Korean J Women Health Nurs.
2020 Dec;26(4):285-299. 10.4069/kjwhn.2020.11.19.
Factors associated with the decision to undergo risk-reducing salpingo-oophorectomy among women at high risk for hereditary breast and ovarian cancer: a systematic review
- Affiliations
-
- 1Graduate School, Yonsei University, Seoul, Korea
- 2National Evidence-based Healthcare Collaborating Agency, Seoul, Korea
- 3Mo-Im Kim Nursing Research Institute and College of Nursing, Yonsei University, Seoul, Korea
- KMID: 2510366
- DOI: http://doi.org/10.4069/kjwhn.2020.11.19
Abstract
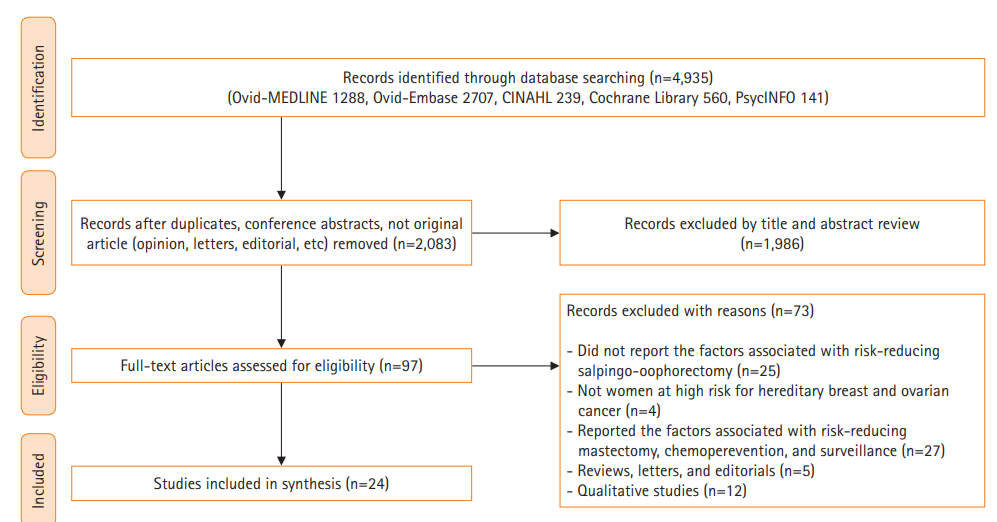
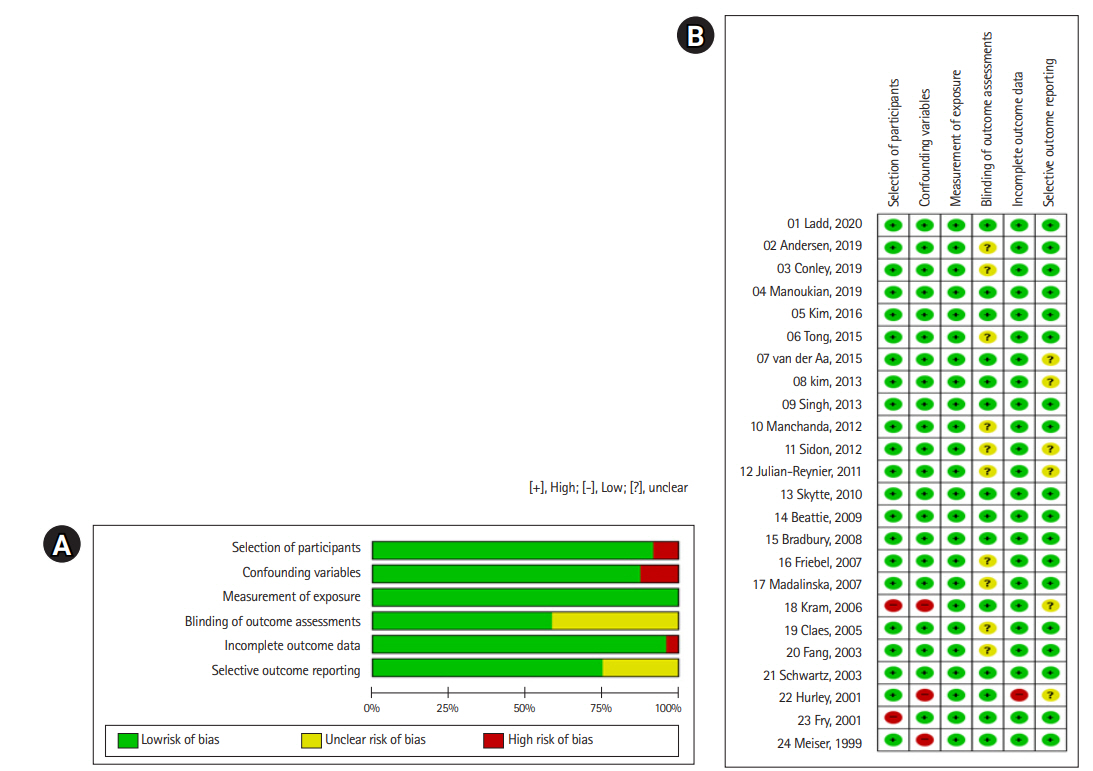
- This systematic review aims to identify factors associated with risk-reducing salpingo-oophorectomy (RRSO), including the uptake rate and decision timing, among women at high risk for hereditary breast and ovarian cancer (HBOC). We found 4,935 relevant studies using MEDLINE, Embase, CINAHL, and PsycINFO on July 6, 2020. Two authors screened the articles and extracted data. Twenty-four studies met the inclusion criteria. Quality assessment of articles was conducted using the Risk of Bias for Nonrandomized Studies tool. Five types of factors were identified (demographic factors, clinical factors, family history of cancer, psychological factors, and objective cancer risk). The specific significant factors were older age, having child(ren), being a BRCA1/2 carrier, mastectomy history, perceived risk for ovarian cancer, and perceived advantages of RRSO, whereas objective cancer risk was not significant. The uptake rate of RRSO was 23.4% to 87.2% (mean, 