Ann Pediatr Endocrinol Metab.
2020 Dec;25(4):265-271. 10.6065/apem.2040098.049.
Limitations of current screening methods for lipid disorders in Korean adolescents and a proposal for an effective detection method: a nationwide, cross-sectional study
- Affiliations
-
- 1Department of Pediatrics, Good Moonhwa Hospital, Busan, Korea
- 2Department of Pediatrics, College of Medicine, Dong-A University, Busan, Korea
- KMID: 2510898
- DOI: http://doi.org/10.6065/apem.2040098.049
Abstract
- Purpose
To determine the limitations of current screening methods for lipid disorders and to suggest a new method that is effective for use in Korean adolescents.
Methods
Data from the 6th Korea National Health and Nutrition Examination Survey (2013–2015) were analyzed. The diagnostic validity (sensitivity and specificity) of various cardiovascular risk factors currently used for lipid disorder screening was investigated, as was the diagnostic validity of non-HDL-cholesterol ≥145 mg/dL as a screening tool.
Results
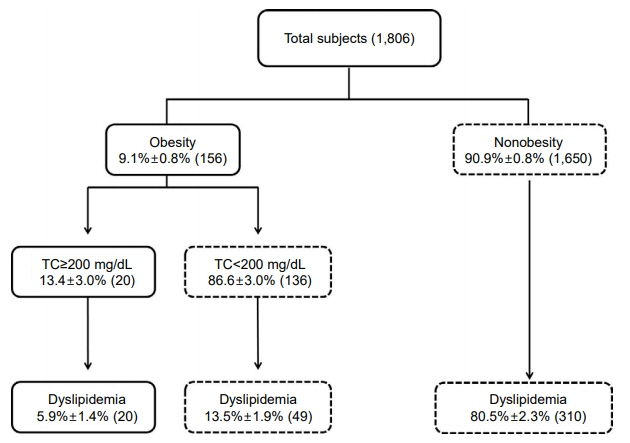
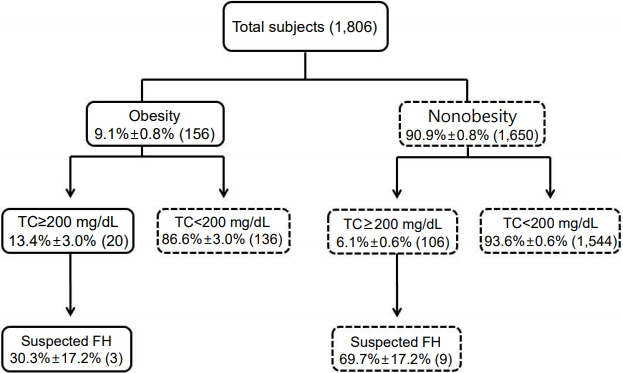
The prevalence of dyslipidemia and familial hypercholesterolemia (FH) among Korean adolescents was 20.4%±1.0% and 0.8%±0.3%, respectively. The current standard screening methods identified only 5.9%±1.4% and 30.3%±17.2% of the total number of dyslipidemia and FH cases, respectively. The diagnostic sensitivity and specificity of lipid profile analysis for dyslipidemia among obese adolescents were 19.5%±2.3% and 93.6%±0.8% and for FH were 30.3%±17.2% and 91.1%±0.8%, respectively. When adolescents with obesity, hypertension, or a family history of dyslipidemia or cardiocerebrovascular disease for over 3 generations were included in the screening, diagnostic sensitivity increased to 68.4%±2.8% for dyslipidemia and 83.5%±2.7% for FH. Universal screening of all adolescents based on non-HDL-cholesterol levels had sensitivities of 30.2%±2.7% and 100%, and specificities of 99.2%±0.3% and 94%±0.6% for dyslipidemia and FH, respectively.
Conclusion
New screening methods should be considered for early diagnosis and treatment of lipid disorders in Korean adolescents.
Figure
Cited by 1 articles
-
Screening and Management for Dyslipidemia in Korean Children and Adolescents
Jong Seo Yoon, Il Tae Hwang
Ewha Med J. 2022;45(3):e4. doi: 10.12771/emj.2022.e4.
Reference
-
References
1. Kannel WB, Castelli WP, Gordon T. Cholesterol in the prediction of atherosclerotic disease. New perspectives based on the Framingham study. Ann Intern Med. 1979; 90:85–91.
Article2. Berenson GS, Srinivasan SR, Bao W, Newman WP 3rd, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med. 1998; 338:1650–6.
Article3. McGill HC Jr, McMahan CA, Malcom GT, Oalmann MC, Strong JP. Effects of serum lipoproteins and smoking on atherosclerosis in young men and women. The PDAY Research Group. Pathobiological determinants of atherosclerosis in youth. Arterioscler Thromb Vasc Biol. 1997; 17:95–106.
Article4. McGill HC Jr, McMahan CA, Zieske AW, Malcom GT, Tracy RE, Strong JP. Effects of nonlipid risk factors on atherosclerosis in youth with a favorable lipoprotein profile. Circulation. 2001; 103:1546–50.
