Endocrinol Metab.
2020 Dec;35(4):774-783. 10.3803/EnM.2020.404.
Minimally Invasive Adrenal Surgery
- Affiliations
-
- 1Department of Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 2Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2511004
- DOI: http://doi.org/10.3803/EnM.2020.404
Abstract
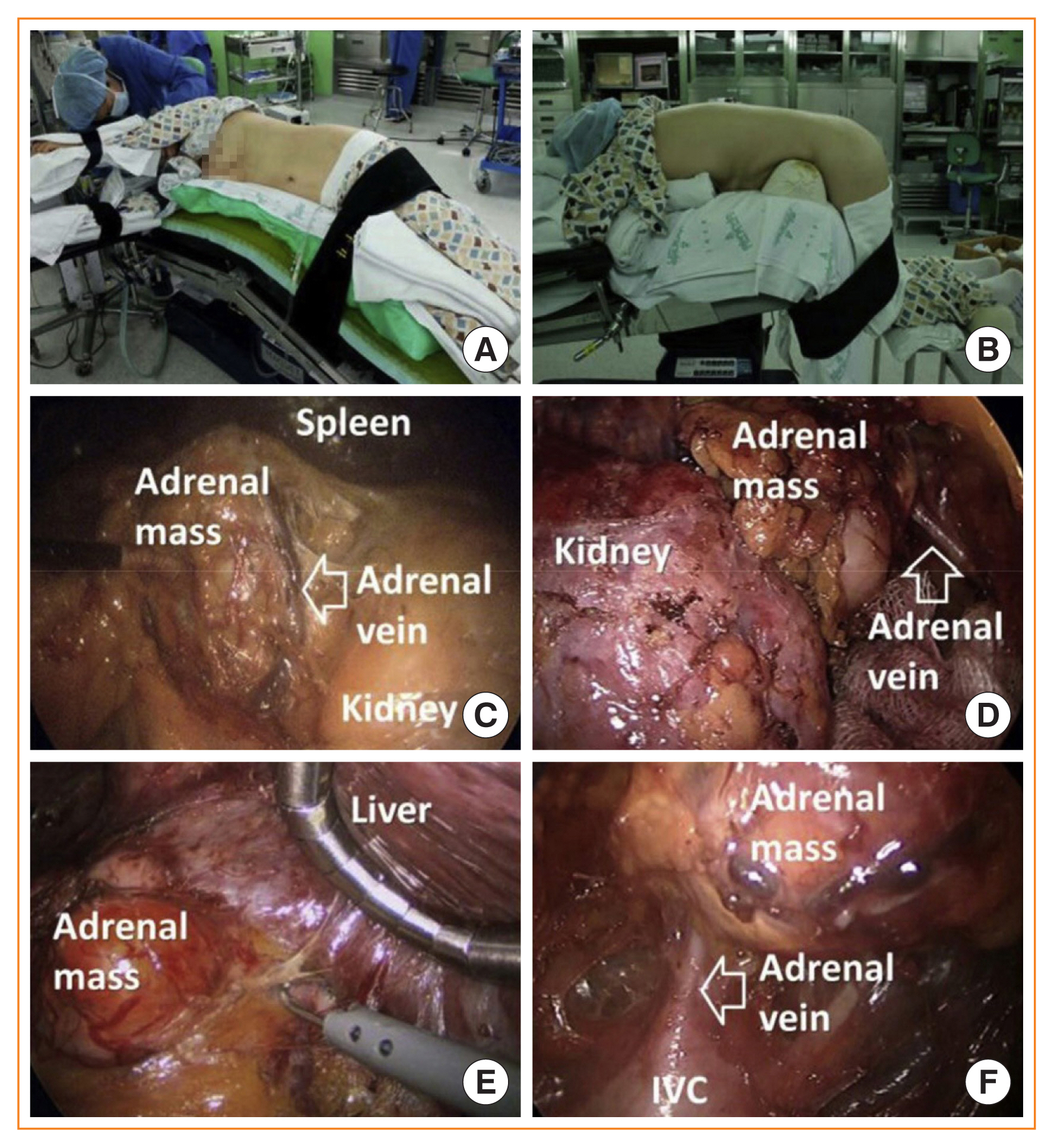
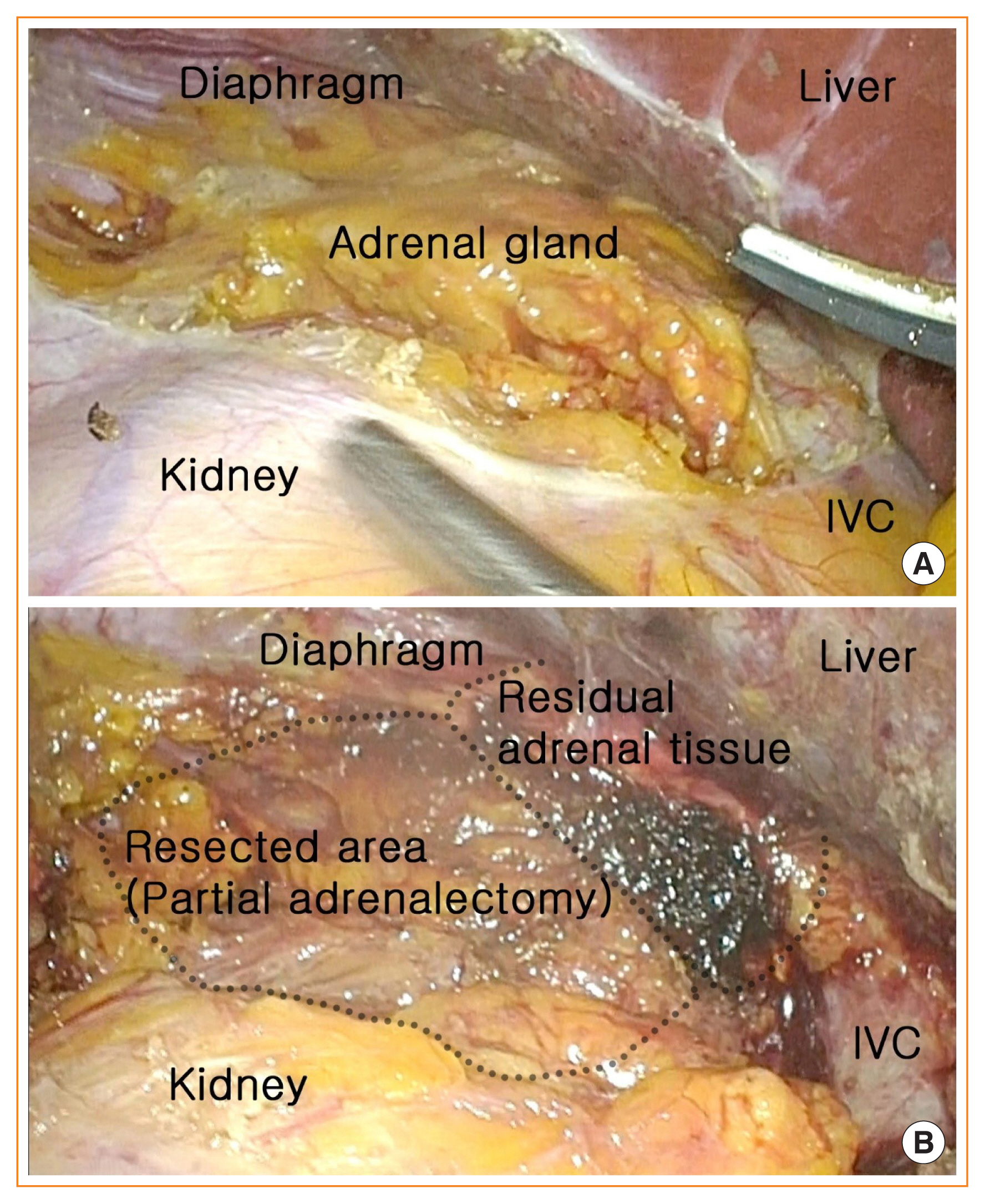
- Since the introduction of minimally invasive surgery, laparoscopic adrenalectomy has become the main treatment option for adrenal masses. Various studies have reported that laparoscopic adrenalectomy showed fewer postoperative complications and faster recovery than conventional open adrenalectomy. Laparoscopic adrenalectomy can be performed through either the transperitoneal approach or the retroperitoneoscopic approach, which are widely used in most adrenal surgical procedures. Furthermore, with the development of minimally invasive surgery, organ-sparing adrenalectomy has recently emerged as a way to conserve functional adrenal gland tissue. According to recent data, organ-sparing adrenalectomy shows promising surgical, functional, and oncological outcomes including less intraoperative blood loss, maintenance of adrenal function, and low recurrence. Partial adrenalectomy was initially proposed for bilateral adrenal tumors in patients with hereditary disease to avoid chronic adrenal insufficiency. However, it has also gained popularity for the treatment of unilateral adrenal disease involving a small adrenal tumor because even patients with a unilateral adrenal gland may develop adrenal insufficiency in stressful situations. Therefore, partial adrenalectomy has become increasingly common to avoid lifelong steroid replacement and recurrence in most cases, especially in bilateral adrenal disease. This review article evaluates the current evidence on minimally invasive adrenalectomy and organ-preserving partial adrenalectomy.
