Association of Quantitative Flow Ratio with Lesion Severity and Its Ability to Discriminate Myocardial Ischemia
- Affiliations
-
- 1Department of Cardiology, Zhongshan Hospital, Fudan University, Shanghai Institute of Cardiovascular Diseases, Shanghai, China
- 2Department of Internal Medicine and Cardiovascular Center, Seoul National University Hospital, Seoul, Korea
- 3Division of Cardiology, Department of Internal Medicine, Heart Vascular Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Department of Cardiology, China-Japan Union Hospital of Jilin University, Jilin, China
- 5Department of Internal Medicine, Sejong General Hospital, Bucheon, Korea
- 6Department of Nuclear Medicine, Seoul National University Hospital, Seoul, Korea
- 7Institute on Aging, Seoul National University, Seoul, Korea
- KMID: 2512450
- DOI: http://doi.org/10.4070/kcj.2020.0375
Abstract
- Background and Objectives
Quantitative flow ratio (QFR) is an angiography-based technique for functional assessment of coronary artery stenosis. This study investigated the response of QFR to different degree of stenosis severity and its ability to predict the positron emission tomography (PET)-defined myocardial ischemia.
Methods
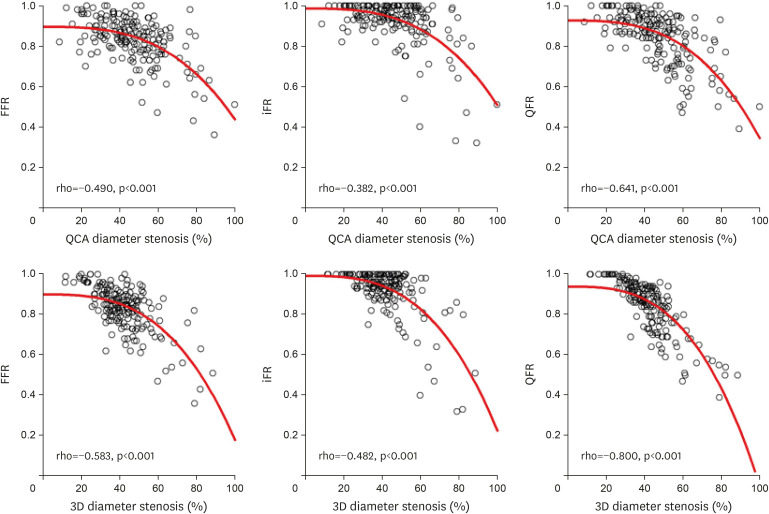
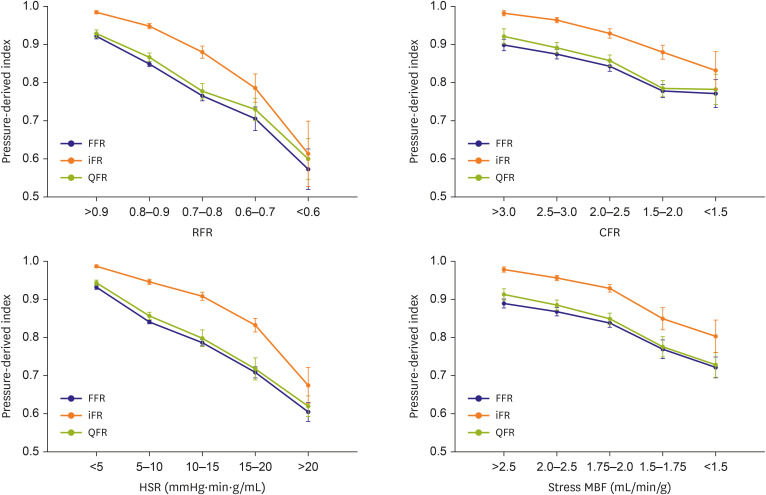
From 109 patients with 185 vessels who underwent both 13 N-ammonia PET and invasive physiological measurement, we compared QFR, fractional flow reserve (FFR) and instantaneous wave-free ratio (iFR) for the responses to the different degree of anatomical (percent diameter stenosis [%DS]) and hemodynamic (relative flow reserve [RFR], coronary flow reserve, hyperemic stenosis resistance, and stress myocardial flow) stenosis severity and diagnostic performance against PET-derived parameters.
