Obstet Gynecol Sci.
2020 Nov;63(6):726-734. 10.5468/ogs.20145.
Clinical experience of robotic myomectomy for fertility preservation using preoperative magnetic resonance imaging predictor
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Ewha Womans University Seoul Hospital, College of Medicine, Ewha Womans University, Seoul, Korea
- 2Department of Obstetrics and Gynecology, Ewha Womans University Mokdong Hospital, College of Medicine, Ewha Womans University, Seoul, Korea
- 3Department of Radiology, Konkuk University Medical Center, Research Institute of Medical Science, Konkuk University School of Medicine, Seoul, Korea
- KMID: 2511213
- DOI: http://doi.org/10.5468/ogs.20145
Abstract
Objective
This study aimed to demonstrate the use of preoperative magnetic resonance imaging (MRI) findings to select the optimal surgical technique between single-site (SS) and multi-site (MS) robotic myomectomy based on clinical experience, for the preservation of fertility.
Methods
Ninety-eight patients who underwent SS or MS robotic myomectomy using the da Vinci® Si system after undergoing MRI were evaluated retrospectively. The correlation between preoperative MRI findings and the intraoperative or postoperative findings during robotic myomectomy for the preservation of fertility was analyzed. The reproductive outcome was investigated when the patient wished to conceive.
Results
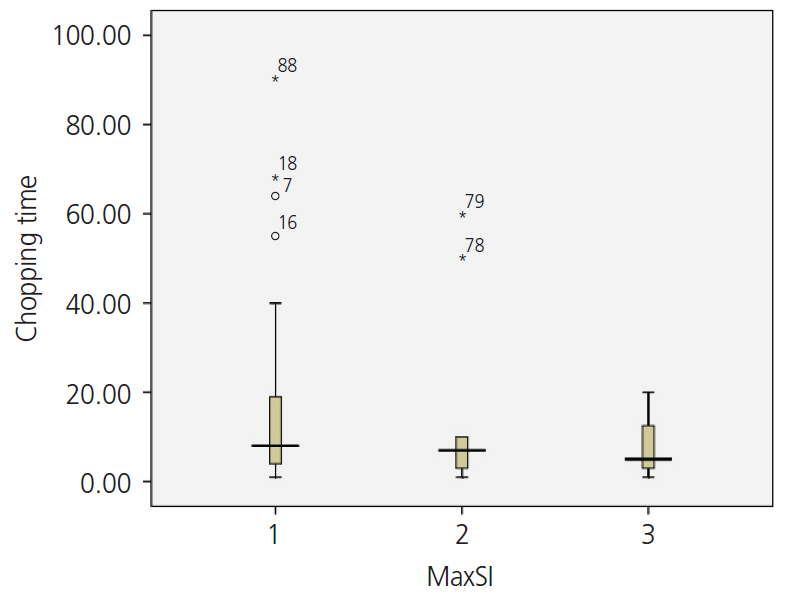
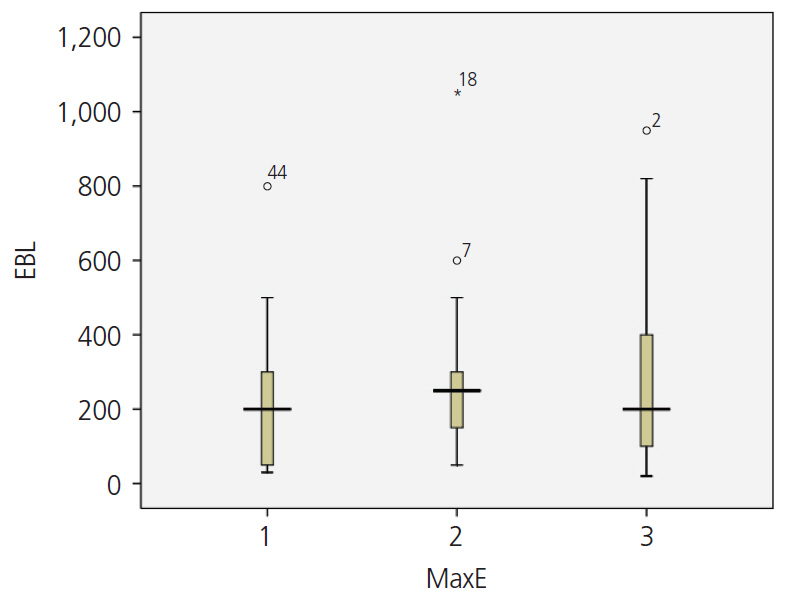
The mean age of the patients was 35.68±5.04 years and 80 patients (81.6%) were nulliparous. The total diameter of myomas on MRI was 106.75±54.52 mm. The number of resected myomas was 4.31±4.39 (range, 1–27), and the total weight of resected myomas was 293.11±281.13 (range, 30–1,260) g. Myomas with high signal intensity on MRI required less time for resection. MS robotic myomectomy was performed for an increased number and total diameter of a myoma or a deep-seated myoma. Postoperatively, all patients resumed normal menstruation. Of the 15 patients who wished to conceive, 12 (80%) conceived successfully. Of these, uterine dehiscence occurred in 1 patient and 10 patients underwent an uneventful cesarean section.
