Ann Pediatr Endocrinol Metab.
2020 Dec;25(4):240-247. 10.6065/apem.2040018.009.
Discriminatory performance of insulin-like growth factor 1 and insulin-like growth factor binding protein-3 by correlating values to chronological age, bone age, and pubertal status for diagnosis of isolated growth hormone deficiency
- Affiliations
-
- 1Department of Pediatrics, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2510895
- DOI: http://doi.org/10.6065/apem.2040018.009
Abstract
- Purpose
The discriminatory performance of insulin-like growth factor 1 (IGF-1) and insulin-like growth factor binding protein-3 (IGFBP-3) was investigated by correlating their values with chronological age (CA), bone age (BA), and pubertal status (PS) for diagnosis of isolated growth hormone deficiency (IGHD).
Methods
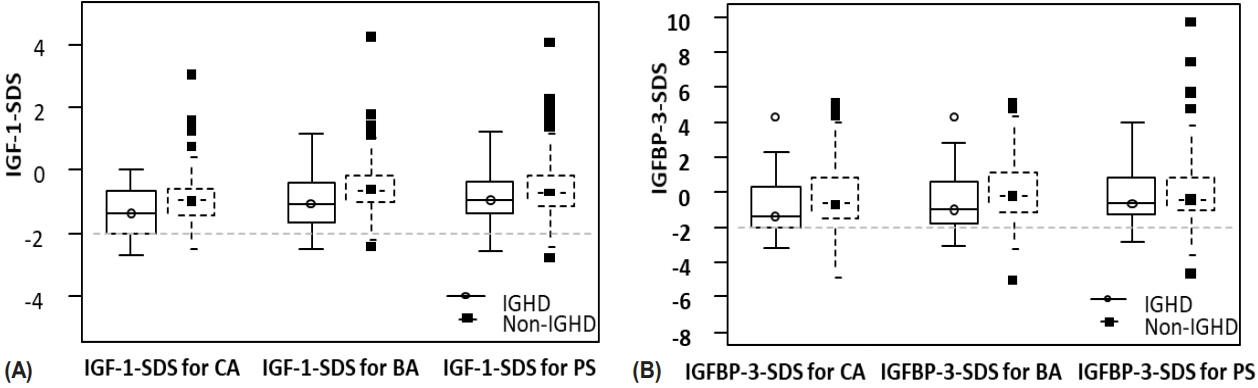
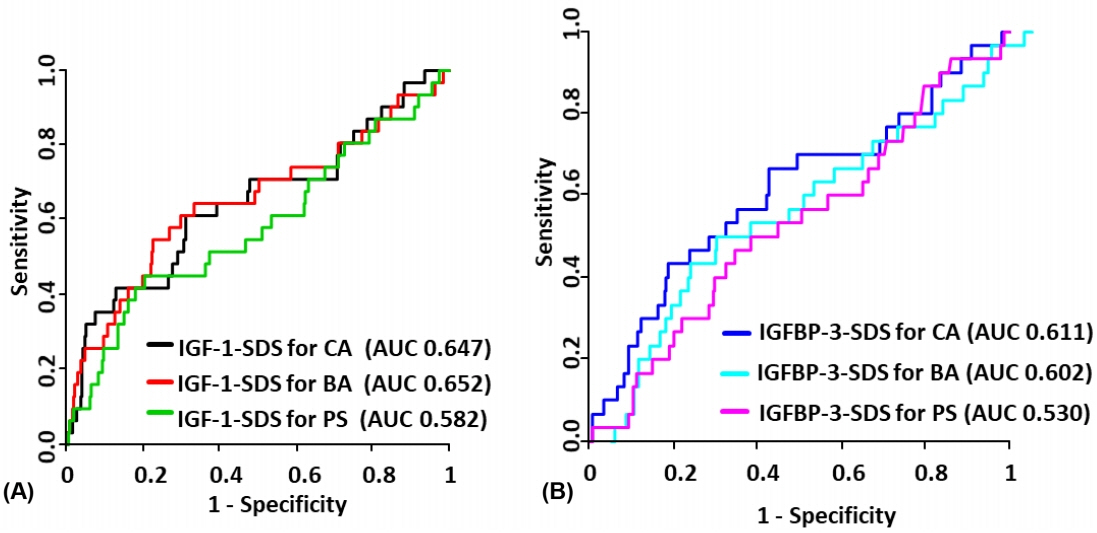
We evaluated IGF-1 and IGFBP-3 levels in 310 short-stature subjects subdivided into 2 groups: IGHD (n=31) and non-IGHD (n=279). IGF-1 and IGFBP-3 were assayed using immune-radiometric assay and transformed into standard deviation score (SDS) according to CA, BA, and PS.