Figure
Reference
-
1. Gagner M, Lacroix A, Bolte E. Laparoscopic adrenalectomy in Cushing’s syndrome and pheochromocytoma. N Engl J Med. 1992; 327:1033.
Article2. Higashihara E, Tanaka Y, Horie S, Aruga S, Nutahara K, Homma Y, et al. A case report of laparoscopic adrenalectomy. Nihon Hinyokika Gakkai Zasshi. 1992; 83:1130–3.
Article3. Mercan S, Seven R, Ozarmagan S, Tezelman S. Endoscopic retroperitoneal adrenalectomy. Surgery. 1995; 118:1071–5.
Article4. Piazza L, Caragliano P, Scardilli M, Sgroi AV, Marino G, Giannone G. Laparoscopic robot-assisted right adrenalectomy and left ovariectomy (case reports). Chir Ital. 1999; 51:465–6.5. Chai YJ, Kwon H, Yu HW, Kim SJ, Choi JY, Lee KE, et al. Systematic review of surgical approaches for adrenal tumors: lateral transperitoneal versus posterior retroperitoneal and laparoscopic versus robotic adrenalectomy. Int J Endocrinol. 2014; 2014:918346.
Article6. Cooper AB, Habra MA, Grubbs EG, Bednarski BK, Ying AK, Perrier ND, et al. Does laparoscopic adrenalectomy jeopardize oncologic outcomes for patients with adrenocortical carcinoma? Surg Endosc. 2013; 27:4026–32.
Article7. Nagaraja V, Eslick GD, Edirimanne S. Recurrence and functional outcomes of partial adrenalectomy: a systematic review and meta-analysis. Int J Surg. 2015; 16(Pt A):7–13.
Article8. Ikeda Y, Takami H. Adrenal overview. Biomed Pharmacother. 2002; 56(Suppl 1):104s–6s.9. McKinlay R, Mastrangelo MJ Jr, Park AE. Laparoscopic adrenalectomy: indications and technique. Curr Surg. 2003; 60:145–9.
Article10. Constantinides VA, Christakis I, Touska P, Palazzo FF. Systematic review and meta-analysis of retroperitoneoscopic versus laparoscopic adrenalectomy. Br J Surg. 2012; 99:1639–48.11. Lairmore TC, Folek J, Govednik CM, Snyder SK. Improving minimally invasive adrenalectomy: selection of optimal approach and comparison of outcomes. World J Surg. 2016; 40:1625–31.
Article12. Chai YJ, Woo JW, Kwon H, Choi JY, Kim SJ, Lee KE. Comparative outcomes of lateral transperitoneal adrenalectomy versus posterior retroperitoneoscopic adrenalectomy in consecutive patients: a single surgeon’s experience. Asian J Surg. 2016; 39:74–80.
Article13. Bittner JG 4th, Gershuni VM, Matthews BD, Moley JF, Brunt LM. Risk factors affecting operative approach, conversion, and morbidity for adrenalectomy: a single-institution series of 402 patients. Surg Endosc. 2013; 27:2342–50.
Article14. Sautter AE, Cunningham SC, Kowdley GC. Laparoscopic adrenalectomy for adrenal cancer: a systematic review. Am Surg. 2016; 82:420–6.15. Henry JF, Peix JL, Kraimps JL. Positional statement of the European Society of Endocrine Surgeons (ESES) on malignant adrenal tumors. Langenbecks Arch Surg. 2012; 397:145–6.
Article16. Chen JY, Ardestani A, Tavakkoli A. Laparoscopic adrenal metastasectomy: appropriate, safe, and feasible. Surg Endosc. 2014; 28:816–20.
Article17. Walz MK, Alesina PF, Wenger FA, Deligiannis A, Szuczik E, Petersenn S, et al. Posterior retroperitoneoscopic adrenalectomy: results of 560 procedures in 520 patients. Surgery. 2006; 140:943–8.
