Restor Dent Endod.
2020 Nov;45(4):e55. 10.5395/rde.2020.45.e55.
Assessment of the radiant emittance of damaged/contaminated dental lightcuring tips by spectrophotometric methods
- Affiliations
-
- 1Dental Biomedical Sciences PhD Program, University of Maryland School of Dentistry, Baltimore, MD, USA
- 2Department of Restorative Dental Sciences, Imam Abdulrahman Bin Faisal University, College of Dentistry, Dammam, Saudi Arabia
- 3Dental Materials Laboratory, School of Dentistry, Federal University of Rio Grande do Sul, Porto Alegre, RS, Brazil
- 4BlueLight Analytics Company, Halifax, NS, Canada
- 5Department of Dental Clinical Sciences, Dalhousie University, Halifax, NS, Canada
- 6Division of Operative Dentistry, Department of General Dentistry, University of Maryland School of Dentistry, Baltimore, MD, USA
- KMID: 2512046
- DOI: http://doi.org/10.5395/rde.2020.45.e55
Abstract
Objectives
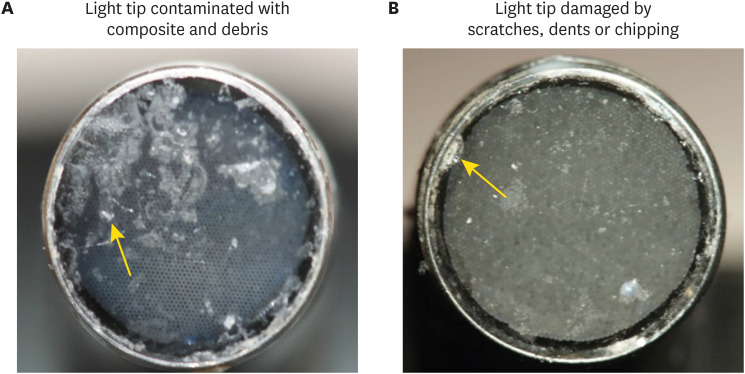
This study investigated the effects of physically damaged and resin-contaminated tips on radiant emittance, comparing them with new undamaged, non-contaminated tips using 3 pieces of spectrophotometric laboratory equipment.
Materials and Methods
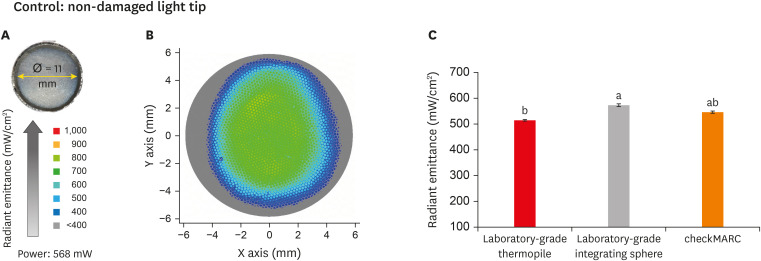
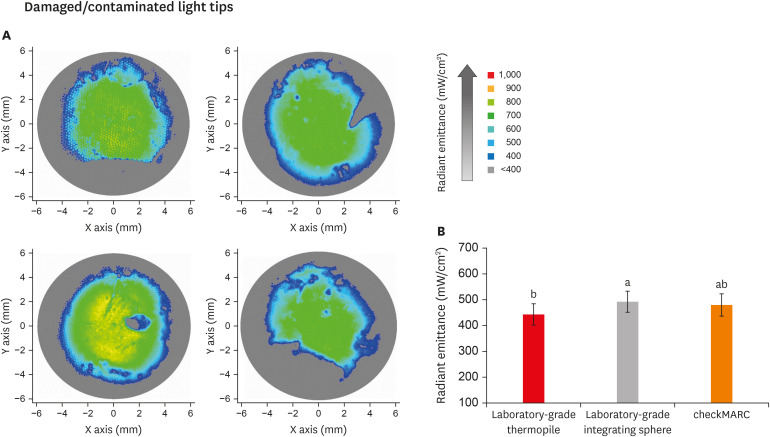
Nine tips with damage and/or resin contaminants from actual clinical situations were compared with a new tip without damage or contamination (control group). The radiant emittance was recorded using 3 spectrophotometric methods: a laboratory-grade thermopile, a laboratory-grade integrating sphere, and a portable light collector (checkMARC).
