The Impact of the Coronavirus Disease-2019 Pandemic on Childhood Obesity and Vitamin D Status
- Affiliations
-
- 1Department of Pediatrics, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2510741
- DOI: http://doi.org/10.3346/jkms.2021.36.e21
Abstract
- Background
The risk of weight gain as a consequence of school closure in children during the coronavirus disease-2019 (COVID-19) pandemic has been recognized. This study was performed to investigate changes in anthropometric and metabolic parameters in children following a 6-month period of social distancing and school closure due to the pandemic.
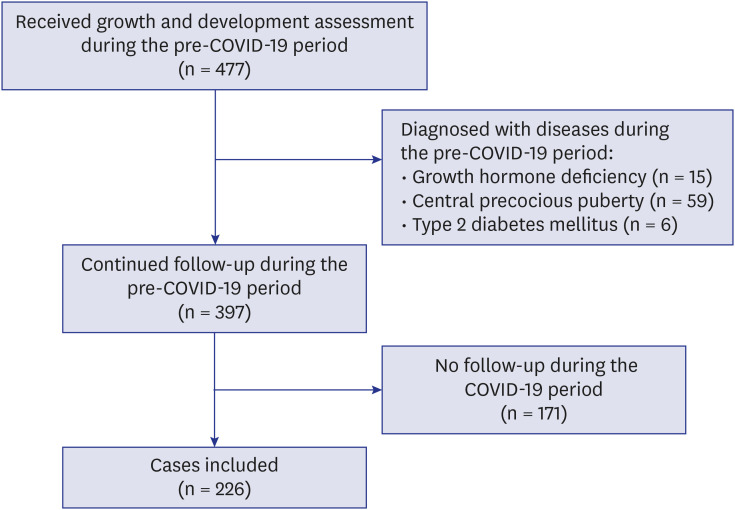
Methods
This retrospective cohort study was conducted in school-aged children that were on routine follow-up at the Growth Clinic of Seoul St. Mary's Hospital. Changes in body mass index (BMI) standard deviation scores (z-scores), lipid profiles, and vitamin D levels were investigated. The 1-year period prior to school closure was defined as “pre-COVID-19 period,” and the subsequent 6-month period as “COVID-19 period.”
Results
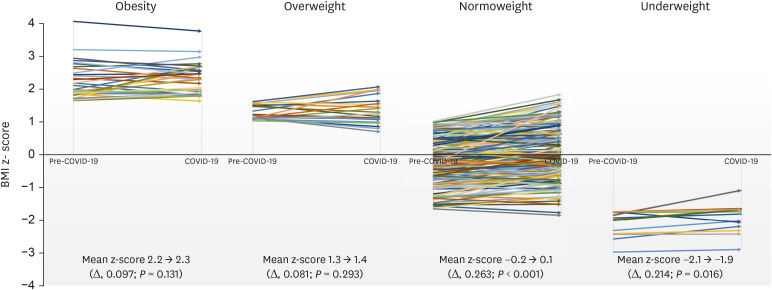
Overall, 226 children between 4 to 14 years old without comorbidities were assessed. On average, their BMI z-scores increased by 0.219 (95% confidence interval [CI], 0.167–0.271; P < 0.001) in the COVID-19 period compared to the pre-COVID-19 period, and the proportion of overweight or obesity increased from 23.9% in the pre-COVID-19 period to 31.4% in the COVID-19 period. The number of days after school closure ( P = 0.004) and being in the normoweight category in the pre-COVID-19 period ( P = 0.017) were factors associated with an increased BMI in the COVID-19 period. The mean triglyceride (105.8 mg/dL vs. 88.6 mg/dL, P < 0.001) and low-density lipoprotein-cholesterol (100.2 mg/dL vs. 94.0 mg/dL, P = 0.002) levels were higher, whereas the calcidiol level (18.9 mg/dL vs. 23.8 mg/dL, P < 0.001) was lower in the COVID-19 period compared to the pre-COVID-19 period.
Conclusion
Within 6 months, increased childhood obesity and vitamin D deficiencies were observed. The duration of school closure was significantly associated with an increased BMI and being normoweight does not exclude the risks for gaining weight.
Keyword
Figure
Cited by 5 articles
-
Parental Mental Health and Children's Behaviors and Media Usage during COVID-19-Related School Closures
Seong-Ju Kim, Sangha Lee, Hyojin Han, Jaeoh Jung, Su-Jin Yang, Yunmi Shin
J Korean Med Sci. 2021;36(25):e184. doi: 10.3346/jkms.2021.36.e184.Changes in the Incidence of Intussusception and Infectious Diseases After the COVID-19 Pandemic in Korea
In Hyuk Yoo, Hyun Mi Kang, Dae Chul Jeong
J Korean Med Sci. 2022;37(8):e60. doi: 10.3346/jkms.2022.37.e60.Lower-Income Predicts Increased Smartphone Use and Problematic Behaviors Among Schoolchildren During COVID-19 Related School Modification: A Longitudinal Study
Eun Sil Her, Sangha Lee, Su-Jin Yang, LiHae Park, Mi Gyeong Park, Seong-Ju Kim, Yunmi Shin
J Korean Med Sci. 2022;37(28):e225. doi: 10.3346/jkms.2022.37.e225.Correlation of tri-ponderal mass index with insulin-like growth factor-I and insulin-like growth factor binding protein-3 in children and adolescents
Iee Ho Choi, Sun-Young Kim, Minsun Kim
Ann Pediatr Endocrinol Metab. 2024;29(4):258-265. doi: 10.6065/apem.2346158.079.Effects of the COVID-19 pandemic on serum vitamin D concentration in Korean children
Jinjoo Choi, Yunsoo Choe, Kyeongmi Lee, Nayoung Kim, Seung Yang
Ann Pediatr Endocrinol Metab. 2024;29(4):220-226. doi: 10.6065/apem.2346196.098.
