Deterioration of Sleep Quality According to Glycemic Status
- Affiliations
-
- 1Eulji University College of Nursing, Daejeon, Korea.
- 2Division of Endocrinology, Department of Internal Medicine, Daejeon Eulji Medical Center, Eulji University School of Medicine, Daejeon, Korea.
- KMID: 2513030
- DOI: http://doi.org/10.4093/dmj.2019.0125
Abstract
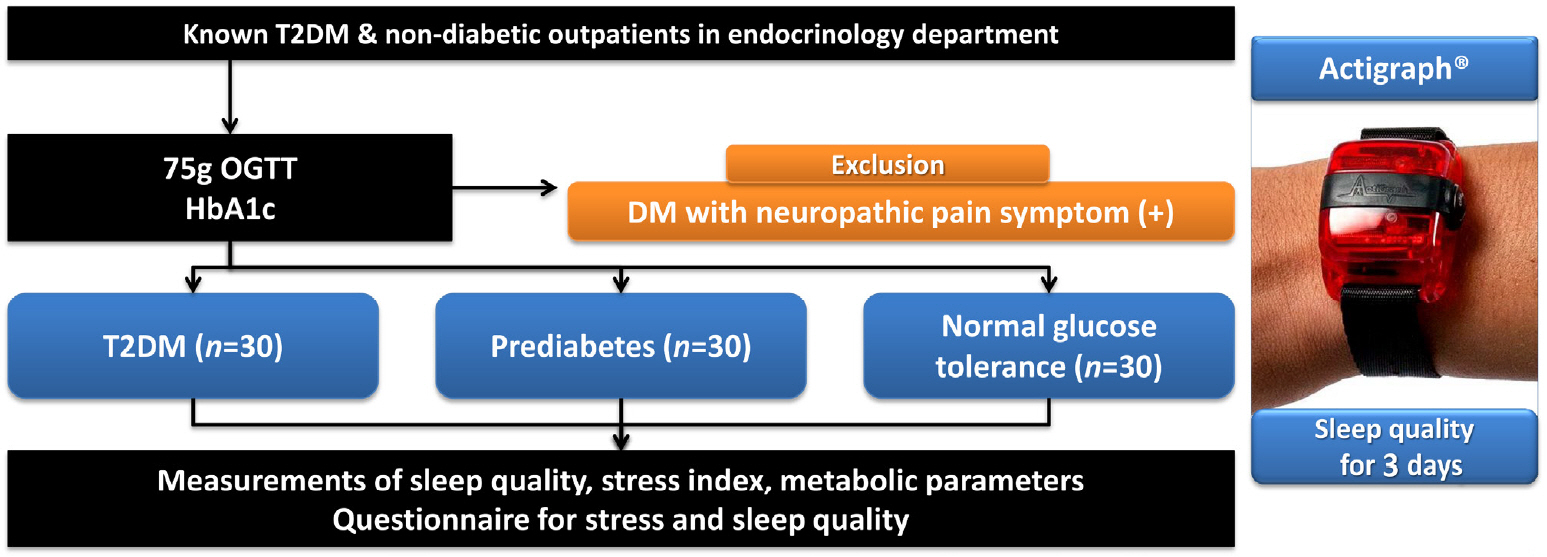
Background Type 2 diabetes mellitus (T2DM) is a progressive disease with multiple complications. The present study aimed to determine the effects of glycemic status on sleep quality in individuals with T2DM, prediabetes, and normal glucose tolerance (NGT).