Results
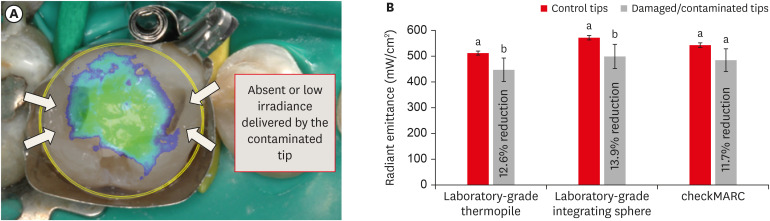
A significant difference between the laboratory-grade thermopile and the laboratory-grade integrating sphere was found when the radiant emittance values of the control or damaged/contaminated tips were investigated (p < 0.05), but both methods were comparable to checkMARC (p > 0.05). Regardless of the method used to quantify the light output, the mean radiant emittance values of the damaged/contaminated tips were significantly lower than those of the control (p < 0.05). The beam profile of the damaged/ contaminated tips was less homogeneous than that of the control.
Conclusions
Damaged/contaminated tips can reduce the radiant emittance output and the homogeneity of the beam, which may affect the energy delivered to composite restorations. The checkMARC spectrophotometer device can be used in dental offices, as it provided values close to those produced by a laboratory-grade integrated sphere spectrophotometer. Dentists should assess the radiant emittance of their light-curing units to ensure optimal curing in photoactivated, resin-based materials.
Keyword
Figure
Reference
-
1. Chan KHS, Mai Y, Kim H, Tong KCT, Ng D, Hsiao JCM. Review: resin composite filling. Materials (Basel). 2010; 3:1228–1243.
Article2. Balhaddad AA, Kansara AA, Hidan D, Weir MD, Xu HHK, Melo MAS. Toward dental caries: exploring nanoparticle-based platforms and calcium phosphate compounds for dental restorative materials. Bioact Mater. 2018; 4:43–55. PMID: 30582079.
Article3. World Health Organization. Oral health surveys: basic methods. 3rd ed. Geneva: World Health Organization;1987.4. Gordan VV, Riley JL 3rd, Rindal DB, Qvist V, Fellows JL, Dilbone DA, Brotman SG, Gilbert GH. National Dental Practice-Based Research Network Collaborative Group. Repair or replacement of restorations: a prospective cohort study by dentists in the National Dental Practice-Based Research Network. J Am Dent Assoc. 2015; 146:895–903. PMID: 26610834.5. David JR, Gomes OM, Gomes JC, Loguercio AD, Reis A. Effect of exposure time on curing efficiency of polymerizing units equipped with light-emitting diodes. J Oral Sci. 2007; 49:19–24. PMID: 17429178.
Article6. Santini A, Gallegos IT, Felix CM. Photoinitiators in dentistry: a review. Prim Dent J. 2013; 2:30–33.
Article7. Samaha S, Bhatt S, Finkelman M, Papathanasiou A, Perry R, Strassler H, Kugel G, Garcia-Godoy F, Price R. Effect of instruction, light curing unit, and location in the mouth on the energy delivered to simulated restorations. Am J Dent. 2017; 30:343–349. PMID: 29251458.8. Price RB, Ferracane JL, Shortall AC. Light-curing units: a review of what we need to know. J Dent Res. 2015; 94:1179–1186. PMID: 26156516.9. Maktabi H, Balhaddad AA, Alkhubaizi Q, Strassler H, Melo MAS. Factors influencing success of radiant exposure in light-curing posterior dental composite in the clinical setting. Am J Dent. 2018; 31:320–328. PMID: 30658380.10. AlShaafi MM. Factors affecting polymerization of resin-based composites: a literature review. Saudi Dent J. 2017; 29:48–58. PMID: 28490843.