Article18. Gavriilidis P, Camenzuli C, Paspala A, Di Marco AN, Palazzo FF. Posterior retroperitoneoscopic versus laparoscopic transperitoneal adrenalectomy: a systematic review by an updated meta-analysis. World J Surg. 2020. Aug. 27. [Epub]. https://doi.org/10.1007/s00268-020-05759-w.
Article19. Chai YJ, Yu HW, Song RY, Kim SJ, Choi JY, Lee KE. Lateral transperitoneal adrenalectomy versus posterior retroperitoneoscopic adrenalectomy for benign adrenal gland disease: randomized controlled trial at a single tertiary medical center. Ann Surg. 2019; 269:842–8.20. Abraham MA, Jose R, Paul MJ. Seesawing end-tidal carbon dioxide: portent of critical carbon dioxide embolism in retroperitoneoscopy. BMJ Case Rep. 2018; 2018:bcr2017219397.
Article21. Ban EJ, Yap Z, Kandil E, Lee CR, Kang SW, Lee J, et al. Hemodynamic stability during adrenalectomy for pheochromocytoma: a case control study of posterior retroperitoneal vs lateral transperitoneal approaches. Medicine (Baltimore). 2020; 99:e19104.22. Constantinides VA, Christakis I, Touska P, Meeran K, Palazzo F. Retroperitoneoscopic or laparoscopic adrenalectomy? A single-centre UK experience. Surg Endosc. 2013; 27:4147–52.
Article23. Barczynski M, Konturek A, Nowak W. Randomized clinical trial of posterior retroperitoneoscopic adrenalectomy versus lateral transperitoneal laparoscopic adrenalectomy with a 5-year follow-up. Ann Surg. 2014; 260:740–7.
Article24. Ottlakan A, Paszt A, Simonka Z, Abraham S, Borda B, Vas M, et al. Laparoscopic transperitoneal and retroperitoneal adrenalectomy: a 20-year, single-institution experience with an analysis of the learning curve and tumor size [lap transper and retroper adrenalectomy]. Surg Endosc. 2020; 34:5421–7.
Article25. Tuncel A, Langenhuijsen J, Erkan A, Mikhaylikov T, Arslan M, Aslan Y, et al. Comparison of synchronous bilateral transperitoneal and posterior retroperitoneal laparoscopic adrenalectomy: results of a multicenter study. Surg Endosc. 2020. Mar. 9. [Epub]. https://doi.org/10.1007/s00464-020-07474-y.
Article26. Cabalag MS, Mann GB, Gorelik A, Miller JA. Comparison of outcomes after laparoscopic versus posterior retroperitoneoscopic adrenalectomy: a pilot study. Surg Laparosc Endosc Percutan Tech. 2014; 24:62–6.27. Lee CR, Walz MK, Park S, Park JH, Jeong JS, Lee SH, et al. A comparative study of the transperitoneal and posterior retroperitoneal approaches for laparoscopic adrenalectomy for adrenal tumors. Ann Surg Oncol. 2012; 19:2629–34.
Article28. Dickson PV, Alex GC, Grubbs EG, Ayala-Ramirez M, Jimenez C, Evans DB, et al. Posterior retroperitoneoscopic adrenalectomy is a safe and effective alternative to transabdominal laparoscopic adrenalectomy for pheochromocytoma. Surgery. 2011; 150:452–8.
Article29. Nigri G, Rosman AS, Petrucciani N, Fancellu A, Pisano M, Zorcolo L, et al. Meta-analysis of trials comparing laparoscopic transperitoneal and retroperitoneal adrenalectomy. Surgery. 2013; 153:111–9.
Article30. Rubinstein M, Gill IS, Aron M, Kilciler M, Meraney AM, Finelli A, et al. Prospective, randomized comparison of transperitoneal versus retroperitoneal laparoscopic adrenalectomy. J Urol. 2005; 174:442–5.
Article31. Irvin GL 3rd, Fishman LM, Sher JA. Familial pheochromocytoma. Surgery. 1983; 94:938–40.32. Seyam R, Khalil MI, Kamel MH, Altaweel WM, Davis R, Bissada NK. Organ-sparing procedures in GU cancer: part 1-organ-sparing procedures in renal and adrenal tumors: a systematic review. Int Urol Nephrol. 2019; 51:377–93.
Article33. Janetschek G, Finkenstedt G, Gasser R, Waibel UG, Peschel R, Bartsch G, et al. Laparoscopic surgery for pheochromocytoma: adrenalectomy, partial resection, excision of paragangliomas. J Urol. 1998; 160:330–4.