Results
The highest sensitivity was found in IGF-1-SDS for CA and IGFBP-3-SDS for CA (22.6% and 30.0%, respectively). The highest specificity was found in IGF-1-SDS for PS and IGFBP-3-SDS for PS (98.2% and 94.4%, respectively). Groups with the highest positive predictive values were IGF-1-SDS for BA and IGFBP-3-SDS for BA (10.9% and 5.1%, respectively). Highest negative predictive values were seen in IGF-1-SDS for CA and IGFBP-3-SDS for CA (98.4% and 98.4%, respectively).
Conclusion
IGF-1-SDS for CA, instead of IGF-1-SDS for BA or PS, could be used as a standard variable for IGHD screening. The sufficiently high specificity of IGF-1-SDS for PS suggests that this value is a useful tool for identification of IGHD.
Keyword
Figure
Cited by 1 articles
-
Approach to Short Stature in Children and Adolescent
Hyo-Kyoung Nam
Ewha Med J. 2021;44(4):111-116. doi: 10.12771/emj.2021.44.4.111.
Reference
-
References
1. Kim JH, Yun S, Hwang SS, Shim JO, Chae HW, Lee YJ, et al. The 2017 Korean National Growth Charts for children and adolescents: development, improvement, and prospects. Korean J Pediatr. 2018; 61:135–49.
Article2. Richmond E, Rogol AD. Testing for growth hormone deficiency in children. Growth Horm IGF Res. 2019; 50:57–60.
Article3. Lindsay R, Feldkamp M, Harris D, Robertson J, Rallison M. Utah Growth Study: growth standards and the prevalence of growth hormone deficiency. J Pediatr. 1994; 125:29–35.
Article4. Rona RJ, Tanner JM. Aetiology of idiopathic growth hormone deficiency in England and Wales. Arch Dis Child. 1977; 52:197–208.
Article5. Vimpani GV, Vimpani AF, Lidgard GP, Cameron EH, Farquhar JW. Prevalence of severe growth hormone deficiency. Br Med J. 1977; 2:427–30.
Article6. Bao XL, Shi YF, Du YC, Liu R, Deng JY, Gao SM. Prevalence of growth hormone deficiency of children in Beijing. Chin Med J (Engl). 1992; 105:401–5.7. Velayutham K, Selvan SSA, Jeyabalaji RV, Balaji S. Prevalence and etiological profile of short stature among school children in a South Indian population. Indian J Endocrinol Metab. 2017; 21:820–2.
Article8. Ahmed ML, Allen AD, Sharma A, Macfarlane JA, Dunger DB. Evaluation of a district growth screening programme: the Oxford Growth Study. Arch Dis Child. 1993; 69:361–5.
Article9. Marin G, Domene HM, Barnes KM, Blackwell BJ, Cassorla FG, Cutler GB Jr. The effects of estrogen priming and puberty on the growth hormone response to standardized treadmill exercise and arginine-insulin in normal girls and boys. J Clin Endocrinol Metab. 1994; 79:537–41.
Article10. Martinez AS, Domene HM, Ropelato MG, Jasper HG, Pennisi PA, Escobar ME, et al. Estrogen priming effect on growth hormone (GH) provocative test: a useful tool for the diagnosis of GH deficiency. J Clin Endocrinol Metab. 2000; 85:4168–72.
Article11. Devesa J, Lima L, Lois N, Fraga C, Lechuga MJ, Arce V, et al. Reasons for the variability in growth hormone (GH) responses to GHRH challenge: the endogenous hypo - thalamic-somatotroph rhythm (HSR). Clin Endocrinol (Oxf). 1989; 30:367–77.12. Hyun SE, Lee BC, Suh BK, Chung SC, Ko CW, Kim HS, et al. Reference values for serum levels of insulin-like growth factor-I and insulin-like growth factor binding protein-3 in Korean children and adolescents. Clin Biochem. 2012; 45:16–21.
Article13. Consensus guidelines for the diagnosis and treatment of growth hormone (GH) deficiency in childhood and adolescence: summary statement of the GH Research Society. GH Research Society. J Clin Endocrinol Metab. 2000; 85:3990–3.14. Maxim LD, Niebo R, Utell MJ. Screening tests: a review with examples. Inhal Toxicol. 2014; 26:811–28.