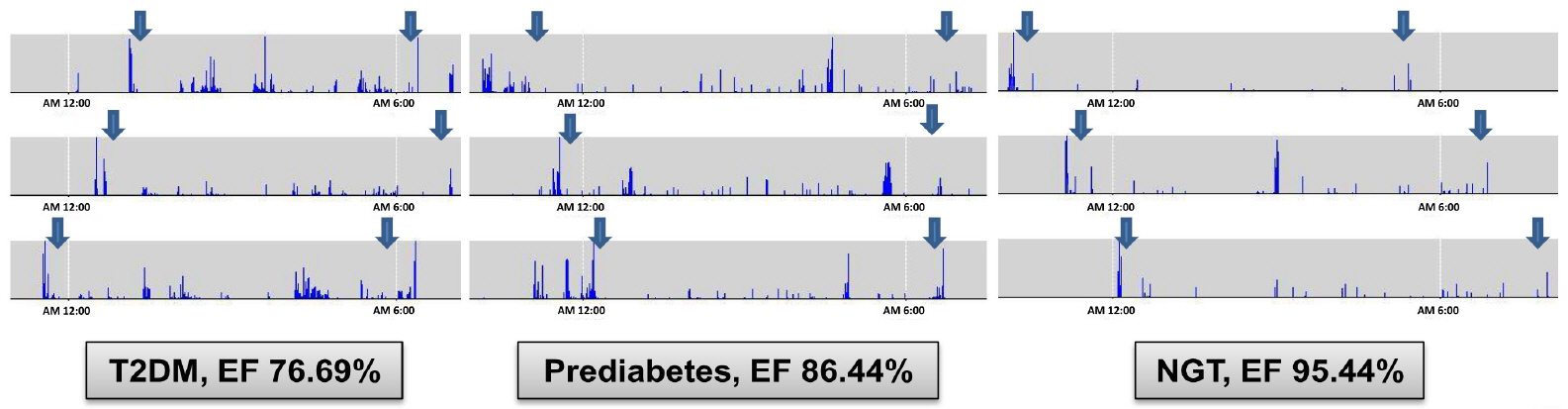
Methods A total of 90 participants were categorized into three groups, T2DM (
n =30), prediabetes (n =30), and NGT (n =30). Objective sleep quality was measured with the actigraph wrist-worn device over 3 nights and subjective sleep quality was evaluated with a questionnaire.Results The duration of diabetes in the T2DM group was 2.23 years and the glycosylated hemoglobin (HbA1c) levels in the T2DM, prediabetes, and NGT groups were 7.83%, 5.80%, and 5.31%, respectively. Sleep efficiency decreased across the T2DM, prediabetes, and NGT groups (86.25%, 87.99%, and 90.22%, respectively;
P =0.047). Additionally, HbA1c levels revealed a significant negative correlation with sleep efficiency (r =−0.348,P =0.001). The sleep quality questionnaire results were similar among the three groups.Conclusion Although the participants in the present study were not necessarily conscious of their sleep disturbances, deterioration in sleep quality progressed according to glycemic status.
Figure
Cited by 1 articles
-
Early Development of Bidirectional Associations between Sleep Disturbance and Diabetes
Yongin Cho
Diabetes Metab J. 2020;44(5):668-670. doi: 10.4093/dmj.2020.0198.
Reference
-
1. Lorenzo C, Wagenknecht LE, D’Agostino RB Jr, Rewers MJ, Karter AJ, Haffner SM. Insulin resistance, beta-cell dysfunction, and conversion to type 2 diabetes in a multiethnic population: the Insulin Resistance Atherosclerosis Study. Diabetes Care. 2010; 33:67–72.2. Kitabchi AE, Temprosa M, Knowler WC, Kahn SE, Fowler SE, Haffner SM, Andres R, Saudek C, Edelstein SL, Arakaki R, Murphy MB, Shamoon H. Diabetes Prevention Program Research Group. Role of insulin secretion and sensitivity in the evolution of type 2 diabetes in the diabetes prevention program: effects of lifestyle intervention and metformin. Diabetes. 2005; 54:2404–2414.
Article3. Reichard P, Nilsson BY, Rosenqvist U. The effect of long-term intensified insulin treatment on the development of microvascular complications of diabetes mellitus. N Engl J Med. 1993; 329:304–309.
Article4. Yoo M, Sharma N, Pasnoor M, Kluding PM. Painful diabetic peripheral neuropathy: presentations, mechanisms, and exercise therapy. J Diabetes Metab. 2013; Suppl 10:005.
Article5. Iqbal Z, Azmi S, Yadav R, Ferdousi M, Kumar M, Cuthbertson DJ, Lim J, Malik RA, Alam U. Diabetic peripheral neuropathy: epidemiology, diagnosis, and pharmacotherapy. Clin Ther. 2018; 40:828–849.
Article6. Neumann C, Martinez D, Schmid H. Nocturnal oxygen desaturation in diabetic patients with severe autonomic neuropathy. Diabetes Res Clin Pract. 1995; 28:97–102.
Article7. Surani S, Brito V, Surani A, Ghamande S. Effect of diabetes mellitus on sleep quality. World J Diabetes. 2015; 6:868–873.
Article8. Ficker JH, Dertinger SH, Siegfried W, Konig HJ, Pentz M, Sailer D, Katalinic A, Hahn EG. Obstructive sleep apnoea and diabetes mellitus: the role of cardiovascular autonomic neuropathy. Eur Respir J. 1998; 11:14–19.
Article9. Lou P, Zhang P, Zhang L, Chen P, Chang G, Zhang N, Li T, Qiao C. Effects of sleep duration and sleep quality on prevalence of type 2 diabetes mellitus: a 5-year follow-up study in China. Diabetes Res Clin Pract. 2015; 109:178–184.
Article10. Knutson KL. Impact of sleep and sleep loss on glucose homeostasis and appetite regulation. Sleep Med Clin. 2007; 2:187–197.
Article11. Mesarwi O, Polak J, Jun J, Polotsky VY. Sleep disorders and the development of insulin resistance and obesity. Endocrinol Metab Clin North Am. 2013; 42:617–634.