Conclusion
SS or MS robotic myomectomy can be recommended for patients who wish to conserve fertility. However, the optimal surgical technique should be selected based on preoperative MRI findings to predict an effective surgical process and the successful preservation of fertility.
Figure
Reference
-
References
1. Stewart EA. Uterine fibroids. Lancet. 2001; 357:293–8.
Article2. Karlsen K, Mogensen O, Humaidana P, Kesmodel US, Ravn P. Uterine fibroids increase time to pregnancy: a cohort study. Eur J Contracept Reprod Health Care. 2020; 25:37–42.
Article3. Kim H, Shim S, Hwang Y, Kim M, Hwang H, Chung Y, et al. Is robot-assisted laparoscopic myomectomy limited in multiple myomas?: a feasibility for ten or more myomas. Obstet Gynecol Sci. 2018; 61:135–41.
Article4. Kim M, Kim MK, Kim ML, Jung YW, Yun BS, Seong SJ. Robotic single-site myomectomy: a single-center experience of 101 consecutive cases. Int J Med Robot. 2019; 15:e1959.
Article5. Dueholm M, Lundorf E, Hansen ES, Ledertoug S, Olesen F. Accuracy of magnetic resonance imaging and transvaginal ultrasonography in the diagnosis, mapping, and measurement of uterine myomas. Am J Obstet Gynecol. 2002; 186:409–15.
Article6. Jondal DE, Wang J, Chen J, Gorny KR, Felmlee J, Hesly G, et al. Uterine fibroids: correlations between MRI appearance and stiffness via magnetic resonance elastography. Abdom Radiol (NY). 2018; 43:1456–63.
Article7. Wang T, Tang H, Xie Z, Deng S. Robotic-assisted vs. laparoscopic and abdominal myomectomy for treatment of uterine fibroids: a meta-analysis. Minim Invasive Ther Allied Technol. 2018; 27:249–64.
Article8. Huberlant S, Lenot J, Neron M, Ranisavljevic N, Letouzey V, De Tayrac R, et al. Fertility and obstetrical outcomes after robot-assisted laparoscopic myomectomy. Int J Med Robot. 2020; 16:e2059.
Article9. Pitter MC, Srouji SS, Gargiulo AR, Kardos L, Seshadri-Kreaden U, Hubert HB, et al. Fertility and symptom relief following robot-assisted laparoscopic myomectomy. Obstet Gynecol Int. 2015; 2015:967568.
Article10. Pitter MC, Gargiulo AR, Bonaventura LM, Lehman JS, Srouji SS. Pregnancy outcomes following robot-assisted myomectomy. Hum Reprod. 2013; 28:99–108.
Article11. Choi SH, Hong S, Kim M, Bae HS, Kim MK, Kim ML, et al. Robotic-assisted laparoscopic myomectomy: the feasibility in single-site system. Obstet Gynecol Sci. 2019; 62:56–64.
