Ann Lab Med.
2021 Jan;41(1):95-100. 10.3343/alm.2021.41.1.95.
Platelet Inventory Management Program: Development and Practical Experience
- Affiliations
-
- 1Department of Laboratory Medicine and Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea
- KMID: 2512738
- DOI: http://doi.org/10.3343/alm.2021.41.1.95
Abstract
- Background
Patients with ongoing or expected bleeding require platelet (PLT) transfusions; however, owing to the testing required after a blood donation, manufacturing PLT products may take 1.5–2.0 days after a request is made. This supply-demand mismatch leads clinicians to retain spare PLTs for transfusions, leading to increased PLT discard rates. We developed a PLT inventory management program to supply PLTs more efficiently to patients requiring PLT transfusions within the expiration date, while reducing PLT discard rates.
Methods
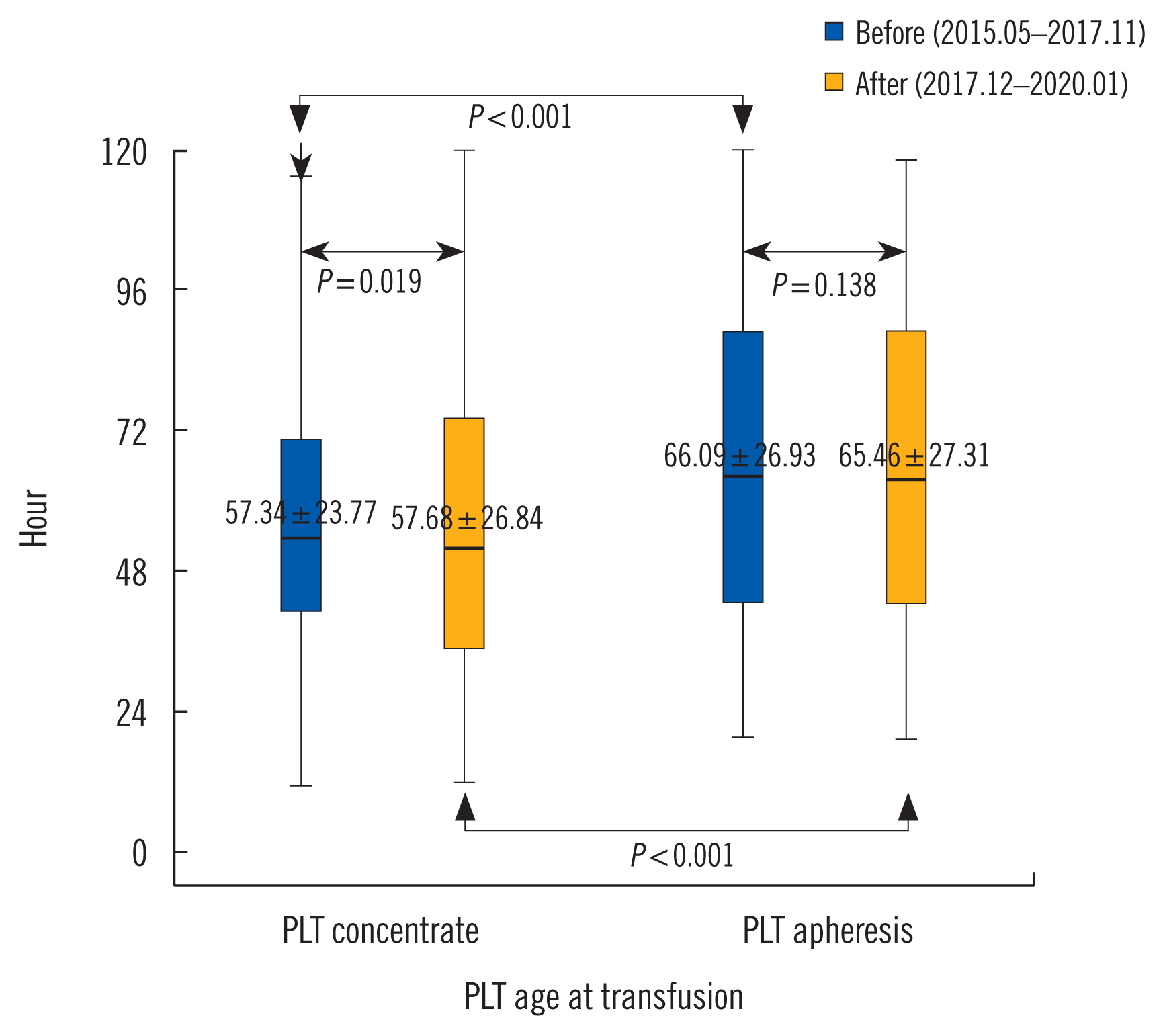
PLT concentrates (58,863 and 58,357 units) and apheresis products (7,905 and 8,441 units) were analyzed from May 2015 to November 2017 and from December 2017 to January 2020, respectively. We developed a program to manage total PLT inventories and prospective PLT transfusion patients based on blood type, blood product, and remaining period of efficacy; the program facilitates PLT preparation transfer to non-designated patients within the remaining period of efficacy.
