J Korean Soc Matern Child Health.
2021 Jan;25(1):48-54. 10.21896/jksmch.2021.25.1.48.
Risk Factors of the High-Risk Pregnancy and Association with Particulate Matter
- Affiliations
-
- 1College of Nursing Science, Kyung Hee University, Seoul, Korea
- 2Department of Precision Medicine & Biostatistics, Yonsei University Wonju College of Medicine, Wonju, Korea
- KMID: 2512484
- DOI: http://doi.org/10.21896/jksmch.2021.25.1.48
Abstract
- Purpose
High-risk pregnancy, resulting in major complications, such as abortion, gestational hypertension, and preterm labor, are on the rise, requiring intervention. Increased concentration of particulate matter that is 10 μg per cubic meter or less in diameter (PM10) due to increased air pollution and industrialization has recently been noted as a risk factor for health problems, and prior studies have reported that PM10 is related to abortion, gestational hypertension, and preterm labor.
Methods
This study used data from the Korean medical panel between 2008 and 2016 to identify 879 women with normal pregnancies and 301 women diagnosed with high-risk pregnancies. The association between high-risk pregnancy and PM10 was analyzed using the annual average regional concentration during the same period by the Korea Environment Corporation.
Results
At 35 years of age or older, the risk of abortion (p<0.001; 95% confidence interval [CI], 1.43–2.71) and preterm labor increased (p<0.05; 95% CI, 0.33–0.90). Married pregnant women were at a high risk of preterm labor (p<0.05; 95% CI, 0.25–0.98), and the prevalence of gestational hypertension was high in the metropolitan area (p<0.05; 95% CI, 12.09–25.93). On comparing the average annual concentration of particulate matter according to the level of atmospheric ventilation of the Korea Environment Corporation using a cutoff of ≤50 μg/m3, the probability of preterm labor was 2.2 times higher in groups exposed to particulate matter concentration of ≥50 μg/m3 (p<0.01; 95% CI, 1.49–3.25).
Conclusion
PM10 was related to preterm labor, and the risk of preterm labor was high if the average annual concentration of PM10 in the individual’s residential area exceeded 50 μg/m3.
Figure
Reference
-
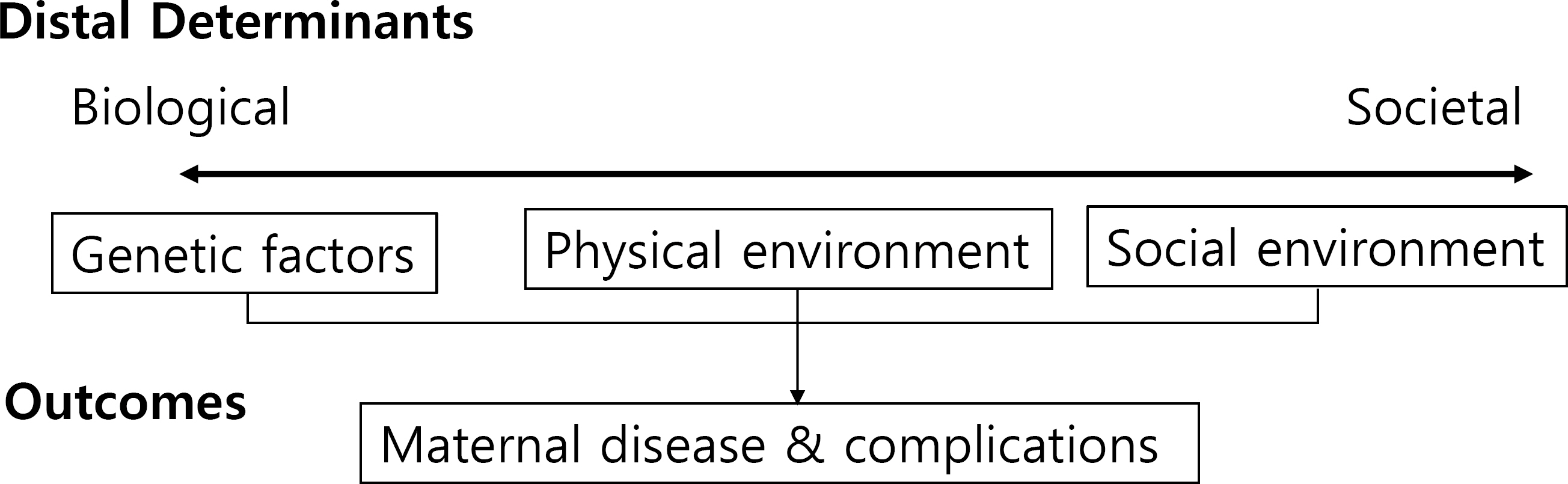
Bae H. Effects of short-term exposure to PM10 and PM2.5 on mortality in Seoul. J Environ Health. 2014. 40:346–54.Dadvand P., Ostro B., Amato F., Figueras F., Minguillón MC., Martinez D, et al. Particulate air pollution and preeclampsia: a source-based analysis. Occup Environ Med. 2014. 71:570–7.Ferguson KK., McElrath TF., Meeker JD. Environmental phthalate exposure and preterm birth. JAMA Pediatr. 2014. 168:61–7.Grippo A., Zhang J., Chu L., Guo Y., Qiao L., Zhang J, et al. Air pollution exposure during pregnancy and spontaneous abortion and stillbirth. Rev Environ Health. 2018. 33:247–64.Han YJ. Analysis on the risk factors of Korea's stillbirth [dissertation]. Seoul (Korea): Yonsei University;2003.Howson CP., Kinney MV., Lawn JE. March of Dimes, PMNCH, Save the children, WHO. Born too soon: the global action report on preterm birth. Geneva (Switzerland): World Health Organization;2012.Huynh M., Spasojevic J., Li W., Maduro G., Van Wye G., Waterman PD, et al. Spatial social polarization and birth outcomes: preterm birth and infant mortality – New York City, 2010–14. Scand J Public Health. 