45.2%) among high-risk women for HBOC. The mean time to decide whether to undergo RRSO after BRCA testing was 4 to 34 months. RRSO decisions are affected by demographic, clinical, and psychological factors, rather than objective cancer risk. Nonetheless, women seeking RRSO should be offered information about objective cancer risk. Even though decision-making for RRSO is a complex and multifaceted process, the psychosocial factors that may influence decisions have not been comprehensively examined, including family attitudes toward RRSO, cultural norms, social values, and health care providers’ attitudes.
Figure
Cited by 1 articles
-
Attitudes toward Risk-Reducing Mastectomy and Risk-Reducing Salpingo-oophorectomy among Young, Unmarried, Healthy Women in Korea
Boyoung Park, Dongwon Kim, Jiyoung Kim, Bom Yi Lee, Junghyun Yoon, Sung-Won Kim
Cancer Res Treat. 2022;54(2):375-382. doi: 10.4143/crt.2021.449.
Reference
-
References
1. Hartmann LC, Lindor NM. The role of risk-reducing surgery in hereditary breast and ovarian cancer. N Engl J Med. 2016; 374(5):454–468. https://doi.org/10.1056/NEJMra1503523.
Article2. Petrucelli N, Daly MB, Feldman GL. Hereditary breast and ovarian cancer due to mutations in BRCA1 and BRCA2. Genet Med. 2010; 12(5):245–259. https://doi.org/10.1097/GIM.0b013e3181d38f2f.
Article3. Kang E, Seong MW, Park SK, Lee JW, Lee J, Kim LS, et al. The prevalence and spectrum of BRCA1 and BRCA2 mutations in Korean population: recent update of the Korean Hereditary Breast Cancer (KOHBRA) study. Breast Cancer Res Treat. 2015; 151(1):157–168. https://doi.org/10.1007/s10549-015-3377-4.