Results
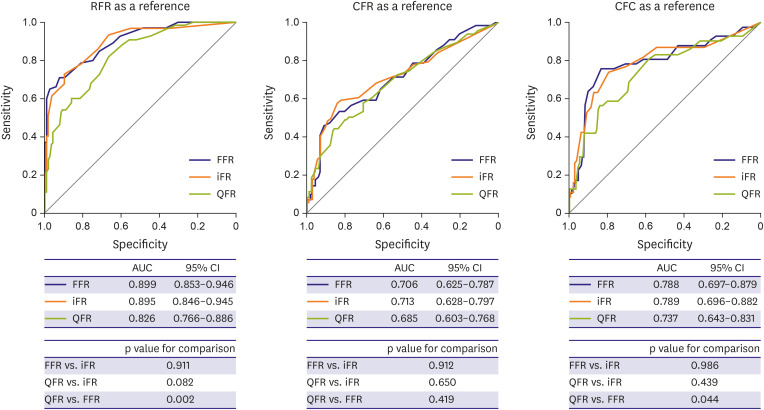
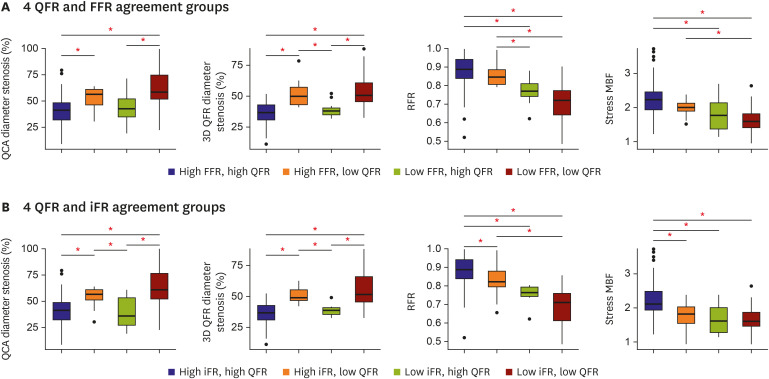
QFR, FFR, and iFR showed similar responses to both anatomic and hemodynamic stenosis severity. Regarding RFR, the diagnostic accuracy of QFR was lower than FFR (76.2% vs. 83.2%, p=0.021) and iFR (76.2% vs. 84.3%, p=0.031). For coronary flow capacity (CFC), QFR showed a lower accuracy than iFR (74.1% vs. 82%, p=0.031) and lower discriminant function than FFR (area under curve: 0.74 vs. 0.79, p=0.044). Discordance between QFR and FFR or iFR was shown in 14.6% of cases and was driven by the difference in %DS and heterogeneous distribution of PET-derived RFR and stress myocardial blood flow.
Conclusions
QFR demonstrated a similar response to different anatomic and hemodynamic stenosis severity as FFR or iFR. However, its diagnostic performance was inferior to FFR and iFR when PET-derived RFR and CFC were used as a reference.
Figure
Cited by 4 articles
-
Would a Noninvasive Coronary Physiology Become a Standard and Popular Approach?
Yun-Kyeong Cho, Chang-Wook Nam
Korean Circ J. 2021;51(2):140-142. doi: 10.4070/kcj.2020.0511.Differential Prognostic Implications of Pre- and Post-Stent Fractional Flow Reserve in Patients Undergoing Percutaneous Coronary Intervention
Jinlong Zhang, Doyeon Hwang, Seokhun Yang, Chee Hae Kim, Joo Myung Lee, Chang-Wook Nam, Eun-Seok Shin, Joon-Hyung Doh, Masahiro Hoshino, Rikuta Hamaya, Yoshihisa Kanaji, Tadashi Murai, Jun-Jie Zhang, Fei Ye, Xiaobo Li, Zhen Ge, Shao-Liang Chen, Tsunekazu Kakuta, Bon-Kwon Koo
Korean Circ J. 2021;52(1):47-59. doi: 10.4070/kcj.2021.0128.Differential Prognostic Implications of Pre- and Post-Stent Fractional Flow Reserve in Patients Undergoing Percutaneous Coronary Intervention
Jinlong Zhang, Doyeon Hwang, Seokhun Yang, Chee Hae Kim, Joo Myung Lee, Chang-Wook Nam, Eun-Seok Shin, Joon-Hyung Doh, Masahiro Hoshino, Rikuta Hamaya, Yoshihisa Kanaji, Tadashi Murai, Jun-Jie Zhang, Fei Ye, Xiaobo Li, Zhen Ge, Shao-Liang Chen, Tsunekazu Kakuta, Bon-Kwon Koo
Korean Circ J. 2021;52(1):47-59. doi: 10.4070/kcj.2021.0128.Practical Approach for Angina and Non-Obstructive Coronary Arteries: A State-of-the-Art Review
Coen K.M. Boerhout, Marcel A.M. Beijk, Peter Damman, Jan J. Piek, Tim P. van de Hoef
Korean Circ J. 2023;53(8):519-534. doi: 10.4070/kcj.2023.0109.