2018. 46:157–66.Jung NY. A study on the factors related to natural heritage in Korea (2008–2014) [dissertation]. Seoul (Korea): Hanyang University;2018.Kintiraki E., Papakatsika S., Kotronis G., Goulis DG., Kotsis V. Pregnancy-Induced hypertension. Hormones (Athens). 2015. 14:211–23.Lamichhane DK., Leem JH., Lee JY., Kim HC. A meta-analysis of exposure to particulate matter and adverse birth outcomes. Environ Health Toxicol. 2015. 30:e2015011.Lee SY. Policy challenges for pregnancy after the age of 35 years. Health Welf Policy Forum. 2014. 213:24–35.Liu C., Sun J., Liu Y., Liang H., Wang M., Wang C, et al. Different exposure levels of fine particulate matter and preterm birth: a meta-analysis based on cohort studies. Environ Sci Pollut Res Int. 2017. 24:17976–84.Männistö T., Mendola P., Liu D., Leishear K., Sherman S., Laughon SK. Acute air pollution exposure and blood pressure at delivery among women with and without hypertension. Am J Hypertens. 2015. 28:58–72.Misra DP., Guyer B., Allston A. Integrated perinatal health framework. A multiple determinants model with a life span approach. Am J Prev Med. 2003. 25:65–75.Nobles CJ., Williams A., Ouidir M., Sherman S., Mendola P. Differential effect of ambient air pollution exposure on risk of gestational hypertension and preeclampsia. Hypertension. 2019. 74:384–90.Parker JD., Woodruff TJ., Basu R., Schoendorf KC. Air pollution and birth weight among term infants in California. Pediatrics. 2005. 115:121–8.Savitz DA., Danilack VA., Engel SM., Elston B., Lipkind HS. Descriptive epidemiology of chronic hypertension, gestational hypertension, and preeclampsia in New York State, 1995–2004. Matern Child Health J. 2014. 18:829–38.Sepidarkish M., Almasi-Hashiani A., Maroufizadeh S., Vesali S., Pirjani R., Samani RO. Association between previous spontaneous abortion and pre-eclampsia during a subsequent pregnancy. Int J Gynaecol Obstet. 2017. 136:83–6.Shin HC. Analysis of high-risk maternal pregnancy and childbirth-related medical trends [Internet]. Wonju (Korea): Health Insurance Review & Assessment Service;2012. [cited 2021 Jan 5]. Available from:. http://repository.hira.or.kr/handle/2019.oak/868.Women's Health Nursing Research Society. Women's health nursing II. 10th ed. Seoul (Korea): Soomunsa;2020.Zaman U., Nazir A., Taimoor A., Shah I., Fatima S., Jadoon H. Association of risk factors with spontaneous preterm labour with intact foetal membranes. J Ayub Med Coll Abbottabad. 2019. 31:536–40.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Health effects of particulate matter
- Association of Particulate Matter With ENT Diseases
- The Relationships between Particulate Matter Risk Perception, Knowledge, and Health Promoting Behaviors among College Students
- Reclassification of High-Risk Pregnancy for Maternal-Fetal Healthcare Providers
- Ambient Particulate Matter and the Risk of Deaths from Cardiovascular and Cerebrovascular Disease