Clin Exp Otorhinolaryngol.
2021 Feb;14(1):88-92. 10.21053/ceo.2020.00143.
Effects of Olfactory Training in Patients With Postinfectious Olfactory Dysfunction
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Konkuk University School of Medicine, Seoul, Korea
- KMID: 2512886
- DOI: http://doi.org/10.21053/ceo.2020.00143
Abstract
Objectives
. Postinfectious olfactory dysfunction (PIOD) is the most common etiology of olfactory dysfunction, and olfactory training (OT) is an accepted treatment modality for PIOD. Some studies have investigated OT in Korean patients, but they involved odorants unfamiliar to Koreans or had no control group. The aim of this study was to verify the efficacy of OT in PIOD patients, using odorants familiar to Koreans and including a control group.
Methods
. We enrolled a total of 104 Korean patients with PIOD over the 3-year study period. All participants were assessed using endoscopy and an olfactory function test at the baseline assessment and 3 months after OT. The olfactory function test was performed using the Korean version of Sniffin’ stick (KVSS) II. Nasal and psychological function was evaluated using a visual analog scale and the Mini-Mental State Examination. OT was performed over a period of 3 months, using five odorants (rose, lemon, cinnamon, orange, and peach).
Results
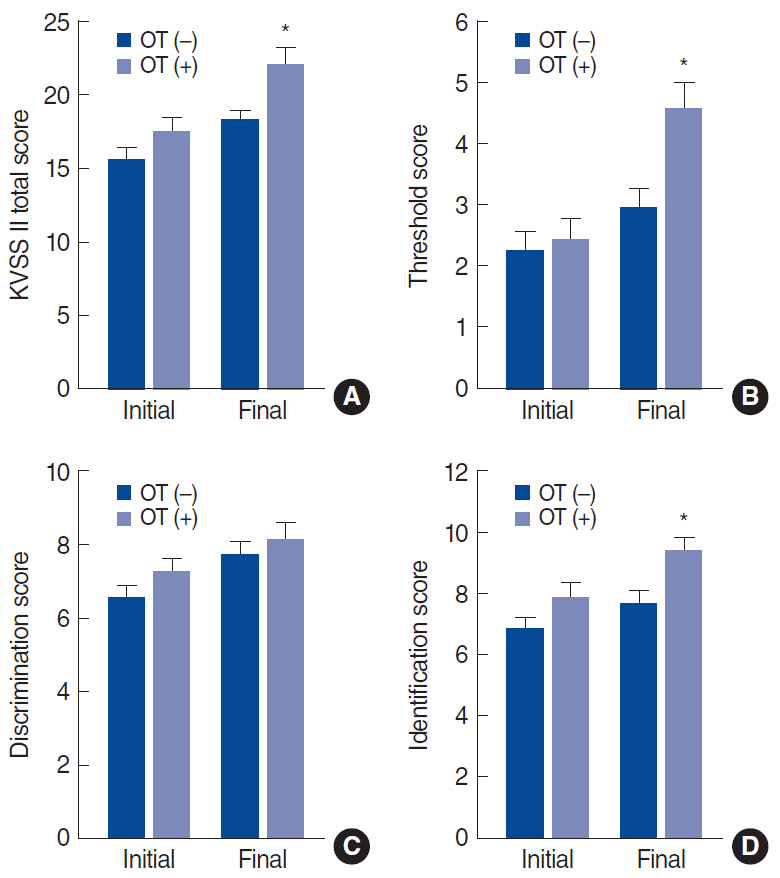
. OT improved olfactory function in approximately 40% of subjects over a period of 12 weeks compared to non-OT subjects. A comparison of changes between the initial and follow-up assessments demonstrated that the OT group had significantly better olfactory results for the total KVSS II, threshold, and identification scores than the non-OT group. The degree of olfactory improvement after OT was affected by the initial score.
Conclusion
. The effects of OT in patients with PIOD were demonstrated in this study. A meaningful contribution of this study is that Korean patients were tested using odors familiar to them in comparison with a control group.
Keyword
Figure
Cited by 1 articles
-
Comparative Analysis of Olfactory and Gustatory Function of Patients With COVID-19 Olfactory Dysfunction and Non-COVID-19 Postinfectious Olfactory Dysfunction
Taesik Jung, Bo Yoon Choi, Minho Jang, Taehee Kim, EunHye Seo, Jin Kook Kim
J Korean Med Sci. 2023;38(43):e352. doi: 10.3346/jkms.2023.38.e352.
