Intest Res.
2021 Jan;19(1):45-52. 10.5217/ir.2019.00135.
Quality of life in inflammatory bowel diseases: it is not all about the bowel
- Affiliations
-
- 1Division of Gastroenterology, Hepatology, Infectious Diseases, Department of Internal Medicine I, University Hospital Tübingen, Tübingen, Germany
- 2Division of Psychosomatic Medicine and Psychotherapy, Department of Internal Medicine VI, University Hospital Tübingen, Tübingen, Germany
- KMID: 2512100
- DOI: http://doi.org/10.5217/ir.2019.00135
Abstract
- Background/Aims
The inflammatory bowel diseases (IBD), ulcerative colitis (UC), and Crohn’s disease (CD) are chronic diseases mostly affecting young patients. As they are diseases accompanying patients for their entire life, and the quality of life (QUOL) interacts with disease activity, improving QUOL should be one of the main goals of therapy. This study aims to identify factors contributing to good or impaired QUOL.
Methods
Questionnaires addressing health-related QUOL and other psychological and social features were positioned on our institutions’ webpage and on the webpage of the largest self-help group for IBD in Germany. Patients were subdivided according to their QUOL score with a cutoff of <60. We used the Short Inflammatory Bowel Disease Questionnaire, the Assessment of the Demand for Additional Psychological Treatment, and the Fear of Progression Questionnaire Short Form.
Results
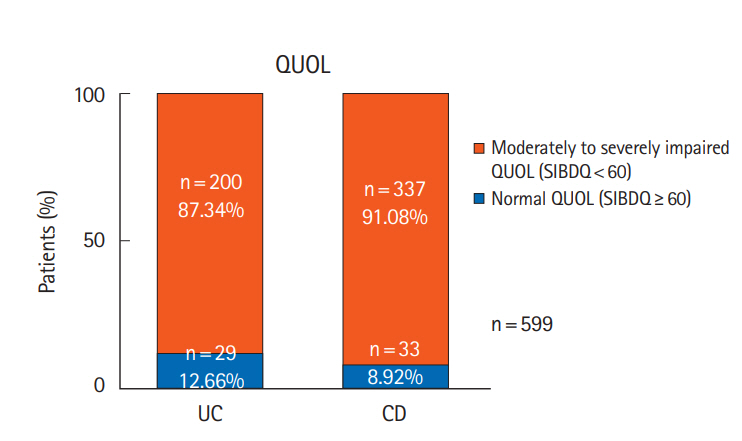
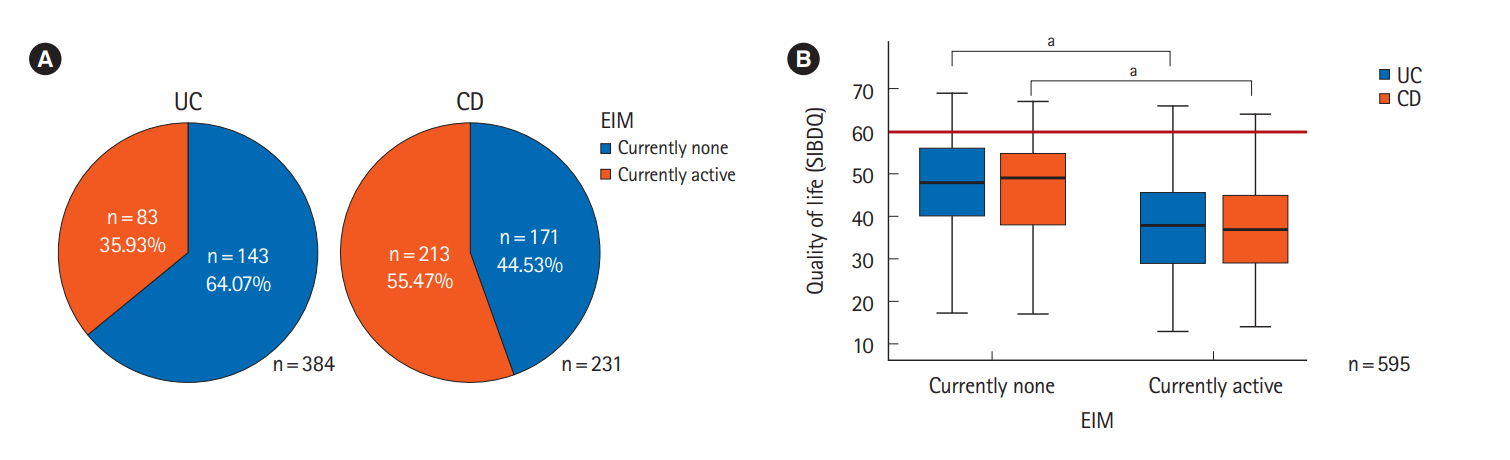
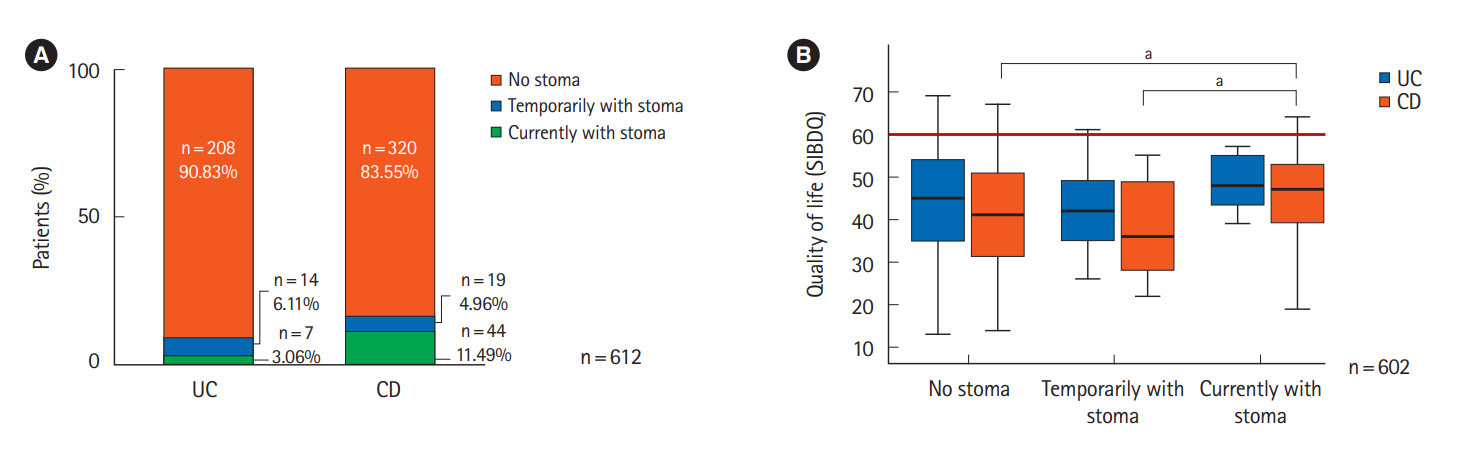
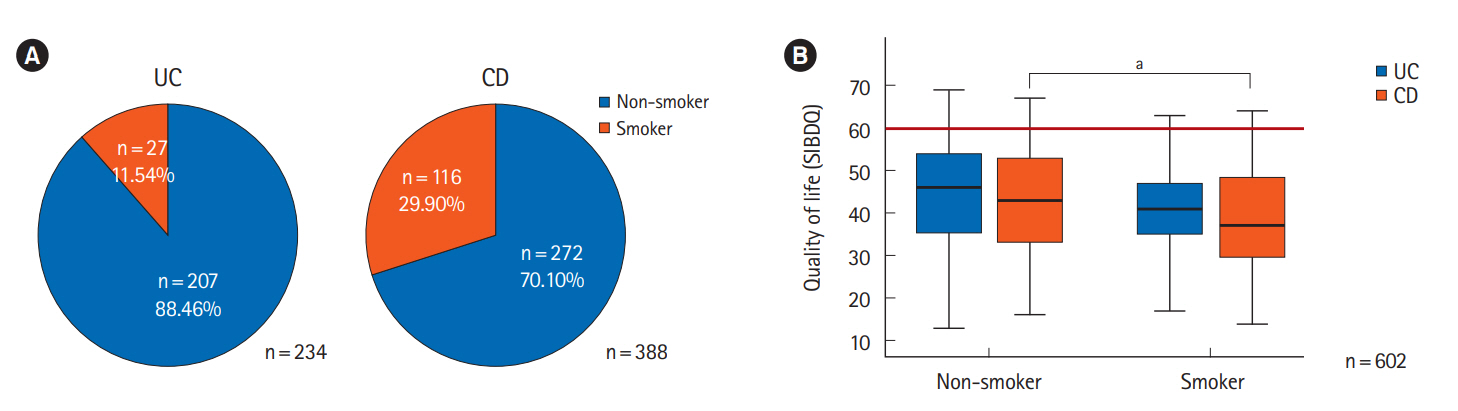
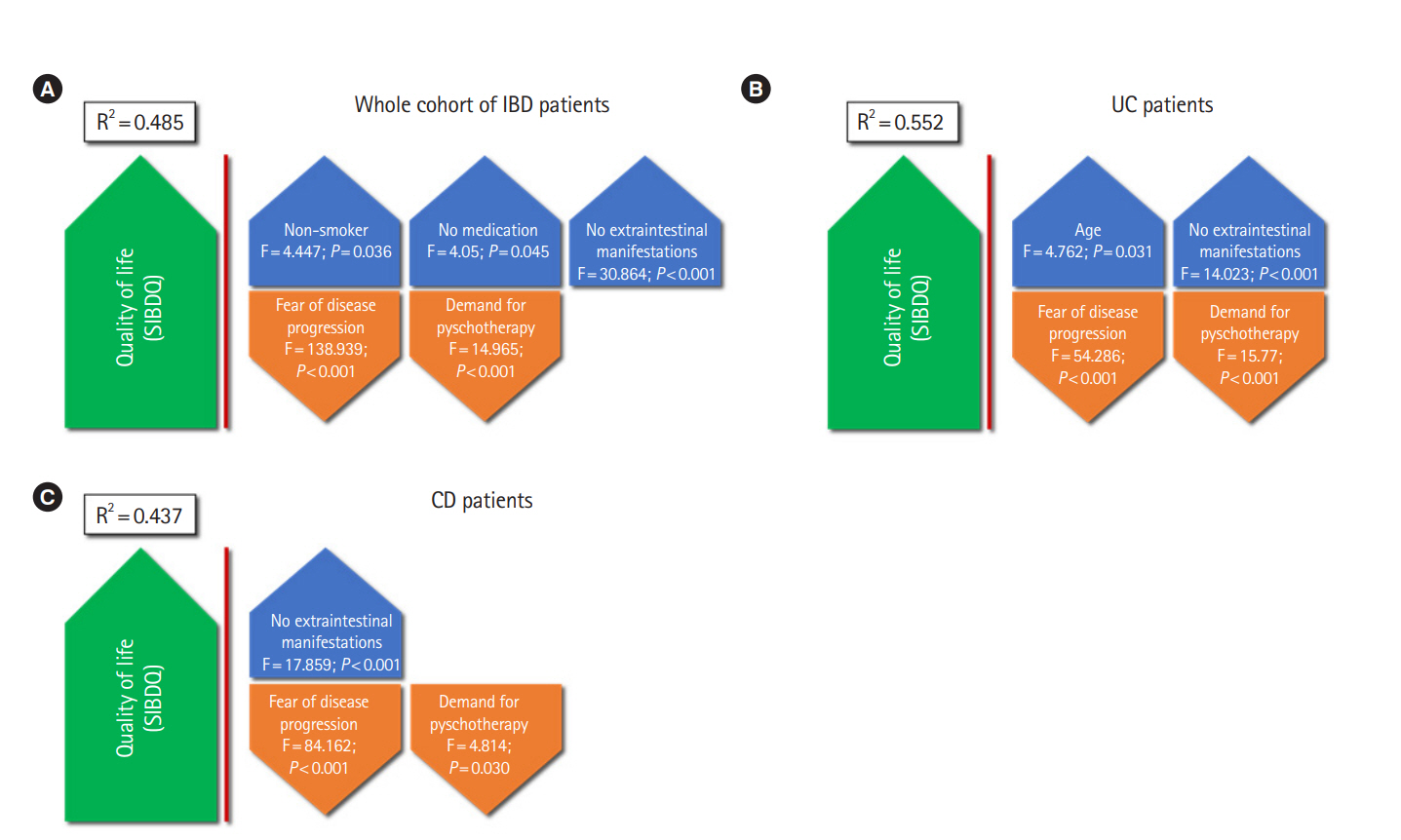
High numbers of patients in both subgroups showed an impaired QUOL (87.34% in UC, 91.08% in CD). Active extraintestinal manifestations, smoking, high fear of progression and high demand for psychotherapy were associated with reduced QUOL. In addition, polypharmacological interventions did not result in a good QUOL, but ostomies are linked to improved QUOL especially in CD patients.