Reference
-
1. Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019; 40:87–165. PMID: 30165437.2. Dehmer GJ, Weaver D, Roe MT, et al. A contemporary view of diagnostic cardiac catheterization and percutaneous coronary intervention in the United States: a report from the CathPCI Registry of the National Cardiovascular Data Registry, 2010 through June 2011. J Am Coll Cardiol. 2012; 60:2017–2031. PMID: 23083784.3. Toth GG, Toth B, Johnson NP, et al. Revascularization decisions in patients with stable angina and intermediate lesions: results of the international survey on interventional strategy. Circ Cardiovasc Interv. 2014; 7:751–759. PMID: 25336468.4. Tu S, Barbato E, Köszegi Z, et al. Fractional flow reserve calculation from 3-dimensional quantitative coronary angiography and TIMI frame count: a fast computer model to quantify the functional significance of moderately obstructed coronary arteries. JACC Cardiovasc Interv. 2014; 7:768–777. PMID: 25060020.5. Tu S, Westra J, Yang J, et al. Diagnostic accuracy of fast computational approaches to derive fractional flow reserve from diagnostic coronary angiography: the international multicenter FAVOR pilot study. JACC Cardiovasc Interv. 2016; 9:2024–2035. PMID: 27712739.6. Xu B, Tu S, Qiao S, et al. Diagnostic accuracy of angiography-based quantitative flow ratio measurements for online assessment of coronary stenosis. J Am Coll Cardiol. 2017; 70:3077–3087. PMID: 29101020.7. Collet C, Onuma Y, Sonck J, et al. Diagnostic performance of angiography-derived fractional flow reserve: a systematic review and Bayesian meta-analysis. Eur Heart J. 2018; 39:3314–3321. PMID: 30137305.
Article8. Westra J, Andersen BK, Campo G, et al. Diagnostic performance of in-procedure angiography-derived quantitative flow reserve compared to pressure-derived fractional flow reserve: the FAVOR II Europe-Japan study. J Am Heart Assoc. 2018; 7:e009603. PMID: 29980523.
Article9. Westra J, Tu S, Winther S, et al. Evaluation of coronary artery stenosis by quantitative flow ratio during invasive coronary angiography: the WIFI II study (Wire-Free Functional Imaging II). Circ Cardiovasc Imaging. 2018; 11:e007107. PMID: 29555835.
Article10. Hwang D, Choi KH, Lee JM, et al. Diagnostic agreement of quantitative flow ratio with fractional flow reserve and instantaneous wave-free ratio. J Am Heart Assoc. 2019; 8:e011605. PMID: 30977410.
Article11. Emori H, Kubo T, Kameyama T, et al. Quantitative flow ratio and instantaneous wave-free ratio for the assessment of the functional severity of intermediate coronary artery stenosis. Coron Artery Dis. 2018; 29:611–617. PMID: 29965837.
Article12. Hwang D, Jeon KH, Lee JM, et al. Diagnostic performance of resting and hyperemic invasive physiological indices to define myocardial ischemia: validation with 13N-ammonia positron emission tomography. JACC Cardiovasc Interv. 2017; 10:751–760. PMID: 28365268.13. Lee JM, Hwang D, Park J, et al. Exploring coronary circulatory response to stenosis and its association with invasive physiologic indexes using absolute myocardial blood flow and coronary pressure. Circulation. 2017; 136:1798–1808. PMID: 28851731.
Article14. Lee JM, Kim CH, Koo BK, et al. Integrated myocardial perfusion imaging diagnostics improve detection of functionally significant coronary artery stenosis by 13N-ammonia positron emission tomography. Circ Cardiovasc Imaging. 2016; 9:e004768. PMID: 27609817.