Reference
-
1. Nordin S, Bramerson A. Complaints of olfactory disorders: epidemiology, assessment and clinical implications. Curr Opin Allergy Clin Immunol. 2008; Feb. 8(1):10–5.
Article2. Deems DA, Doty RL, Settle RG, Moore-Gillon V, Shaman P, Mester AF, et al. Smell and taste disorders, a study of 750 patients from the University of Pennsylvania Smell and Taste Center. Arch Otolaryngol Head Neck Surg. 1991; May. 117(5):519–28.
Article3. Damm M, Temmel A, Welge-Lussen A, Eckel HE, Kreft MP, Klussmann JP, et al. Olfactory dysfunctions: epidemiology and therapy in Germany, Austria and Switzerland. HNO. 2004; Feb. 52(2):112–20.4. Seiden AM. Postviral olfactory loss. Otolaryngol Clin North Am. 2004; Dec. 37(6):1159–66.
Article5. Damm M, Pikart LK, Reimann H, Burkert S, Goktas O, Haxel B, et al. Olfactory training is helpful in postinfectious olfactory loss: a randomized, controlled, multicenter study. Laryngoscope. 2014; Apr. 124(4):826–31.
Article6. Hummel T, Rissom K, Reden J, Hahner A, Weidenbecher M, Huttenbrink KB. Effects of olfactory training in patients with olfactory loss. Laryngoscope. 2009; 119(3):496–9.
Article7. Cockrell JR, Folstein MF. Mini-Mental State Examination (MMSE). Psychopharmacol Bull. 1988; 24(4):689–92.8. Altundag A, Cayonu M, Kayabasoglu G, Salihoglu M, Tekeli H, Saglam O, et al. Modified olfactory training in patients with postinfectious olfactory loss. Laryngoscope. 2015; Aug. 125(8):1763–6.
Article9. Takagi SF. A standardized olfactometer in Japan: a review over ten years. Ann N Y Acad Sci. 1987; 510:113–8.10. Kim JM, Jeong MS, Shin DH, Seol JH, Hong SC, Cho JH, et al. Olfactory identification test using familiar distracters for Koreans. Clin Exp Otorhinolaryngol. 2014; Mar. 7(1):19–23.
Article11. Saito S, Ayabe-Kanamura S, Takashima Y. A smell test based on odor classification of Japanese people. Chem Senses. 1995; Jun. 20(3):379.12. Pekala K, Chandra RK, Turner JH. Efficacy of olfactory training in patients with olfactory loss: a systematic review and meta-analysis. Int Forum Allergy Rhinol. 2016; Mar. 6(3):299–307.
Article13. Whitcroft KL, Hummel T. Clinical diagnosis and current management strategies for olfactory dysfunction: a review. JAMA Otolaryngol Head Neck Surg. 2019; July. 145(9):846–53.14. Qiao XF, Wang GP, Li X, Bai YH, Zheng W. Analysis of the clinical effect of olfactory training on olfactory dysfunction after upper respiratory tract infection. Acta Otolaryngol. 2019; Jul. 139(7):643–6.
Article15. Sorokowska A, Drechsler E, Karwowski M, Hummel T. Effects of olfactory training: a meta-analysis. Rhinology. 2017; Mar. 55(1):17–26.
Article16. Oleszkiewicz A, Hanf S, Whitcroft KL, Haehner A, Hummel T. Examination of olfactory training effectiveness in relation to its complexity and the cause of olfactory loss. Laryngoscope. 2018; Jul. 128(7):1518–22.
Article17. Fleiner F, Lau L, Goktas O. Active olfactory training for the treatment of smelling disorders. Ear Nose Throat J. 2012; May. 91(5):198–215. 198-203,215.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparative Analysis of Olfactory and Gustatory Function of Patients With COVID-19 Olfactory Dysfunction and Non-COVID-19 Postinfectious Olfactory Dysfunction
- Comparing the Effectiveness of Olfactory Training, According as Type and Preference of Odorant
- The Effects of Olfactory Training with Intranasal Corticosteroid Spray in Korean Patients with Olfactory Dysfunction
- A review on photobiomodulation therapy for olfactory dysfunction caused by COVID-19
- The Sniffing Bead System as a Useful Diagnostic Tool for Olfactory Dysfunction in COVID-19