Conclusions
Scores used in clinical day-to-day-practice mainly focusing on somatic factors do not sufficiently address important aspects concerning QUOL. Most importantly, extraintestinal manifestations show a hitherto underestimated impact on QUOL.
Figure
Cited by 2 articles
-
Correlation of fecal calprotectin and patient-reported outcome measures in patients with ulcerative colitis
Nagesh Kamat, Sudheer K Vuyyuru, Saurabh Kedia, Pabitra Sahu, Bhaskar Kante, Peeyush Kumar, Mukesh Kumar Ranjan, Mukesh Kumar Singh, Sambuddha Kumar, Vikas Sachdev, Govind Makharia, Vineet Ahuja
Intest Res. 2022;20(2):269-273. doi: 10.5217/ir.2021.00064.Corticosteroid, a double-edged sword in inflammatory bowel disease management: possibility of reducing corticosteroid use through physician education
Seulji Kim, Seong-Joon Koh
Intest Res. 2022;20(4):389-391. doi: 10.5217/ir.2022.00117.
Reference
-
1. Schreiber S, Hartmann H, Kruis W, et al. Inflammatory bowel disease competence network. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2016; 59:465–474.2. Wehkamp J, Götz M, Herrlinger K, Steurer W, Stange EF. Inflammatory bowel disease. Dtsch Arztebl Int. 2016; 113:72–82.3. Walsh AJ, Bryant RV, Travis SP. Current best practice for disease activity assessment in IBD. Nat Rev Gastroenterol Hepatol. 2016; 13:567–579.
Article4. Sandborn WJ, Feagan BG, Rutgeerts P, et al. Vedolizumab as induction and maintenance therapy for Crohn’s disease. N Engl J Med. 2013; 369:711–721.
Article5. Annese V. A review of extraintestinal manifestations and complications of inflammatory bowel disease. Saudi J Med Med Sci. 2019; 7:66–73.
Article6. Masaki T, Kishiki T, Kojima K, Asou N, Beniya A, Matsuoka H. Recent trends (2016-2017) in the treatment of inflammatory bowel disease. Ann Gastroenterol Surg. 2018; 2:282–288.
Article7. Parkes GC, Whelan K, Lindsay JO. Smoking in inflammatory bowel disease: impact on disease course and insights into the aetiology of its effect. J Crohns Colitis. 2014; 8:717–725.