Article4. Rebbeck TR, Kauff ND, Domchek SM. Meta-analysis of risk reduction estimates associated with risk-reducing salpingo-oophorectomy in BRCA1 or BRCA2 mutation carriers. J Natl Cancer Inst. 2009; 101(2):80–87. https://doi.org/10.1093/jnci/djn442.
Article5. Padamsee TJ, Wills CE, Yee LD, Paskett ED. Decision making for breast cancer prevention among women at elevated risk. Breast Cancer Res. 2017; 19(1):34. https://doi.org/10.1186/s13058-017-0826-5.
Article6. Meadows R, Padamsee TJ, Paskett ED. Distinctive psychological and social experiences of women choosing prophylactic oophorectomy for cancer prevention. Health Care Women Int. 2018; 39(5):595–616. https://doi.org/10.1080/07399332.2018.1424855.
Article7. Howard AF, Balneaves LG, Bottorff JL. Women’s decision making about risk-reducing strategies in the context of hereditary breast and ovarian cancer: a systematic review. J Genet Couns. 2009; 18(6):578–597. https://doi.org/10.1007/s10897-009-9245-9.
Article8. Hickey M, Rio I, Trainer A, Marino JL, Wrede CD, Peate M. What information do healthcare professionals need to inform premenopausal women about risk-reducing salpingo-oophorectomy? Menopause. 2020; 27(1):20–25. https://doi.org/10.1097/GME.0000000000001421.
Article9. Cherry C, Ropka M, Lyle J, Napolitano L, Daly MB. Understanding the needs of women considering risk-reducing salpingo-oophorectomy. Cancer Nurs. 2013; 36(3):E33–E38. https://doi.org/10.1097/NCC.0b013e3182642cb5.
Article10. Rosenberg SM, Greaney ML, Patenaude AF, Sepucha KR, Meyer ME, Partridge AH. “I don’t want to take chances.”: a qualitative exploration of surgical decision making in young breast cancer survivors. Psychooncology. 2018; 27(6):1524–1529. https://doi.org/10.1002/pon.4683.
Article11. Bradbury AR, Ibe CN, Dignam JJ, Cummings SA, Verp M, White MA, et al. Uptake and timing of bilateral prophylactic salpingo-oophorectomy among BRCA1 and BRCA2 mutation carriers. Genet Med. 2008; 10(3):161–166. https://doi.org/10.1097/GIM.0b013e318163487d.
Article12. Kim D, Kang E, Hwang E, Sun Y, Hwang Y, Yom CK, et al. Factors affecting the decision to undergo risk-reducing salpingo-oophorectomy among women with BRCA gene mutation. Fam Cancer. 2013; 12(4):621–628. https://doi.org/10.1007/s10689-013-9625-z.
Article13. Singh K, Lester J, Karlan B, Bresee C, Geva T, Gordon O. Impact of family history on choosing risk-reducing surgery among BRCA mutation carriers. Am J Obstet Gynecol. 2013; 208(4):329. e1-329.e3296. https://doi.org/10.1016/j.ajog.2013.01.026.
Article14. Kim SI, Lim MC, Lee DO, Kong SY, Seo SS, Kang S, et al. Uptake of risk-reducing salpingo-oophorectomy among female BRCA mutation carriers: experience at the National Cancer Center of Korea. J Cancer Res Clin Oncol. 2016; 142(1):333–340. https://doi.org/10.1007/s00432-015-2051-x.
Article15. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009; 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097.
Article16. Kim SY, Park JE, Lee YJ, Seo HJ, Sheen SS, Hahn S, et al. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol. 2013; 66(4):408–414. https://doi.org/10.1016/j.jclinepi.2012.09.016.
Article17. Conley CC, Agnese DM, Vadaparampil ST, Andersen BL. Factors associated with intentions for breast cancer risk management: does risk group matter? Psychooncology. 2019; 28(5):1119–1126. https://doi.org/10.1002/pon.5066.
Article18. Manoukian S, Alfieri S, Bianchi E, Peissel B, Azzollini J, Borreani C. Risk-reducing surgery in BRCA1/BRCA2 mutation carriers: are there factors associated with the choice? Psychooncology. 2019; 28(9):1871–1878. https://doi.org/10.1002/pon.5166.