Article15. Fayter D, Nixon J, Hartley S, Rithalia A, Butler G, Rudolf M, et al. Effectiveness and cost-effectiveness of heightscreening programmes during the primary school years: a systematic review. Arch Dis Child. 2008; 93:278–84.
Article16. Simundic AM. Measures of diagnostic accuracy: basic definitions. Ejifcc. 2009; 19:203–11.17. Inoue-Lima TH, Vasques GA, Scalco RC, Nakaguma M, Mendonca BB, Arnhold IJP, et al. IGF-1 assessed by pubertal status has the best positive predictive power for GH deficiency diagnosis in peripubertal children. J Pediatr Endocrinol Metab. 2019; 32:173–9.
Article18. Cianfarani S, Tondinelli T, Spadoni GL, Scire G, Boemi S, Boscherini B. Height velocity and IGF-I assessment in the diagnosis of childhood onset GH insufficiency: do we still need a second GH stimulation test? Clin Endocrinol (Oxf). 2002; 57:161–7.
Article19. Felicio JS, Janau LC, Moraes MA, Zahalan NA, de Souza Resende F, de Lemos MN, et al. Diagnosis of idiopathic GHD in children based on response to rhGH treatment: the importance of GH provocative tests and IGF-1. Front Endocrinol (Lausanne). 2019; 10:638.20. Marwaha RK, Garg MK, Gupta S, Khurana AK, Narang A, Shukla M, et al. Assessment of insulin like growth factor-1 and IGF binding protein-3 in healthy Indian girls from Delhi and their correlation with age, pubertal status, obesity and thyroid hormonal status. J Pediatr Endocrinol Metab. 2017; 30:739–47.
Article21. Saggese G, Ranke MB, Saenger P, Rosenfeld RG, Tanaka T, Chaussain JL, et al. Diagnosis and treatment of growth hormone deficiency in children and adolescents: towards a consensus. Ten years after the Availability of Recombinant Human Growth Hormone Workshop held in Pisa, Italy, 27- 28 March 1998. Horm Res. 1998; 50:320–40.22. Loche S, Bizzarri C, Maghnie M, Faedda A, Tzialla C, Autelli M, et al. Results of early reevaluation of growth hormone secretion in short children with apparent growth hormone deficiency. J Pediatr. 2002; 140:445–9.
Article23. Wacharasindhu S, Supornsilchai V, Aroonparkmongkol S, Srivuthana S. Diagnosis and growth hormone (GH) therapy in children with GH deficiency: experience in King Chulalongkorn Memorial Hospital, Thailand. J Med Assoc Thai. 2007; 90:2047–52.24. Zadik Z, Chalew SA, Kowarski A. Assessment of growth hormone secretion in normal stature children using 24- hour integrated concentration of GH and pharmacological stimulation. J Clin Endocrinol Metab. 1990; 71:932–6.25. Ghigo E, Bellone J, Aimaretti G, Bellone S, Loche S, Cappa M, et al. Reliability of provocative tests to assess growth hormone secretory status. Study in 472 normally growing children. J Clin Endocrinol Metab. 1996; 81:3323–7.
Article26. Stanley T. Diagnosis of growth hormone deficiency in childhood. Curr Opin Endocrinol Diabetes Obes. 2012; 19:47–52.
Article27. Hintz RL. The role of auxologic and growth factor measurements in the diagnosis of growth hormone deficiency. Pediatrics. 1998; 102:524–6.
Article28. Horner JM, Thorsson AV, Hintz RL. Growth deceleration patterns in children with constitutional short stature: an aid to diagnosis. Pediatrics. 1978; 62:529–34.
Article29. Savastano S, Di Somma C, Belfiore A, Guida B, Orio F Jr, Rota F, et al. Growth hormone status in morbidly obese subjects and correlation with body composition. J Endocrinol Invest. 2006; 29:536–43.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship of Insulin like Growth Factor I with Pharmacologically Stimulated Growth Hormone Secretion in Growth Hormone Deficient Children
- Serum levels of free insulin-like growth factor-I and clinical value in healthy children
- Profile of Insulin, Growth Hormone and Insulin-like Growth Factors in Human Cord Blood According to Birth Weight
- Growth and Pituitary Hormonal Status in Children with Craniopharyngioma
- The Role of the Insulin-like Growth Factors and Insulin-like Growth Factor Binding Proteins in Growth Disorders