Article8. Irvine EJ, Zhou Q, Thompson AK. The Short Inflammatory Bowel Disease Questionnaire: a quality of life instrument for community physicians managing inflammatory bowel disease. CCRPT Investigators. Canadian Crohn’s Relapse Prevention Trial. Am J Gastroenterol. 1996; 91:1571–1578.9. Jowett SL, Seal CJ, Barton JR, Welfare MR. The Short Inflammatory Bowel Disease Questionnaire is reliable and responsive to clinically important change in ulcerative colitis. Am J Gastroenterol. 2001; 96:2921–2928.
Article10. Han SW, Gregory W, Nylander D, et al. The SIBDQ: further validation in ulcerative colitis patients. Am J Gastroenterol. 2000; 95:145–151.
Article11. Guyatt G, Mitchell A, Irvine EJ, et al. A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterology. 1989; 96:804–810.
Article12. Rose M, Fliege H, Hildebrandt M, et al. Validation of the new German translation version of the “Short Inflammatory Bowel Disease Questionnaire” (SIBDQ). Z Gastroenterol. 2000; 38:277–286.
Article13. Williet N, Sarter H, Gower-Rousseau C, et al. Patient-reported outcomes in a French nationwide survey of inflammatory bowel disease patients. J Crohns Colitis. 2017; 11:165–174.
Article14. Miehsler W, Weichselberger M, Offerlbauer-Ernst A, et al. Assessing the demand for psychological care in chronic diseases: development and validation of a questionnaire based on the example of inflammatory bowel disease. Inflamm Bowel Dis. 2004; 10:637–645.15. Miehsler W, Weichselberger M, Offerlbauer-Ernst A, et al. Which patients with IBD need psychological interventions? A controlled study. Inflamm Bowel Dis. 2008; 14:1273–1280.
Article16. Miehsler W, Dejaco C, Moser G. Factor analysis of ADAPT questionnaire for assessment of subjective need for psychological interventions. Inflamm Bowel Dis. 2008; 14:142–143.
Article17. Staufer K, Scherzer TM, Miehsler W, et al. Self-reported need for psychotherapy predicts interferon-induced depression in hepatitis C: stratification for interferon-free treatment. Antivir Ther. 2015; 20:501–506.
Article18. Klag T, Mazurak N, Fantasia L, et al. High demand for psychotherapy in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2017; 23:1796–1802.
Article19. Mehnert A, Herschbach P, Berg P, Henrich G, Koch U. Fear of progression in breast cancer patients: validation of the short form of the Fear of Progression Questionnaire (FoP-Q-SF). Z Psychosom Med Psychother. 2006; 52:274–288.
Article20. Erim Y, Loquai C, Schultheis U, et al. Anxiety, posttraumatic stress, and fear of cancer progression in patients with melanoma in cancer aftercare. Onkologie. 2013; 36:540–544.
Article21. Knowles SR, Wilson J, Wilkinson A, et al. Psychological wellbeing and quality of life in Crohn’s disease patients with an ostomy: a preliminary investigation. J Wound Ostomy Continence Nurs. 2013; 40:623–629.
Article22. Abdalla MI, Sandler RS, Kappelman MD, et al. The impact of ostomy on quality of life and functional status of Crohn’s disease patients. Inflamm Bowel Dis. 2016; 22:2658–2664.
Article23. Dibley L, Czuber-Dochan W, Duncan J, et al. NO002 Decisionmaking about emergency and planned stoma surgery for IBD: a qualitative exploration of patient and clinician perspectives. J Crohns Colitis. 2017; 11(Suppl 1):S487–S488.
Article24. Cosnes J. Smoking, physical activity, nutrition and lifestyle: environmental factors and their impact on IBD. Dig Dis. 2010; 28:411–417.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Depressive Symptoms and Quality of Life in the Patients of Inflammatory Bowel Disease
- Clinical Implication of Sarcopenia in Patients with Inflammatory Bowel Disease
- Pharmacologic treatment for inflammatory bowel disease
- Anxiety, Depression, and Quality of Life in Parents of Adolescents with Inflammatory Bowel Disease: A Longitudinal Study
- Musculoskeletal Manifestation in Inflammatory Bowel Disease