Article19. Andersen MR, Karlan BY, Drescher CW, Paley P, Hawley S, Palomares M, et al. False-positive screening events and worry influence decisions about surgery among high-risk women. Health Psychol. 2019; 38(1):43–52. https://doi.org/10.1037/hea0000647.
Article20. Ladd MK, Peshkin BN, Senter L, Baldinger S, Isaacs C, Segal H, et al. Predictors of risk-reducing surgery intentions following genetic counseling for hereditary breast and ovarian cancer. Transl Behav Med. 2020; 10(2):337–346. https://doi.org/10.1093/tbm/iby101.
Article21. Tong A, Kelly S, Nusbaum R, Graves K, Peshkin BN, Valdimarsdottir HB, et al. Intentions for risk-reducing surgery among high-risk women referred for BRCA1/BRCA2 genetic counseling. Psychooncology. 2015; 24(1):33–39. https://doi.org/10.1002/pon.3560.
Article22. van der Aa JE, Hoogendam JP, Butter ES, Ausems MG, Verheijen RH, Zweemer RP. The effect of personal medical history and family history of cancer on the uptake of risk-reducing salpingo-oophorectomy. Fam Cancer. 2015; 14(4):539–544. https://doi.org/10.1007/s10689-015-9827-7.
Article23. Manchanda R, Burnell M, Abdelraheim A, Johnson M, Sharma A, Benjamin E, et al. Factors influencing uptake and timing of risk reducing salpingo-oophorectomy in women at risk of familial ovarian cancer: a competing risk time to event analysis. BJOG. 2012; 119(5):527–536. https://doi.org/10.1111/j.1471-0528.2011.03257.x.
Article24. Sidon L, Ingham S, Clancy T, Clayton R, Clarke A, Jones EA, et al. Uptake of risk-reducing salpingo-oophorectomy in women carrying a BRCA1 or BRCA2 mutation: evidence for lower uptake in women affected by breast cancer and older women. Br J Cancer. 2012; 106(4):775–779. https://doi.org/10.1038/bjc.2011.573.
Article25. Julian-Reynier C, Mancini J, Mouret-Fourme E, Gauthier-Villars M, Bonadona V, Berthet P, et al. Cancer risk management strategies and perceptions of unaffected women 5 years after predictive genetic testing for BRCA1/2 mutations. Eur J Hum Genet. 2011; 19(5):500–506. https://doi.org/10.1038/ejhg.2010.241.
Article26. Skytte AB, Gerdes AM, Andersen MK, Sunde L, Brøndum-Nielsen K, Waldstrøm M, et al. Risk-reducing mastectomy and salpingo-oophorectomy in unaffected BRCA mutation carriers: uptake and timing. Clin Genet. 2010; 77(4):342–349. https://doi.org/10.1111/j.1399-0004.2009.01329.x.
Article27. Beattie MS, Crawford B, Lin F, Vittinghoff E, Ziegler J. Uptake, time course, and predictors of risk-reducing surgeries in BRCA carriers. Genet Test Mol Biomarkers. 2009; 13(1):51–56. https://doi.org/10.1089/gtmb.2008.0067.
Article28. Friebel TM, Domchek SM, Neuhausen SL, Wagner T, Evans DG, Isaacs C, et al. Bilateral prophylactic oophorectomy and bilateral prophylactic mastectomy in a prospective cohort of unaffected BRCA1 and BRCA2 mutation carriers. Clin Breast Cancer. 2007; 7(11):875–882. https://doi.org/10.3816/CBC.2007.n.053.
Article29. Madalinska JB, van Beurden M, Bleiker EM, Valdimarsdottir HB, Lubsen-Brandsma L, Massuger LF, et al. Predictors of prophylactic bilateral salpingo-oophorectomy compared with gynecologic screening use in BRCA1/2 mutation carriers. J Clin Oncol. 2007; 25(3):301–307. https://doi.org/10.1200/JCO.2006.07.4922.
