J Korean Med Sci.
2020 Dec;35(50):e417. 10.3346/jkms.2020.35.e417.
Systematic Preventable Trauma Death Rate Survey to Establish the Regionbased Inclusive Trauma System in a Representative Province of Korea
- Affiliations
-
- 1Division of Trauma Surgery, Department of Surgery, Ajou University School of Medicine, Suwon, Korea
- 2Southern Gyeonggi Trauma Center, Ajou University Hospital, Suwon, Korea
- 3National Emergency Medical Center, National Medical Center, Seoul, Korea
- 4The Health Insurance Review & Assessment Service, Wonju, Korea
- 5Department of Emergency Medicine, Uijeongbu St. Mary's Hospital, The Catholic University of Korea, Seoul, Korea
- KMID: 2509752
- DOI: http://doi.org/10.3346/jkms.2020.35.e417
Abstract
- Background
Trauma mortality review is the first step in assessing the quality of the trauma treatment system and provides an important basis for establishing a regional inclusive trauma system. This study aimed to obtain a reliable measure of the preventable trauma death rate in a single province in Korea.
Methods
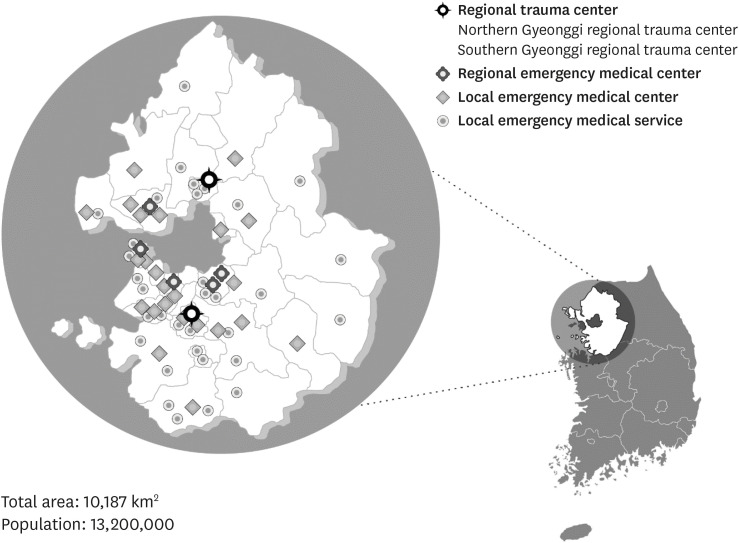
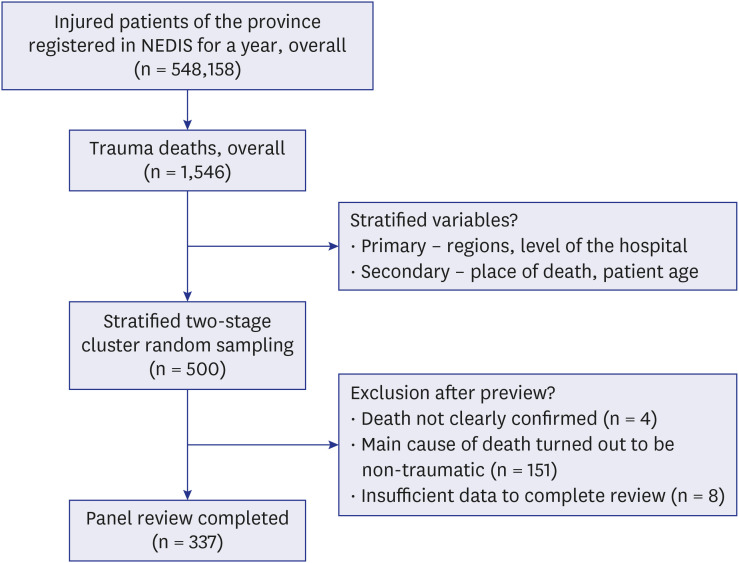
From January to December 2017, a total of 500 sample cases of trauma-related deaths from 64 hospitals in Gyeonggi Province were included. All cases were evaluated for preventability and opportunities for improvement using a multidisciplinary panel review approach.
Results
Overall, 337 cases were included in the calculation for the preventable trauma death rate. The preventable trauma death rate was estimated at 17.0%. The odds ratio was 3.97 folds higher for those who arrived within “1–3 hours” than those who arrived within “1 hour.” When the final treatment institution was not a regional trauma center, the odds ratio was 2.39 folds higher than that of a regional trauma center. The most significant stage of preventable trauma death was the hospital stage, during which 86.7% of the cases occurred, of which only 10.3% occurred in the regional trauma center, whereas preventable trauma death was more of a problem at emergency medical institutions.