Results
The overall PLT concentrate discard rate was 3,254 (2.78%): 1,811 (3.07%) units before and 1,443 units (2.41%) after program application (P < 0.001). The discard rate owing to expiration was reduced from 69 units (3.81%) before to two units (0.14%) after program application (P < 0.001).
Conclusions
This program can guide the allocation of PLT preparations based on the remaining period of efficacy, enabling PLT products to be used before their expiration date and reducing PLT product discard rate.
Keyword
Figure
Reference
-
1. Veihola M, Aroviita P, Linna M, Sintonen H, Kekomäki R. Variation of platelet production and discard rates in 17 blood centers representing 10 European countries from 2000 to 2002. Transfusion. 2006; 46:991–5.
Article2. Handigund M, Cho YG. Insights into platelet storage and the need for multiple approaches. Ann Clin Lab Sci. 2015; 45:713–9.3. de Kort W, Janssen M, Kortbeek N, Jansen N, van der Wal J, van Dijk N. Platelet pool inventory management: theory meets practice. Transfusion. 2011; 51:2295–303.
Article4. Blake JT. On the use of operational research for managing platelet inventory and ordering. Transfusion. 2009; 49:396–401.5. Flint AW, McQuilten ZK, Irwin G, Rushford K, Haysom HE, Wood EM. Is platelet expiring out of date? A systematic review. Transfus Med Rev. 2020; 34:42–50.
Article6. Gomez AT, Quinn JG, Doiron DJ, Watson S, Crocker BD, Cheng CK. Implementation of a novel real-time platelet inventory management system at a multi-site transfusion service. Transfusion. 2015; 55:2070–5.
Article7. Fuller AK, Uglik KM, Braine HG, King KE. A comprehensive program to minimize platelet outdating. Transfusion. 2011; 51:1469–76.
Article8. Fillet AM, Desmarets M, Assari S, Quaranta JF, François A, Pugin A, et al. Blood products use in France: a nationwide cross-sectional survey. Transfusion. 2016; 56:3033–41.
Article9. Fedele PL, Polizzotto MN, Grigoriadis G, Waters N, Comande M, Borosak M, et al. Profiling clinical platelet and plasma use to inform blood supply and contingency planning: PUPPY, the prospective utilization of platelets and plasma study. Transfusion. 2016; 56:2455–65.
Article10. van Dijk N, Haijema R, van der Wal J, Sibinga CS. Blood platelet production: a novel approach for practical optimization. Transfusion. 2009; 49:411–20.
Article11. Whitaker B, Rajbhandary S, Kleinman S, Harris A, Kamani N. Trends in United States blood collection and transfusion: results from the 2013 AABB Blood Collection, Utilization, and Patient Blood Management Survey. Transfusion. 2016; 56:2173–83.
Article12. Jo SA, Hwang WJ, Kim SY, Kim YJ, Kim HH, Chang CH, et al. Study for efficient blood management using evaluation the blood wastage statements in Pusan University Hospital. Korean J Blood Transfus. 2008; 19:25–32.13. Kim BC, Seo YI, Chai DR, Shin JW, Choi TY. Analysis of discarded blood components at a university hospital in Korea. Korean J Blood Transfus. 2011; 22:120–6.14. Kwon JR, Lee SW, Cho YH, Kwon YH, Kim HJ, Lee HJ, et al. An analysis of blood usage and blood wastage in Korea hospitals in 2008. Korean J Blood Transfus. 2009; 20:184–94.15. Collins RA, Wisniewski MK, Waters JH, Triulzi DJ, Yazer MH. Effectiveness of multiple initiatives to reduce blood component wastage. Am J Clin Pathol. 2015; 143:329–35.
Article16. Javadzadeh Shahshahani H, Taghvai N. Blood wastage management in a regional blood transfusion centre. Transfus Med. 2017; 27(S5):348–53.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A study on a nursing curriculum after a basic 3-year diploma course for the baccalaureate degree
- A Study on the Development of a Computer-Assisted Program for Elementary School Foodservice(I)-Based on Foodservice Management
- Executive Strategies for CPD Program Development and Enhancement
- Proposal for an Ideal Management System for Hematopoietic Stem Cells in Korea
- The Inventory Levels of Red Blood Cells from Sentinel Hospitals in Korea according to the Blood Type