Article34. Nakada T, Kubota Y, Sasagawa I, Yagisawa T, Watanabe M, Ishigooka M. Therapeutic outcome of primary aldosteronism: adrenalectomy versus enucleation of aldosterone-producing adenoma. J Urol. 1995; 153:1775–80.
Article35. Mitchell J, Barbosa G, Tsinberg M, Milas M, Siperstein A, Berber E. Unrecognized adrenal insufficiency in patients undergoing laparoscopic adrenalectomy. Surg Endosc. 2009; 23:248–54.
Article36. Perysinakis I, Aggeli C, Kaltsas G, Zografos GN. Adrenal-sparing surgery: current concepts on a theme from the past. Hormones (Athens). 2020; 19:317–27.
Article37. Asari R, Scheuba C, Kaczirek K, Niederle B. Estimated risk of pheochromocytoma recurrence after adrenal-sparing surgery in patients with multiple endocrine neoplasia type 2A. Arch Surg. 2006; 141:1199–205.
Article38. Castinetti F, Taieb D, Henry JF, Walz M, Guerin C, Brue T, et al. Management of endocrine disease: outcome of adrenal sparing surgery in heritable pheochromocytoma. Eur J Endocrinol. 2016; 174:R9–18.
Article39. Kaye DR, Storey BB, Pacak K, Pinto PA, Linehan WM, Bratslavsky G. Partial adrenalectomy: underused first line therapy for small adrenal tumors. J Urol. 2010; 184:18–25.
Article40. Lee JE, Curley SA, Gagel RF, Evans DB, Hickey RC. Cortical-sparing adrenalectomy for patients with bilateral pheochromocytoma. Surgery. 1996; 120:1064–70.
Article41. Castinetti F, Qi XP, Walz MK, Maia AL, Sanso G, Peczkowska M, et al. Outcomes of adrenal-sparing surgery or total adrenalectomy in phaeochromocytoma associated with multiple endocrine neoplasia type 2: an international retrospective population-based study. Lancet Oncol. 2014; 15:648–55.
Article42. Balci M, Tuncel A, Aslan Y, Aykanat C, Berker D, Guzel O. Laparoscopic partial versus total adrenalectomy in nonhereditary unilateral adrenal masses. Urol Int. 2020; 104:75–80.
Article43. Gomella PT, Sanford TH, Pinto PA, Bratslavsky G, Metwalli AR, Linehan WM, et al. Long-term functional and oncologic outcomes of partial adrenalectomy for pheochromocytoma. Urology. 2020; 140:85–90.
Article44. Fu B, Zhang X, Wang GX, Lang B, Ma X, Li HZ, et al. Long-term results of a prospective, randomized trial comparing retroperitoneoscopic partial versus total adrenalectomy for aldosterone producing adenoma. J Urol. 2011; 185:1578–82.
Article45. Lenders JW, Duh QY, Eisenhofer G, Gimenez-Roqueplo AP, Grebe SK, Murad MH, et al. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2014; 99:1915–42.
Article46. Jeschke K, Janetschek G, Peschel R, Schellander L, Bartsch G, Henning K. Laparoscopic partial adrenalectomy in patients with aldosterone-producing adenomas: indications, technique, and results. Urology. 2003; 61:69–72.
Article47. Colleselli D, Janetschek G. Current trends in partial adrenalectomy. Curr Opin Urol. 2015; 25:89–94.
Article48. Grubbs EG, Rich TA, Ng C, Bhosale PR, Jimenez C, Evans DB, et al. Long-term outcomes of surgical treatment for hereditary pheochromocytoma. J Am Coll Surg. 2013; 216:280–9.
Article49. Walz MK, Peitgen K, Diesing D, Petersenn S, Janssen OE, Philipp T, et al. Partial versus total adrenalectomy by the posterior retroperitoneoscopic approach: early and long-term results of 325 consecutive procedures in primary adrenal neoplasias. World J Surg. 2004; 28:1323–9.
Article50. Uludag M, Aygun N, Isgor A. Surgical indications and techniques for adrenalectomy. Sisli Etfal Hastan Tip Bul. 2020; 54:8–22.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A New Beginning for the Journal of Minimally Invasive Surgery for the International Recognition and Contribution of Scientific Development of Minimally Invasive Surgery
- Robotic assisted adrenalectomy: Is it ready for prime time?
- Establishment of Minimally Invasive Thoracic Surgery Program
- A Late Adopter's Perspective on Minimally Invasive Surgery: Presidential Lecture at KSEL 2018
- Transperitoneal Laparoscopic Removal of Adrenal Ganglioneuroma