Ann Rehabil Med.
2020 Dec;44(6):493-501. 10.5535/arm.20016.
Effects of Chin-Down Maneuver on Pharyngeal Pressure Generation According to Dysphagia and Viscosity
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul National University Hospital, Seoul, Korea
- 2Department of Rehabilitation Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 3Department of Rehabilitation Medicine, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2510816
- DOI: http://doi.org/10.5535/arm.20016
Abstract
Objective
To demonstrate the effects of chin-down maneuver on swallowing by using high-resolution manometry (HRM).
Methods
HRM data of 20 healthy subjects and 64 dysphagic patients were analyzed. Participants swallowed 5 mL of thin and honey-like liquids in neutral and chin-down positions. HRM was used to evaluate maximal velopharyngeal pressure/area, maximal tongue base pressure/area, maximal pharyngeal constrictor pressure, pre-/post-swallow upper esophageal sphincter (UES) peak pressure, minimal UES pressure, UES activity time, and nadir duration.
Results
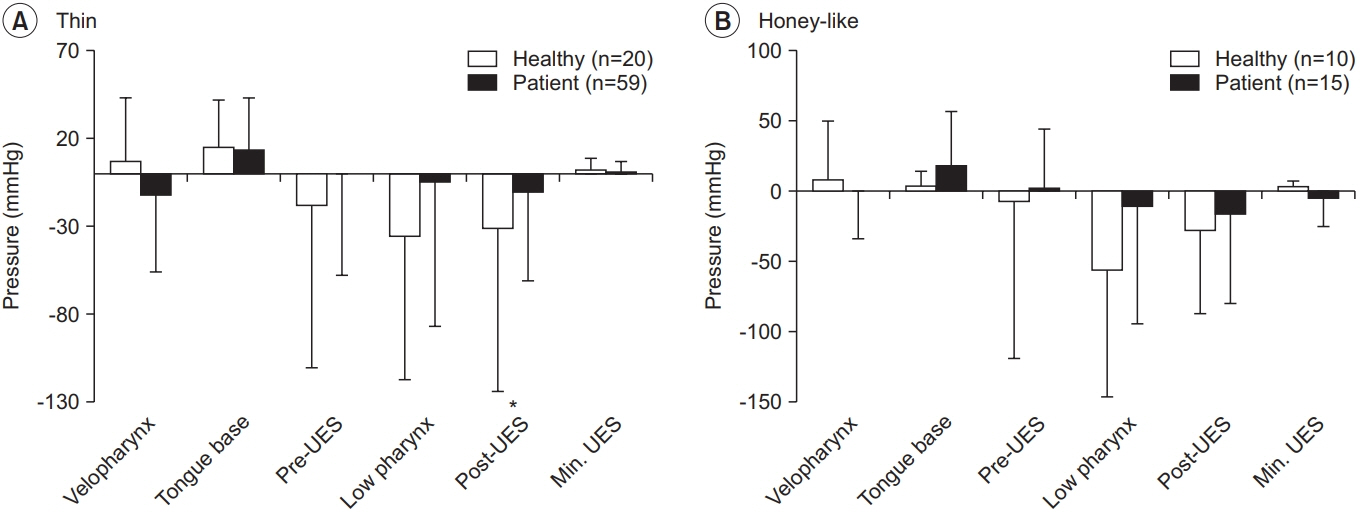
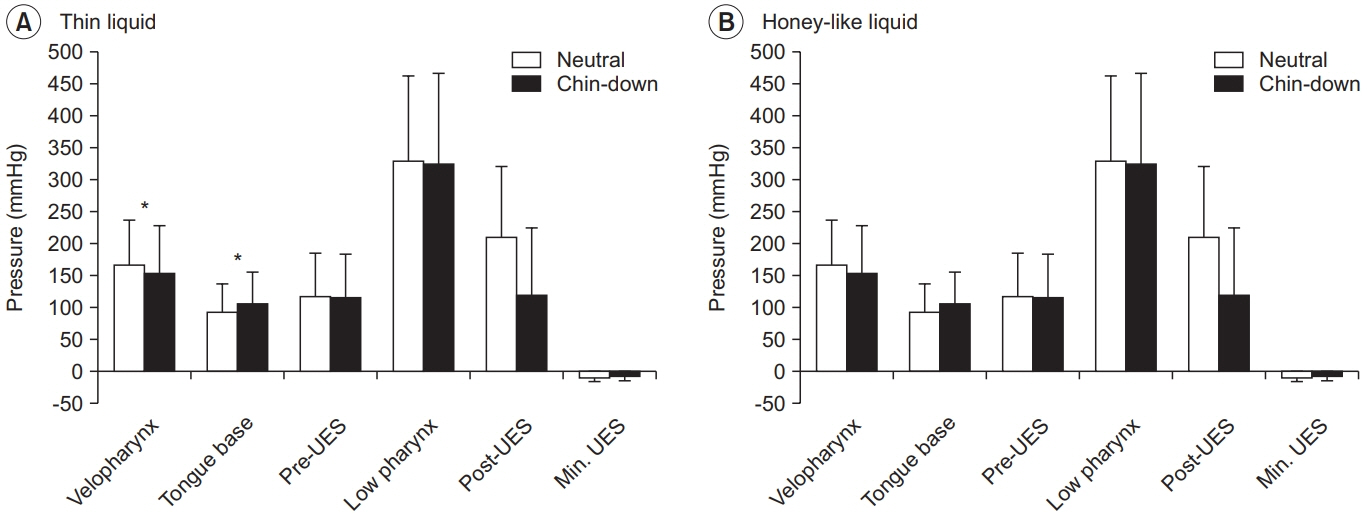
Compared to the neutral position, the chin-down maneuver significantly increased tongue base pressure in both normal and dysphagic groups as well as for both honey-like and thin viscosities, although the honey-like liquid did not reach statistical significance in the dysphagic group. Regarding pharyngeal constrictors and pre-swallow peak UES pressure, the healthy group showed a significant decrease in thin liquid swallowing and decreasing tendency in honeylike liquid swallowing. UES nadir duration was significantly decreased for honey-like liquid swallowing in the dysphagic group and for both thin and honey-like liquids in the healthy group. UES nadir duration of honey-like and thin flow swallowing in the dysphagia group was 0.26 seconds after the chin-down maneuver, which was severely limited.
Conclusion
This study showed a different kinetic effect of the chin-down maneuver between the healthy and dysphagic groups, as well as between thin and honey-like viscosities. The chin-down maneuver increased tongue base pressure and decreased UES nadir duration, which the latter was severely limited in dysphagic patients. Therefore, appropriate application of the chin-down maneuver in clinical practice is required.