Article5. National Cholesterol Education Program (NCEP): highlights of the report of the Expert Panel on Blood Cholesterol Levels in Children and Adolescents. Pediatrics. 1992; 89:495–501.6. Kavey RE, Daniels SR, Lauer RM, Atkins DL, Hayman LL, Taubert K, et al. American Heart Association guidelines for primary prevention of atherosclerotic cardiovascular disease beginning in childhood. Circulation. 2003; 107:1562–6.
Article7. Daniels SR, Greer FR, Committee on N. Lipid screening and cardiovascular health in childhood. Pediatrics. 2008; 122:198–208.
Article8. Expert Panel on Integrated Guidelines for Cardiovascular H, Risk Reduction in C, Adolescents, National Heart L, Blood I. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011; 128 Suppl 5:S213–56.9. Bittner V, Hardison R, Kelsey SF, Weiner BH, Jacobs AK, Sopko G, et al. Non-high-density lipoprotein cholesterol levels predict five-year outcome in the Bypass Angioplasty Revascularization Investigation (BARI). Circulation. 2002; 106:2537–42.
Article10. Frontini MG, Srinivasan SR, Xu J, Tang R, Bond MG, Berenson GS. Usefulness of childhood non-high density lipoprotein cholesterol levels versus other lipoprotein measures in predicting adult subclinical atherosclerosis: the Bogalusa Heart Study. Pediatrics. 2008; 121:924–9.
Article11. Sigdel M, Yadav BK, Gyawali P, Regmi P, Baral S, Regmi SR, et al. Non-high density lipoprotein cholesterol versus low density lipoprotein cholesterol as a discriminating factor for myocardial infarction. BMC Res Notes. 2012; 5:640.
Article12. van Deventer HE, Miller WG, Myers GL, Sakurabayashi I, Bachmann LM, Caudill SP, et al. Non-HDL cholesterol shows improved accuracy for cardiovascular risk score classification compared to direct or calculated LDL cholesterol in a dyslipidemic population. Clin Chem. 2011; 57:490–501.
Article13. Lim JS. The current state of dyslipidemia in Korean children and adolescents and its management in clinical practice. Ann Pediatr Endocrinol Metab. 2013; 18:1–8.
Article14. Yun YM, Song J, Ji M, Kim JH, Kim Y, Park T, et al. Calibration of high-density lipoprotein cholesterol values from the Korea National Health and Nutrition Examination Survey Data, 2008 to 2015. Ann Lab Med. 2017; 37:1–8.
Article15. Yang S, Hwang JS, Park HK, Lee HS, Kim HS, Kim EY, et al. Serum lipid concentrations, prevalence of dyslipidemia, and percentage eligible for pharmacological treatment of Korean children and adolescents; data from the Korea National Health and Nutrition Examination Survey IV (2007-2009). PLoS One. 2012; 7:e49253.
Article16. Dennison BA, Jenkins PL, Pearson TA. Challenges to implementing the current pediatric cholesterol screening guidelines into practice. Pediatrics. 1994; 94:296–302.
Article17. Ritchie SK, Murphy EC, Ice C, Cottrell LA, Minor V, Elliott E, et al. Universal versus targeted blood cholesterol screening among youth: The CARDIAC project. Pediatrics. 2010; 126:260–5.
Article18. Farwell WR, Sesso HD, Buring JE, Gaziano JM. Non-high-density lipoprotein cholesterol versus low-density lipoprotein cholesterol as a risk factor for a first nonfatal myocardial infarction. Am J Cardiol. 2005; 96:1129–34.
Article19. Pischon T, Girman CJ, Sacks FM, Rifai N, Stampfer MJ, Rimm EB. Non-high-density lipoprotein cholesterol and apolipoprotein B in the prediction of coronary heart disease in men. Circulation. 2005; 112:3375–83.
Article20. Miller M, Ginsberg HN, Schaefer EJ. Relative atherogenicity and predictive value of non-high-density lipoprotein cholesterol for coronary heart disease. Am J Cardiol. 2008; 101:1003–8.
Article21. Shim YS, Baek JW, Kang MJ, Oh YJ, Yang S, Hwang IT. Reference values for the triglyceride to high-density lipoprotein cholesterol ratio and non-high-density lipoprotein cholesterol in Korean children and adolescents: the Korean National Health and Nutrition Examination Surveys 2007-2013. J Atheroscler Thromb. 2016; 23:1334–44.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Loneliness and Depressive Symptoms on Smartphone Overdependence among South Korean Adolescents: A Nationwide Cross-Sectional Study
- Trends in Cancer Screening Rates among Korean Men and Women: Results of the Korean National Cancer Screening Survey, 2004-2013
- Analysis of Hepatobiliary Disorders from a Nationwide Survey ofDischarge Data in Korean Children and Adolescents
- Lung Cancer Screening with Low-Dose CT: Current Status in Other Countries
- Screening and Management for Dyslipidemia in Korean Children and Adolescents