J Korean Soc Matern Child Health.
2021 Jan;25(1):55-62. 10.21896/jksmch.2021.25.1.55.
Serum Ferritin Concentration in the Early Third Trimester of Pregnancy and Risk of Preterm Birth and Low Birth Weight Based on Gestational Age
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Kangwon National University School of Medicine, Chuncheon, Korea
- KMID: 2512485
- DOI: http://doi.org/10.21896/jksmch.2021.25.1.55
Abstract
Objective
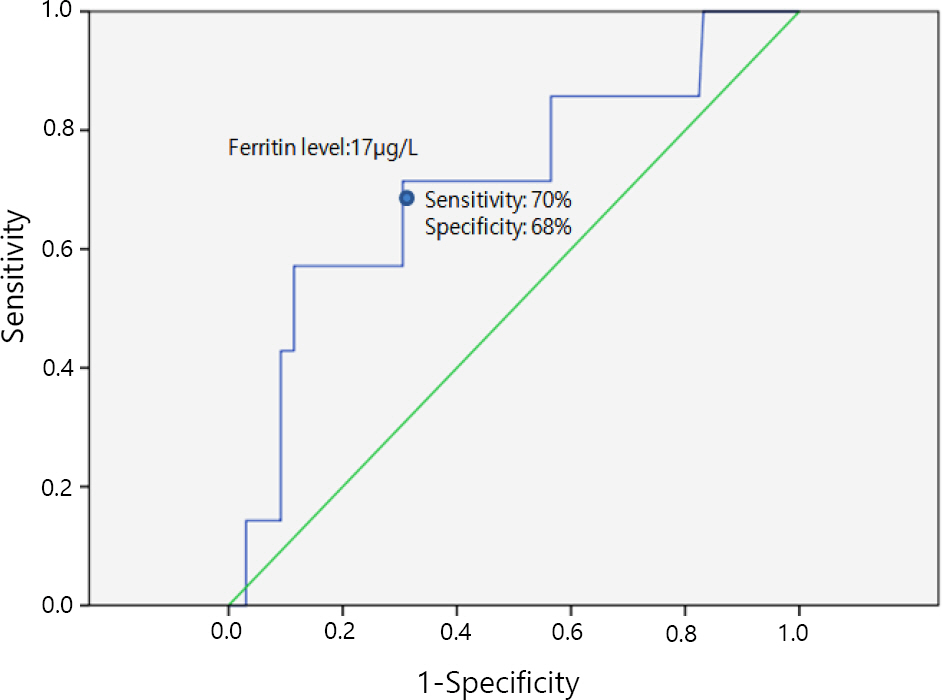
Although serum ferritin is considered the best measure of total body iron, with low levels indicating iron deficiency, recent studies have shown that high levels are associated with gestational diabetes, premature birth, and low birth weight. This study aimed to analyze the association between serum ferritin levels in the third trimester of pregnancy and low birth weight and preterm birth.
Methods
This study included pregnant women who delivered a single fetus at Kangwon National University Hospital between January 2009 and December 2013 and in whom serum ferritin levels were measured between 28 and 34 weeks of gestation. The association between serum ferritin levels measured in the early third trimester of pregnancy and preterm birth and low birth weight infants was analyzed.
Results
A total of 1,079 women fulfilled the study criteria and had their serum ferritin level measured during the third trimester (28–33.9 weeks of gestation) and later delivered at Kangwon National University Hospital. Comparison of the group with serum ferritin levels above the 75th percentile and those below the 25th percentile at the beginning of the third trimester revealed that the incidence of preterm births (<34 weeks of gestation, <37 weeks of gestation) and low birth weight were significantly higher in the group with serum ferritin levels above the 75th percentile than those below the 25th percentile (p<0.05). When variable factors were controlled through multiple regression analysis, the group whose serum ferritin levels were above the 75th percentile at 30–31.9 weeks of gestation had the highest risk of preterm birth before 34 weeks of gestation (adjusted odds ratio [OR], 7.85; 95% confidence interval [CI], 1.32–29.9) and low birth weight (adjusted OR, 6.49; 95% CI, 2.10–20.0).
Conclusion
In this study, when serum ferritin was high in the third trimester of pregnancy, it was significantly increased with preterm birth (<34 and 37 weeks) and low birth weight. In particular, when serum ferritin levels were high at 30–31.9 weeks of gestation, the risk of premature birth before 34 weeks and low birth weight was statistically highest.
Figure
Cited by 2 articles
-
Development Process for Preterm Birth Risk Assessment Scale in High-Risk Pregnancy: 1st Phase of Preliminary Scale Development
Jeung-Im Kim
J Korean Soc Matern Child Health. 2022;26(3):171-182. doi: 10.21896/jksmch.2022.26.3.171.Iron Deficiency Anemia in Pregnancy
Seung-Woo Yang, Yong-Soo Seo
J Korean Soc Matern Child Health. 2023;27(2):45-50. doi: 10.21896/jksmch.2023.27.2.45.
