diabetes Metab J. 2019; 43:487–94.
Article7. Song SO, Song YD, Nam JY, Park KH, Yoon JH, Son KM, Ko Y, Lim DH. Epidemiology of type 1 diabetes mellitus in Korea through an investigation of the national registration project of type 1 diabetes for the reimbursement of glucometer strips with additional analyses using claims data. Diabetes Metab J. 2016; 40:35–45.
Article8. Hu FB, Satija A, Manson JE. Curbing the diabetes pandemic: the need for global policy solutions. JAMA. 2015; 313:2319–20.9. Song SO, Jung CH, Song YD, Park CY, Kwon HS, Cha BS, Park JY, Lee KU, Ko KS, Lee BW. Background and data configuration process of a nationwide population-based study using the Korean national health insurance system. Diabetes Metab J. 2014; 38:395–403.
Article10. Percy C, Fritz A, Jack A, Shanmugarathan K, Sobin L, Parkin DM, Whelan S. International classification of diseases for oncology. Geneva: World Health Organization;2000.11. Ko SH, Kim DJ, Park JH, Park CY, Jung CH, Kwon HS, Park JY, Song KH, Han K, Lee KU, Ko KS. Task Force Team for Diabetes Fact Sheet of the Korean Diabetes Association. Trends of antidiabetic drug use in adult type 2 diabetes in Korea in 2002–2013: nationwide population-based cohort study. Medicine (Baltimore). 2016; 95:e4018.12. Badawi A, Ryoo SG. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): a systematic review and meta-analysis. Int J Infect Dis. 2016; 49:129–33.
Article13. Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, Ji R, Wang H, Wang Y, Zhou Y. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020; 94:91–5.
Article14. Carey IM, Critchley JA, DeWilde S, Harris T, Hosking FJ, Cook DG. Risk of infection in type 1 and type 2 diabetes compared with the general population: a matched cohort study. Diabetes Care. 2018; 41:513–21.
Article15. Harding JL, Benoit SR, Gregg EW, Pavkov ME, Perreault L. Trends in rates of infections requiring hospitalization among adults with versus without diabetes in the U.S., 2000–2015. Diabetes Care. 2020; 43:106–16.
Article16. Hine JL, de Lusignan S, Burleigh D, Pathirannehelage S, Mc-Govern A, Gatenby P, Jones S, Jiang D, Williams J, Elliot AJ, Smith GE, Brownrigg J, Hinchliffe R, Munro N. Association between glycaemic control and common infections in people with type 2 diabetes: a cohort study. Diabet Med. 2017; 34:551–7.
Article17. Harding JL, Pavkov ME, Magliano DJ, Shaw JE, Gregg EW. Global trends in diabetes complications: a review of current evidence. Diabetologia. 2019; 62:3–16.
Article18. Casqueiro J, Casqueiro J, Alves C. Infections in patients with diabetes mellitus: a review of pathogenesis. Indian J Endocrinol Metab. 2012; 16(Suppl 1):S27–36.19. Mancuso P. The role of adipokines in chronic inflammation. Immunotargets Ther. 2016; 5:47–56.
Article20. Peleg AY, Weerarathna T, McCarthy JS, Davis TM. Common infections in diabetes: pathogenesis, management and relationship to glycaemic control. Diabetes Metab Res Rev. 2007; 23:3–13.
Article21. Seo DH, Kang S, Lee YH, Ha JY, Park JS, Lee BW, Kang ES, Ahn CW, Cha BS. Current management of type 2 diabetes mellitus in primary care clinics in Korea. Endocrinol Metab (Seoul). 2019; 34:282–90.
Article22. Ko SH, Han K, Lee YH, Noh J, Park CY, Kim DJ, Jung CH, Lee KU, Ko KS. TaskForce Team for the Diabetes Fact Sheet of the Korean Diabetes Association. Past and Current status of adult type 2 diabetes mellitus management in Korea: a National Health Insurance Service database analysis. Diabetes Metab J. 2018; 42:93–100.
Article23. World Health Organization. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). Geneva: World Health Organization;2020. p. p1–40.24. Baker MG, Barnard LT, Kvalsvig A, Verrall A, Zhang J, Keall M, Wilson N, Wall T, Howden-Chapman P. Increasing incidence of serious infectious diseases and inequalities in New Zealand: a national epidemiological study. Lancet. 2012; 379:1112–9.
Article25. Vijayanand P, Wilkins E, Woodhead M. Severe acute respiratory syndrome (SARS): a review. Clin Med (Lond). 2004; 4:152–60.
Article26. Patel JA, Nielsen FB, Badiani AA, Assi S, Unadkat VA, Patel B, Ravindrane R, Wardle H. Poverty, inequality and COVID-19: the forgotten vulnerable. Public Health. 2020; 183:110–1.
Article