Keyword
Figure
Cited by 1 articles
-
Correlation Between Articulatory Diadochokinetic Parameters and Dysphagia Parameters in Subacute Stroke Patients
Back Min Oh, Hyun Seok, Sang-Hyun Kim, Seung Yeol Lee, Su Jung Park, Beom Jin Kim, Hyun Jung Kim
Ann Rehabil Med. 2023;47(3):192-204. doi: 10.5535/arm.23018.
Reference
-
1. Logemann JA. Evaluation and treatment of swallowing disorders. 2nd ed. Austin, TX: Pro-Ed;1998.2. Bulow M, Olsson R, Ekberg O. Videomanometric analysis of supraglottic swallow, effortful swallow, and chin tuck in healthy volunteers. Dysphagia. 1999; 14:67–72.
Article3. Welch MV, Logemann JA, Rademaker AW, Kahrilas PJ. Changes in pharyngeal dimensions effected by chin tuck. Arch Phys Med Rehabil. 1993; 74:178–81.4. Terre R, Mearin F. Effectiveness of chin-down posture to prevent tracheal aspiration in dysphagia secondary to acquired brain injury: a videofluoroscopy study. Neurogastroenterol Motil. 2012; 24:414–9.5. Solazzo A, Monaco L, Del Vecchio L, Tamburrini S, Iacobellis F, Berritto D, et al. Investigation of compensatory postures with videofluoromanometry in dysphagia patients. World J Gastroenterol. 2012; 18:2973–8.
Article6. Logemann JA, Gensler G, Robbins J, Lindblad AS, Brandt D, Hind JA, et al. A randomized study of three interventions for aspiration of thin liquids in patients with dementia or Parkinson’s disease. J Speech Lang Hear Res. 2008; 51:173–83.
Article7. Park D, Shin CM, Ryu JS. Effect of different viscosities on pharyngeal pressure during swallowing: a study using high-resolution manometry. Arch Phys Med Rehabil. 2017; 98:487–94.
Article8. Ryu JS, Park D, Oh Y, Lee ST, Kang JY. The effects of bolus volume and texture on pharyngeal pressure events using high-resolution manometry and its comparison with videofluoroscopic swallowing study. J Neurogastroenterol Motil. 2016; 22:231–9.
Article9. Castell JA, Castell DO. Manometric analysis of the pharyngo-esophageal segment. Indian J Gastroenterol. 1994; 13:58–63.10. Castell JA, Castell DO, Schultz AR, Georgeson S. Effect of head position on the dynamics of the upper esophageal sphincter and pharynx. Dysphagia. 1993; 8:1–6.