Reference
-
Andrews NC. Disorders of iron metabolism. N Engl J Med. 1999. 341:1986–95.Bothwell TH. Iron requirements in pregnancy and strategies to meet them. Am J Clin Nutr. 2000. 72:257S–64S.Bowers KA., Olsen SF., Bao W., Halldorsson TI., Strøm M., Zhang C. Plasma concentrations of ferritin in early pregnancy are associated with risk of gestational diabetes mellitus in women in the Danish National Birth Cohort. J Nutr. 2016. 146:1756–61.Cao C., Kimberly O., O'Brien KO. Pregnancy and iron homeostasis: an update. Nutr Rev. 2013. 71:35–51.Choi JW., Im MW., Pai SH. Change of erythropoiesis and serum transferrin receptor levels with gestational age in healthy pregnant women. Korean J Hematol. 2000. 35:134–42.Entman SS., Richardson LD., Killam AP. Elevated serum ferritin in the altered ferrokinetics of toxemia of pregnancy. Am J Obstet Gynecol. 1982. 144:418–22.Friedrisch JR., Friedrisch BK. Prophylactic iron supplementation in pregnancy: a controversial issue. Biochem Insights. 2017. 27:1–8.Goldenberg RL., Tamura T., DuBard M., Johnston KE., Copper RL., Neggers Y. Plasma ferritin and pregnancy outcome. Am J Obstet Gynecol. 1996. 175:1356–9.Hwang JY., Lee JY., Kim KN., Kim H., Ha EH., Park H, et al. Maternal iron intake at mid-pregnancy is associated with reduced fetal growth: results from Mothers and Children's Environmental Health (MOCEH) study. Nutr J. 2013. 12:38.Jang HM., Ahn HS. Serum iron concentration of maternal and umbilical cord blood during pregnancy. Korean J Community Nutr. 2005. 10:860–8.Kadyrov M., Kosanke G., Kingdom J., Kaufmann P. Increased fetoplacental angiogenesis during first trimester in anaemic women. Lancet. 1998. 352:1747–9.Klebanoff MA., Shiono PH., Selby JV., Trachtenberg AI., Graubard BI. Anemia and spontaneous preterm birth. Am J Obstet Gynecol. 1991. 164(1 Pt 1):59–63.Knight EM., Spurlock BG., Edwards CH., Johnson AA., Oyemade UJ., Cole OJ, et al. Biochemical profile of African-American women during three trimesters of pregnancy and at delivery. J Nutr. 1994. 124:943S–953S.Lee JI., Im HS. Iron status of pregnant women and evaluation of cut-off levels of Hb, Hct, TIBC, sTfR, sTfR:ferritin ratio for assessment of iron deficiency. Korean J of Human Ecology. 2001. 4:36–45.Milman N., Graudal N., Agger AO. Iron status markers during pregnancy no relationship between levels at the beginning of the second trimester, prior to delivery and postpartum. J Intern Med. 1995. 237:261–7.Pigeon C., Ilyin G., Courselaud B., Leroyer P., Turlin B., Brissot P, et al. A new mouse liver specific gene, encoding a protein homologous to human antimicrobial peptide hepcidin, is overexpressed during iron overoad. J Biol Chem. 2001. 276:7811–9.Ray JG., Berger H., Park AL. Population-based study of serum ferritin in early pregnancy and adverse perinatal outcomes. Paediatr Perinat Epidemiol. 2020. 34:706–12.Rayman MP., Barlis J., Evans RW., Redman CW., King LJ. Abnormal iron parameters in the pregnancy syndrome preeclampsia. Am J Obstet Gynecol. 2002. 187:412–8.Scholl TO. High third-trimester ferritin concentration: associations with very preterm delivery, infection, and maternal nutritional status. Obstet Gynecol. 1998. 92:161–6.Stephansson O., Dickman PW., Johansson A., Cnattingius S. Maternal hemoglobin concentration during pregnancy and risk of stillbirth. JAMA. 2000. 284:2611–7.Theil EC. Ferritin: structure, gene, regulation, and cellular function in animals, plants, and microorganisms. Annu Rev Biochem. 1987. 56:289–315.Weintraub AY., Sheiner E., Mazor M., Levy A., Tevet A., Paamoni O, et al. Maternal serum ferritin concentration in patients with preterm labor and intact membranes. J Matern Fetal Neonatal Med. 2005. 18:163–6.Xiao R., Sorensen TK., Frederick IO., El-Bastawissi A., King IB., Leisenring WM, et al. Maternal second-trimester serum ferritin concentrations and subsequent risk of preterm delivery. Paediatr Perinat Epidemiol. 2002. 16:297–304.Young MF., Oaks BM., Tandon S., Martorell R., Dewey KG., Wendt AS. Maternal hemoglobin concentrations across pregnancy and maternal and child health: a systematic review and meta-analysis. Ann N Y Acad Sci. 2019. 1450:47–68.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship between Maternal Hemoglobin Concentration and Birth Weight of Newborns
- Serum Iron Concentration of Maternal and Umbilical Cord Blood during Pregnancy
- The factors affecting pregnancy outcomes in the second trimester pregnant women
- Maternal Weight Gain Pattern and Birth Weight
- Maternal Plasma Homocysteine Levels and Pregnancy Outcomes