Article11. Rueggeberg FA, Giannini M, Arrais CAG, Price RBT. Light curing in dentistry and clinical implications: a literature review. Braz Oral Res. 2017; 31:e61. PMID: 28902241.
Article12. Maktabi H, Ibrahim M, Alkhubaizi Q, Weir M, Xu H, Strassler H, Fugolin APP, Pfeifer CS, Melo MAS. Underperforming light curing procedures trigger detrimental irradiance-dependent biofilm response on incrementally placed dental composites. J Dent. 2019; 88:103110. PMID: 31022421.
Article13. Alshaafi MM. Evaluation of light-curing units in rural and urban areas. Saudi Dent J. 2012; 24:163–167. PMID: 23960546.
Article14. Price RBT, Ehrnford L, Andreou P, Felix CA. Comparison of quartz-tungsten-halogen, light-emitting diode, and plasma arc curing lights. J Adhes Dent. 2003; 5:193–207. PMID: 14621241.15. Vandenbulcke JDE, Marks LAM, Martens LC, Verbeeck RMH. Comparison of curing depth of a colored polyacid-modified composite resin with different light-curing units. Quintessence Int. 2010; 41:787–794. PMID: 20806104.16. Maghaireh GA, Alzraikat H, Taha NA. Assessing the irradiance delivered from light-curing units in private dental offices in Jordan. J Am Dent Assoc. 2013; 144:922–927. PMID: 23904579.
Article17. Barghi N, Fischer DE, Pham T. Revisiting the intensity output of curing lights in private dental offices. Compend Contin Educ Dent. 2007; 28:380–384. PMID: 17687900.18. Santos GC Jr, Santos MJMC, El-Mowafy O, El-Badrawy W. Intensity of quartz-tungsten-halogen light polymerization units used in dental offices in Brazil. Int J Prosthodont. 2005; 18:434–435. PMID: 16220811.19. Nassar HM, Ajaj R, Hasanain F. Efficiency of light curing units in a government dental school. J Oral Sci. 2018; 60:142–146. PMID: 29576574.
Article20. Al Shaafi M, Maawadh A, Al Qahtani M. Evaluation of light intensity output of QTH and LED curing devices in various governmental health institutions. Oper Dent. 2011; 36:356–361. PMID: 21834709.
Article21. El-Mowafy O, El-Badrawy W, Lewis DW, Shokati B, Kermalli J, Soliman O, Encioiu A, Zawi R, Rajwani F, Rajwani F. Intensity of quartz-tungsten-halogen light-curing units used in private practice in Toronto. J Am Dent Assoc. 2005; 136:766–773. PMID: 16022041.
Article22. Jandt KD, Mills RW, Blackwell GB, Ashworth SH. Depth of cure and compressive strength of dental composites cured with blue light emitting diodes (LEDs). Dent Mater. 2000; 16:41–47. PMID: 11203522.
Article23. Shortall AC, Price RB, MacKenzie L, Burke FJT. Guidelines for the selection, use, and maintenance of LED light-curing units - part II. Br Dent J. 2016; 221:551–554. PMID: 27811902.
Article24. International Organization for Standardization. ISO 10650-2. Dentistry—powered polymerization activators—part 2: light-emitting diode (LED) lamps. Geneva: International Organization for Standardization;2007.25. Shortall AC, Felix CJ, Watts DC. Robust spectrometer-based methods for characterizing radiant exitance of dental LED light curing units. Dent Mater. 2015; 31:339–350. PMID: 25773187.
Article26. Marović D, Matić S, Kelić K, Klarić E, Rakić M, Tarle Z. Time dependent accuracy of dental radiometers. Acta Clin Croat. 2013; 52:173–180. PMID: 24053077.27. Kameyama A, Haruyama A, Asami M, Takahashi T. Effect of emitted wavelength and light guide type on irradiance discrepancies in hand-held dental curing radiometers. ScientificWorldJournal. 2013; 2013:647941. PMID: 24222744.