Article12. Jaiswal M, Divers J, Dabelea D, Isom S, Bell RA, Martin CL, Pettitt DJ, Saydah S, Pihoker C, Standiford DA, Dolan LM, Marcovina S, Linder B, Liese AD, Pop-Busui R, Feldman EL. Prevalence of and risk factors for diabetic peripheral neuropathy in youth with type 1 and type 2 diabetes: SEARCH for Diabetes in Youth Study. Diabetes Care. 2017; 40:1226–1232.
Article13. Nisar MU, Asad A, Waqas A, Ali N, Nisar A, Qayyum MA, Maryam H, Javaid M, Jamil M. Association of diabetic neuropathy with duration of type 2 diabetes and glycemic control. Cureus. 2015; 7:e302.
Article14. Lee CC, Perkins BA, Kayaniyil S, Harris SB, Retnakaran R, Gerstein HC, Zinman B, Hanley AJ. Peripheral neuropathy and nerve dysfunction in individuals at high risk for type 2 diabetes: the PROMISE cohort. Diabetes Care. 2015; 38:793–800.
Article15. Hong JH, Chung HK, Park HY, Joung KH, Lee JH, Jung JG, Kim KS, Kim HJ, Ku BJ, Shong M. GDF15 is a novel biomarker for impaired fasting glucose. Diabetes Metab J. 2014; 38:472–479.
Article16. Snyder-Halpern R, Verran JA. Instrumentation to describe subjective sleep characteristics in healthy subjects. Res Nurs Health. 1987; 10:155–163.
Article17. Fujihara K, Kodama S, Horikawa C, Yoshizawa S, Sugawara A, Hirasawa R, Shimano H, Yachi Y, Suzuki A, Hanyu O, Sone H. The relationship between diabetic neuropathy and sleep apnea syndrome: a meta-analysis. Sleep Disord. 2013; 2013:150371.
Article18. Mallien J, Isenmann S, Mrazek A, Haensch CA. Sleep disturbances and autonomic dysfunction in patients with postural orthostatic tachycardia syndrome. Front Neurol. 2014; 5:118.
Article19. Benichou T, Pereira B, Mermillod M, Tauveron I, Pfabigan D, Maqdasy S, Dutheil F. Heart rate variability in type 2 diabetes mellitus: a systematic review and meta-analysis. PLoS One. 2018; 13:e0195166.
Article20. Petropoulos IN, Ponirakis G, Khan A, Almuhannadi H, Gad H, Malik RA. Diagnosing diabetic neuropathy: something old, something new. Diabetes Metab J. 2018; 42:255–269.
Article21. Kopf S, Groener JB, Kender Z, Fleming T, Bischoff S, Jende J, Schumann C, Ries S, Bendszus M, Schuh-Hofer S, Treede RD, Nawroth PP. Deep phenotyping neuropathy: an underestimated complication in patients with pre-diabetes and type 2 diabetes associated with albuminuria. Diabetes Res Clin Pract. 2018; 146:191–201.
Article22. Farabi SS, Quinn L, Carley DW. Validity of actigraphy in measurement of sleep in young adults with type 1 diabetes. J Clin Sleep Med. 2017; 13:669–674.
Article23. Blackwell T, Redline S, Ancoli-Israel S, Schneider JL, Surovec S, Johnson NL, Cauley JA, Stone KL;. Comparison of sleep parameters from actigraphy and polysomnography in older women: the SOF study. Sleep. 2008; 31:283–291.
Article24. Marino M, Li Y, Rueschman MN, Winkelman JW, Ellenbogen JM, Solet JM, Dulin H, Berkman LF, Buxton OM. Measuring sleep: accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. Sleep. 2013; 36:1747–1755.
Article25. Pop-Busui R, Boulton AJ, Feldman EL, Bril V, Freeman R, Malik RA, Sosenko JM, Ziegler D. Diabetic neuropathy: a position statement by the American Diabetes Association. Diabetes Care. 2017; 40:136–154.
Article26. Yun JS, Ko SH. Risk factors and adverse outcomes of severe hypoglycemia in type 2 diabetes mellitus. Diabetes Metab J. 2016; 40:423–432.
Article27. Pillar G, Schuscheim G, Weiss R, Malhotra A, McCowen KC, Shlitner A, Peled N, Shehadeh N. Interactions between hypoglycemia and sleep architecture in children with type 1 diabetes mellitus. J Pediatr. 2003; 142:163–168.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sleep and Type 2 Diabetes
- The Relationship between Sleep Quality and Stress among Nursing Students in Korea
- Quality of Sleep and Its Influencing Factors in the Institutionalized Elderly
- The relationship between poor sleep quality measured by the Pittsburgh Sleep Quality Index and smoking status according to sex and age: an analysis of the 2018 Korean Community Health Survey
- Managing Sleep Disorders through Lifestyle Choices: A Focus on Nutrition