Article11. Balou M, McCullough GH, Aduli F, Brown D, Stack BC Jr, Snoddy P, et al. Manometric measures of head rotation and chin tuck in healthy participants. Dysphagia. 2014; 29:25–32.
Article12. American Dietetic Association. National dysphagia diet: standardization for optimal care. Chicago, IL: American Dietetic Association;2002.13. Leigh JH, Oh BM, Seo HG, Lee GJ, Min Y, Kim K, et al. Influence of the chin-down and chin-tuck maneuver on the swallowing kinematics of healthy adults. Dysphagia. 2015; 30:89–98.
Article14. Ryu JS, Park DH, Kang JY. Application and interpretation of high-resolution manometry for pharyngeal dysphagia. J Neurogastroenterol Motil. 2015; 21:283–7.
Article15. Kim CK, Ryu JS, Song SH, Koo JH, Lee KD, Park HS, et al. Effects of head rotation and head tilt on pharyngeal pressure events using high resolution manometry. Ann Rehabil Med. 2015; 39:425–31.
Article16. Park D, Oh Y, Ryu JS. Findings of abnormal videofluoroscopic swallowing study identified by high-resolution manometry parameters. Arch Phys Med Rehabil. 2016; 97:421–8.
Article17. Jungheim M, Miller S, Ptok M. Methodologische Aspekte zur Hochauflosungsmanometrie des Pharynx und des oberen Osophagussphinkters [Methodological aspects of high resolution manometry of the pharynx and upper esophageal sphincter]. Laryngorhinootologie. 2013; 92:158–64.18. Fox MR, Bredenoord AJ. Oesophageal high-resolution manometry: moving from research into clinical practice. Gut. 2008; 57:405–23.
Article19. Takasaki K, Umeki H, Enatsu K, Tanaka F, Sakihama N, Kumagami H, et al. Investigation of pharyngeal swallowing function using high-resolution manometry. Laryngoscope. 2008; 118:1729–32.
Article20. Geng Z, Hoffman MR, Jones CA, McCulloch TM, Jiang JJ. Three-dimensional analysis of pharyngeal high-resolution manometry data. Laryngoscope. 2013; 123:1746–53.
Article21. Bulow M, Olsson R, Ekberg O. Videomanometric analysis of supraglottic swallow, effortful swallow, and chin tuck in patients with pharyngeal dysfunction. Dysphagia. 2001; 16:190–5.
Article22. McCulloch TM, Hoffman MR, Ciucci MR. High-resolution manometry of pharyngeal swallow pressure events associated with head turn and chin tuck. Ann Otol Rhinol Laryngol. 2010; 119:369–76.
Article23. Hori K, Tamine K, Barbezat C, Maeda Y, Yamori M, Muller F, et al. Influence of chin-down posture on tongue pressure during dry swallow and bolus swallows in healthy subjects. Dysphagia. 2011; 26:238–45.
Article24. Ayuse T, Ayuse T, Ishitobi S, Kurata S, Sakamoto E, Okayasu I, et al. Effect of reclining and chin-tuck position on the coordination between respiration and swallowing. J Oral Rehabil. 2006; 33:402–8.
Article25. Knigge MA, Thibeault S. Relationship between tongue base region pressures and vallecular clearance. Dysphagia. 2016; 31:391–7.
Article26. Lee SI, Yoo JY, Kim M, Ryu JS. Changes of timing variables in swallowing of boluses with different viscosities in patients with dysphagia. Arch Phys Med Rehabil. 2013; 94:120–6.
Article27. Oh Y, Lee ST, Ryu JS. High resolution manometry analysis of a patient with dysphagia after occiputC3/4 posterior fusion operation. Ann Rehabil Med. 2015; 39:1028–32.
Article28. Goyal RK. Disorders of the cricopharyngeus muscle. Otolaryngol Clin North Am. 1984; 17:115–30.
Article29. Hoffman MR, Mielens JD, Ciucci MR, Jones CA, Jiang JJ, McCulloch TM. High-resolution manometry of pharyngeal swallow pressure events associated with effortful swallow and the Mendelsohn maneuver. Dysphagia. 2012; 27:418–26.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of the Chin-Tuck Maneuver on Anatomical Changes and Angles during Swallowing: A Systematic Review
- Viscosity Control: Effect on Pharyngeal Residue in Dysphagia Patients with Reduced Pharyngeal Constriction
- Effect of Chin Tuck Maneuver on Aspiration and Pharyngeal Residues Evaluated Using Simultaneous Videofluoroscopic Swallowing Study and Fiberoptic Endoscopic Evaluation of Swallowing
- The Effects of Viscosity on Oropharyngeal Phase
- A Case of Idiopathic Pharyngeal Dyskinesia WHO Complained of Dysphagia