Article30. Kram V, Peretz T, Sagi M. Acceptance of preventive surgeries by Israeli women who had undergone BRCA testing. Fam Cancer. 2006; 5(4):327–335. https://doi.org/10.1007/s10689-006-0002-z.
Article31. Claes E, Evers-Kiebooms G, Decruyenaere M, Denayer L, Boogaerts A, Philippe K, et al. Surveillance behavior and prophylactic surgery after predictive testing for hereditary breast/ovarian cancer. Behav Med. 2005; 31(3):93–105. https://doi.org/10.3200/BMED.31.3.93-106.
Article32. Schwartz MD, Kaufman E, Peshkin BN, Isaacs C, Hughes C, DeMarco T, et al. Bilateral prophylactic oophorectomy and ovarian cancer screening following BRCA1/BRCA2 mutation testing. J Clin Oncol. 2003; 21(21):4034–4041. https://doi.org/10.1200/JCO.2003.01.088.
Article33. Fang CY, Miller SM, Malick J, Babb J, Hurley KE, Engstrom PF, et al. Psychosocial correlates of intention to undergo prophylactic oophorectomy among women with a family history of ovarian cancer. Prev Med. 2003; 37(5):424–431. https://doi.org/10.1016/s0091-7435(03)00163-4.
Article34. Hurley KE, Miller SM, Costalas JW, Gillespie D, Daly MB. Anxiety/uncertainty reduction as a motivation for interest in prophylactic oophorectomy in women with a family history of ovarian cancer. J Womens Health Gend Based Med. 2001; 10(2):189–199. https://doi.org/10.1089/152460901300039566.
Article35. Fry A, Rush R, Busby-Earle C, Cull A. Deciding about prophylactic oophorectomy: what is important to women at increased risk of ovarian cancer? Prev Med. 2001; 33(6):578–585. https://doi.org/10.1006/pmed.2001.0924.
Article36. Meiser B, Butow P, Barratt A, Friedlander M, Gattas M, Kirk J, et al. Attitudes toward prophylactic oophorectomy and screening utilization in women at increased risk of developing hereditary breast/ovarian cancer. Gynecol Oncol. 1999; 75(1):122–129. https://doi.org/10.1006/gyno.1999.5544.
Article37. Glassey R, Ives A, Saunders C, Musiello T. Decision making, psychological wellbeing and psychosocial outcomes for high risk women who choose to undergo bilateral prophylactic mastectomy - a review of the literature. Breast. 2016; 28:130–135. https://doi.org/10.1016/j.breast.2016.05.012.
Article38. Ager B, Butow P, Jansen J, Phillips KA, Porter D; CPM DA Advisory Group. Contralateral prophylactic mastectomy (CPM): a systematic review of patient reported factors and psychological predictors influencing choice and satisfaction. Breast. 2016; 28:107–120. https://doi.org/10.1016/j.breast.2016.04.005.
Article39. Sun S, Li ST, Ngeow J. Factors shaping at-risk individuals’ decisions to undergo genetic testing for cancer in Asia. Health Soc Care Community. 2020; 28(5):1569–1577. https://doi.org/10.1111/hsc.12981.
Article40. Haroun I, Graham T, Poll A, Sun P, Hill K, Weitzner E, et al. Reasons for risk-reducing mastectomy versus MRI-screening in a cohort of women at high hereditary risk of breast cancer. Breast. 2011; 20(3):254–258. https://doi.org/10.1016/j.breast.2011.01.006.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Attitudes toward Risk-Reducing Mastectomy and Risk-Reducing Salpingo-oophorectomy among Young, Unmarried, Healthy Women in Korea
- Basic knowledge for counseling patients undergoing risk-reducing salpingo-oophorectomy
- The influence of BRCA variants of unknown significance on cancer risk management decision-making
- Single-Port Access Laparoscopic Prophylactic Bilateral Salpingo-Oophorectomy in BRCA-Positive Breast Cancer Patient: A Case Report
- Uptake Rate of Risk-Reducing Salpingo-Oophorectomy and Surgical Outcomes of Female Germline BRCA1/2 Mutation Carriers: A Retrospective Cohort Study