Reference
-
1. Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020; 91(1):157–160. PMID: 32191675.2. Korean Disease Control and Prevention Agency. The updates on COVID-19 in Korea as of 1 March. Updated March 1, 2020. Accessed October 3, 2020. https://www.cdc.go.kr/board/board.es?mid=a30402000000&bid=0030.3. An R. Projecting the impact of the coronavirus disease-2019 pandemic on childhood obesity in the United States: a microsimulation model. J Sport Health Sci. 2020; 9(4):302–312. PMID: 32454174.
Article4. Foster CE, Horwitz A, Thomas A, Opperman K, Gipson P, Burnside A, et al. Connectedness to family, school, peers, and community in socially vulnerable adolescents. Child Youth Serv Rev. 2017; 81:321–331. PMID: 30202142.
Article5. Wang YC, Vine S, Hsiao A, Rundle A, Goldsmith J. Weight-related behaviors when children are in school versus on summer breaks: does income matter? J Sch Health. 2015; 85(7):458–466. PMID: 26032276.
Article6. Rundle AG, Park Y, Herbstman JB, Kinsey EW, Wang YC. COVID-19-related school closings and risk of weight gain among children. Obesity (Silver Spring). 2020; 28(6):1008–1009. PMID: 32227671.
Article7. Kim JH, Yun S, Hwang SS, Shim JO, Chae HW, Lee YJ, et al. The 2017 Korean National Growth Charts for children and adolescents: development, improvement, and prospects. Korean J Pediatr. 2018; 61(5):135–149. PMID: 29853938.
Article8. Barlow SE; Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007; 120(Suppl 4):S164–92. PMID: 18055651.
Article9. Ministry of Education. Announcement of plans for pre-, elementary, middle and high school class attendance. Updated May 4, 2020. Accessed October 3, 2020. https://www.moe.go.kr/boardCnts/view.do?boardID=294&boardSeq=80510&lev=0&m=02.10. Korean Disease Control and Prevention Agency. The updates on COVID-19 in Korea as of August 18. Updated August 18, 2020. Accessed Oct 3, 2020. https://www.cdc.go.kr/board/board.es?mid=a20501000000&bid=0015.11. Korean Disease Control and Prevention Agency. Social distancing level 2 and fortified social distancing level 2 comparison. Updated September 8, 2020. Accessed October 3, 2020. http://ncov.mohw.go.kr/tcmBoardView.do?contSeq=359862.12. Centers for Disease Control and Prevention. The importance of reopening America's schools this fall. Updated July 23, 2020. Accessed October 3, 2020. https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/reopening-schools.html#fn37.13. Moreno JP, Vézina-Im LA, Vaughan EM, Baranowski T. Impact of child summertime obesity interventions on body mass index, and weight-related behaviours: a systematic review and meta-analysis protocol. BMJ Open. 2017; 7(10):e017144.
Article14. von Hippel PT, Powell B, Downey DB, Rowland NJ. The effect of school on overweight in childhood: gain in body mass index during the school year and during summer vacation. Am J Public Health. 2007; 97(4):696–702. PMID: 17329660.
Article15. Jeffreys M, Smith GD, Martin RM, Frankel S, Gunnell D. Childhood body mass index and later cancer risk: a 50-year follow-up of the Boyd Orr study. Int J Cancer. 2004; 112(2):348–351. PMID: 15352051.
Article16. Terry-McElrath YM, O’Malley PM, Johnston LD. Foods and beverages offered in US public secondary schools through the National School Lunch Program from 2011–2013: early evidence of improved nutrition and reduced disparities. Prev Med. 2015; 78:52–58. PMID: 26190369.
Article17. Ministry of Education. 2019 schoolyear free meal implementation status. Updated July 8, 2020. Accessed October 3, 2020. https://www.gov.kr/portal/gvrnReport/view/H2007000000681125?policyType=G00302&srchTxt=2020.18. Urbina EM, Khoury PR, McCoy CE, Dolan LM, Daniels SR, Kimball TR. Triglyceride to HDL-C ratio and increased arterial stiffness in children, adolescents, and young adults. Pediatrics. 2013; 131(4):e1082–90. PMID: 23460684.
Article19. Saggese G, Vierucci F, Prodam F, Cardinale F, Cetin I, Chiappini E, et al. Vitamin D in pediatric age: consensus of the Italian Pediatric Society and the Italian Society of Preventive and Social Pediatrics, jointly with the Italian Federation of Pediatricians. Ital J Pediatr. 2018; 44(1):51. PMID: 29739471.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The COVID-19 pandemic: an unprecedented tragedy in the battle against childhood obesity
- Obesity and Coronavirus Disease 2019
- What is the disease burden from childhood and adolescent obesity?: a narrative review
- Effects of the COVID-19 pandemic on serum vitamin D concentration in Korean children
- Management of Diabetes in Coronavirus Disease 2019: Prognosis and Practical Issues