Article28. Price RB, Labrie D, Kazmi S, Fahey J, Felix CM. Intra- and inter-brand accuracy of four dental radiometers. Clin Oral Investig. 2012; 16:707–717.
Article29. Michaud PL, Price RBT, Labrie D, Rueggeberg FA, Sullivan B. Localised irradiance distribution found in dental light curing units. J Dent. 2014; 42:129–139. PMID: 24287255.
Article30. Harlow JE, Sullivan B, Shortall AC, Labrie D, Price RB. Characterizing the output settings of dental curing lights. J Dent. 2016; 44:20–26. PMID: 26546716.
Article31. Shimokawa CAK, Harlow JE, Turbino ML, Price RB. Ability of four dental radiometers to measure the light output from nine curing lights. J Dent. 2016; 54:48–55. PMID: 27597433.
Article32. Konerding KL, Heyder M, Kranz S, Guellmar A, Voelpel A, Watts DC, Jandt KD, Sigusch BW. Study of energy transfer by different light curing units into a class III restoration as a function of tilt angle and distance, using a MARC patient simulator (PS). Dent Mater. 2016; 32:676–686. PMID: 27017156.
Article33. Soares CJ, Rodrigues MP, Oliveira LRS, Braga SSL, Barcelos LM, Silva GR, Giannini M, Price RB. An evaluation of the light output from 22 contemporary light curing units. Braz Dent J. 2017; 28:362–371. PMID: 29297558.
Article34. Price RBT, Labrie D, Rueggeberg FA, Felix CM. Irradiance differences in the violet (405 nm) and blue (460 nm) spectral ranges among dental light-curing units. J Esthet Restor Dent. 2010; 22:363–377. PMID: 21126292.
Article35. Price RBT, Rueggeberg FA, Labrie D, Felix CM. Irradiance uniformity and distribution from dental light curing units. J Esthet Restor Dent. 2010; 22:86–101. PMID: 20433559.
Article36. Rueggeberg FA, Caughman WF, Curtis JW Jr. Effect of light intensity and exposure duration on cure of resin composite. Oper Dent. 1994; 19:26–32. PMID: 8183730.37. Al-Zain AO, Eckert GJ, Lukic H, Megremis S, Platt JA. Polymerization pattern characterization within a resin-based composite cured using different curing units at two distances. Clin Oral Investig. 2019; 23:3995–4010.
Article38. Eshmawi YT, Al-Zain AO, Eckert GJ, Platt JA. Variation in composite degree of conversion and microflexural strength for different curing lights and surface locations. J Am Dent Assoc. 2018; 149:893–902. PMID: 30149887.
Article39. Yeh CL, Miyagawa Y, Powers JM. Optical properties of composites of selected shades. J Dent Res. 1982; 61:797–801. PMID: 6953116.
Article40. International Organization for Standardization. ISO 10650-1. Dentistry—powered polymerization activators—part 1: quartz tungsten halogen lamps. Geneva: International Organization for Standardization;2004.41. Arikawa H, Kanie T, Fujii K, Takahashi H, Ban S. Effect of inhomogeneity of light from light curing units on the surface hardness of composite resin. Dent Mater J. 2008; 27:21–28. PMID: 18309608.
Article42. Rueggeberg FA. State-of-the-art: dental photocuring--a review. Dent Mater. 2011; 27:39–52. PMID: 21122903.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Shade comparative analysis of natural tooth measured by visual and spectrophotometric methods
- Comparison of instrumental methods for color change assessment of Giomer resins
- Electron Microscopy of Needle Tips Following Intravitreal Injections Using 30-Gauge Needles
- The efficacy of different implant surface decontamination methods using spectrophotometric analysis: an in vitro study
- The Effectiveness Of Decontamination Methods In Dental Instruments