Article15. Gould KL, Johnson NP, Bateman TM, et al. Anatomic versus physiologic assessment of coronary artery disease. Role of coronary flow reserve, fractional flow reserve, and positron emission tomography imaging in revascularization decision-making. J Am Coll Cardiol. 2013; 62:1639–1653. PMID: 23954338.16. Stuijfzand WJ, Uusitalo V, Kero T, et al. Relative flow reserve derived from quantitative perfusion imaging may not outperform stress myocardial blood flow for identification of hemodynamically significant coronary artery disease. Circ Cardiovasc Imaging. 2015; 8:e002400. PMID: 25596142.
Article17. Johnson NP, Gould KL. Integrating noninvasive absolute flow, coronary flow reserve, and ischemic thresholds into a comprehensive map of physiological severity. JACC Cardiovasc Imaging. 2012; 5:430–440. PMID: 22498334.
Article18. Hajjiri MM, Leavitt MB, Zheng H, Spooner AE, Fischman AJ, Gewirtz H. Comparison of positron emission tomography measurement of adenosine-stimulated absolute myocardial blood flow versus relative myocardial tracer content for physiological assessment of coronary artery stenosis severity and location. JACC Cardiovasc Imaging. 2009; 2:751–758. PMID: 19520347.
Article19. Sen S, Escaned J, Malik IS, et al. Development and validation of a new adenosine-independent index of stenosis severity from coronary wave-intensity analysis: results of the ADVISE (ADenosine Vasodilator Independent Stenosis Evaluation) study. J Am Coll Cardiol. 2012; 59:1392–1402. PMID: 22154731.20. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988; 44:837–845. PMID: 3203132.
Article21. Johnson NP, Koo BK. Coronary psychology: do you believe? JACC Cardiovasc Interv. 2018; 11:1492–1494. PMID: 30093054.22. Lee HS, Lee JM, Nam CW, et al. Consensus document for invasive coronary physiologic assessment in Asia-Pacific countries. Cardiol J. 2019; 26:215–225. PMID: 31225632.
Article23. Adjedj J, Xaplanteris P, Toth G, et al. Visual and quantitative assessment of coronary stenoses at angiography versus fractional flow reserve: the impact of risk factors. Circ Cardiovasc Imaging. 2017; 10:e006243. PMID: 28687539.
Article24. Toth G, Hamilos M, Pyxaras S, et al. Evolving concepts of angiogram: fractional flow reserve discordances in 4000 coronary stenoses. Eur Heart J. 2014; 35:2831–2838. PMID: 24644308.
Article25. Mejía-Rentería H, Lee JM, Lauri F, et al. Influence of microcirculatory dysfunction on angiography-based functional assessment of coronary stenoses. JACC Cardiovasc Interv. 2018; 11:741–753. PMID: 29673505.
Article26. Johnson NP, Kirkeeide RL, Gould KL. Is discordance of coronary flow reserve and fractional flow reserve due to methodology or clinically relevant coronary pathophysiology? JACC Cardiovasc Imaging. 2012; 5:193–202. PMID: 22340827.
Article27. Johnson NP, Kirkeeide RL, Gould KL. Coronary anatomy to predict physiology: fundamental limits. Circ Cardiovasc Imaging. 2013; 6:817–832. PMID: 24046379.28. Chu M, Dai N, Yang J, Westra J, Tu S. A systematic review of imaging anatomy in predicting functional significance of coronary stenoses determined by fractional flow reserve. Int J Cardiovasc Imaging. 2017; 33:975–990. PMID: 28265791.
Article29. Tahari AK, Lee A, Rajaram M, et al. Absolute myocardial flow quantification with 82Rb PET/CT: comparison of different software packages and methods. Eur J Nucl Med Mol Imaging. 2014; 41:126–135. PMID: 23982454.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Assessment of Myocardial Collateral Blood Flow with Contrast Echocardiography
- Coronary Slow Flow Phenomenon Leads to ST Elevation Myocardial Infarction
- Evaluation of Myocardial Ischemia Using Coronary Computed Tomography Angiography in Patients with Stable Angina
- Role of Pressure Wire in Coronary Artery Disease
- A Case of Myocardial Ischemia and Myocardial Injury Caused by Coronary Vasospasm Associated with Hyperthyroidism