Article12. Lewis EI, Srouji SS, Gargiulo AR. Robotic single-site myomectomy: initial report and technique. Fertil Steril. 2015; 103:1370–1377. e1.
Article13. Nam SH, Paek J, Choi C, Nam SH, Kim WY. A comparison between reduced-port robotic surgery and multiport robot-assisted laparoscopy for myomectomy. Eur J Obstet Gynecol Reprod Biol. 2017; 213:53–7.
Article14. Moawad GN, Tyan P, Paek J, Tappy EE, Park D, Choussein S, et al. Comparison between single-site and multiport robot-assisted myomectomy. J Robot Surg. 2019; 13:757–64.
Article15. Goebel K, Goldberg JM. Women’s preference of cosmetic results after gynecologic surgery. J Minim Invasive Gynecol. 2014; 21:64–7.
Article16. Yeung PP Jr, Bolden CR, Westreich D, Sobolewski C. Patient preferences of cosmesis for abdominal incisions in gynecologic surgery. J Minim Invasive Gynecol. 2013; 20:79–84.
Article17. Choi EJ, Rho AM, Lee SR, Jeong K, Moon HS. Robotic single-site myomectomy: clinical analysis of 61 consecutive cases. J Minim Invasive Gynecol. 2017; 24:632–9.
Article18. Moon HS, Shim JE, Lee SR, Jeong K. The comparison of robotic single-site surgery to single-port laparoendoscopic surgery for the treatment of advanced-stage endometriosis. J Laparoendosc Adv Surg Tech A. 2018; 28:1483–8.
Article19. Maciel C, Tang YZ, Sahdev A, Madureira AM, Vilares Morgado P. Preprocedural MRI and MRA in planning fibroid embolization. Diagn Interv Radiol. 2017; 23:163–71.
Article20. Park H, Yoon SW, Sokolov A. Scaled signal intensity of uterine fibroids based on T2-weighted MR images: a potential objective method to determine the suitability for magnetic resonance-guided focused ultrasound surgery of uterine fibroids. Eur Radiol. 2015; 25:3455–8.
Article21. Lénárd ZM, McDannold NJ, Fennessy FM, Stewart EA, Jolesz FA, Hynynen K, et al. Uterine leiomyomas: MR imaging-guided focused ultrasound surgery--imaging predictors of success. Radiology. 2008; 249:187–94.
Article22. Sutton C, Standen P, Acton J, Griffin C. Spontaneous uterine rupture in a preterm pregnancy following myomectomy. Case Rep Obstet Gynecol. 2016; 2016:6195621.
Article23. Bernardi TS, Radosa MP, Weisheit A, Diebolder H, Schneider U, Schleussner E, et al. Laparoscopic myomectomy: a 6-year follow-up single-center cohort analysis of fertility and obstetric outcome measures. Arch Gynecol Obstet. 2014; 290:87–91.
Article24. Buckley VA, Nesbitt-Hawes EM, Atkinson P, Won HR, Deans R, Burton A, et al. Laparoscopic myomectomy: clinical outcomes and comparative evidence. J Minim Invasive Gynecol. 2015; 22:11–25.
Article25. Flyckt RL, Falcone T. Uterine rupture after laparoscopic myomectomy. J Minim Invasive Gynecol. 2015; 22:921–2.
Article26. Kim HS, Oh SY, Choi SJ, Park HS, Cho GJ, Chung JH, et al. Uterine rupture in pregnancies following myomectomy: a multicenter case series. Obstet Gynecol Sci. 2016; 59:454–62.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Fast 3-Dimensional Magnetic Resonance Imaging Reconstruction for Surgical Planning of Uterine Myomectomy
- Robot-Assisted Laparoscopic Adenomyomectomy for Patients Who Want to Preserve Fertility
- Lack of Haptic Feedback Is Replaced by More Developed Visual Sense during Robotic Myomectomy
- Robot-assisted surgery in gynecology: indications and efficacy
- Uterocutaneous fistula after pelviscopic myomectomy - successful diagnosis with hystero-salpingo contrast sonography and complete tract resection and medical treatment for fertility preservation in young woman: a case report