Conclusion
The preventable trauma death rate was slightly lower in this study than in previous studies, although several problems were noted during inter-hospital transfer; in the hospital stage, more problems were noted at emergency medical care facilities than at regional trauma centers. Further, several opportunities for improvements were discovered regarding bleeding control.
Figure
Reference
-
1. World Health Organization. Guidelines for Trauma Quality Improvement Programmes. Geneva, Switzerland: WHO Press;2009.2. Mock C, Joshipura M, Arreola-Risa C, Quansah R. An estimate of the number of lives that could be saved through improvements in trauma care globally. World J Surg. 2012; 36(5):959–963. PMID: 22419411.
Article3. Cales RH, Trunkey DD. Preventable trauma deaths. A review of trauma care systems development. JAMA. 1985; 254(8):1059–1063. PMID: 3894708.
Article4. Jung K, Kim I, Park SK, Cho H, Park CY, Yun JH, et al. Preventable trauma death rate after establishing a national trauma system in Korea. J Korean Med Sci. 2019; 34(8):e65. PMID: 30833882.
Article5. Kim Y, Jung KY, Cho KH, Kim H, Ahn HC, Oh SH, et al. Preventable trauma deaths rates and management errors in emergency medical system in Korea. J Korean Soc Emerg Med. 2006; 17(5):385–394.6. Kim Y. Assessing Preventable Trauma Death Rate and Improving Trauma Center Administration. Seoul, Korea: Ministry of Health & Welfare; Research and Development Business Foundations in Seoul National University;2017.7. Korean Statistical Information Service. Annual population demographics. Updated 2019. Accessed March 1, 2020. http://kosis.kr/statisticsList/statisticsListIndex.do?menuId=M_01_01&vwcd=MT_ZTITLE&parmTabId=M_01_01.8. Jung KY, Kim JS, Kim Y. Problems in trauma care and preventable deaths. J Korean Soc Emerg Med. 2001; 12(1):45–56.9. Motomura T, Mashiko K, Matsumoto H, Motomura A, Iwase H, Oda S, et al. Preventable trauma deaths after traffic accidents in Chiba Prefecture, Japan, 2011: problems and solutions. J Nippon Med Sch. 2014; 81(5):320–327. PMID: 25391701.
Article10. Sanddal TL, Esposito TJ, Whitney JR, Hartford D, Taillac PP, Mann NC, et al. Analysis of preventable trauma deaths and opportunities for trauma care improvement in utah. J Trauma. 2011; 70(4):970–977. PMID: 21206286.
Article11. Teixeira PG, Inaba K, Hadjizacharia P, Brown C, Salim A, Rhee P, et al. Preventable or potentially preventable mortality at a mature trauma center. J Trauma. 2007; 63(6):1338–1346. PMID: 18212658.
Article12. Nirula R, Maier R, Moore E, Sperry J, Gentilello L. Scoop and run to the trauma center or stay and play at the local hospital: hospital transfer's effect on mortality. J Trauma. 2010; 69(3):595–599. PMID: 20838131.
Article13. Rotondo MF, Cribari C, Smith RS. American College of Surgeons Committee on Trauma. Resources for Optimal Care of the Injured Patient. 6th ed. Chicago, IL: American College of Surgeons;2014.14. O'Reilly D, Mahendran K, West A, Shirley P, Walsh M, Tai N. Opportunities for improvement in the management of patients who die from haemorrhage after trauma. Br J Surg. 2013; 100(6):749–755. PMID: 23483534.15. Pfeifer R, Tarkin IS, Rocos B, Pape HC. Patterns of mortality and causes of death in polytrauma patients--has anything changed? Injury. 2009; 40(9):907–911. PMID: 19540488.
Article16. Davenport RA, Tai N, West A, Bouamra O, Aylwin C, Woodford M, et al. A major trauma centre is a specialty hospital not a hospital of specialties. Br J Surg. 2010; 97(1):109–117. PMID: 20013932.
Article17. Celso B, Tepas J, Langland-Orban B, Pracht E, Papa L, Lottenberg L, et al. A systematic review and meta-analysis comparing outcome of severely injured patients treated in trauma centers following the establishment of trauma systems. J Trauma. 2006; 60(2):371–378. PMID: 16508498.
Article18. Liberman M, Mulder DS, Jurkovich GJ, Sampalis JS. The association between trauma system and trauma center components and outcome in a mature regionalized trauma system. Surgery. 2005; 137(6):647–658. PMID: 15933633.
Article19. Chardbunchachai W, Suppachutikul A, Santikarn C. Development of Service System for Injury Patients by Utilizing Data from the Trauma Registry. Khon Kaen, Thailand: Trauma and Critical Care Center, Khon Kaen Regional Hospital;2002.20. Hwang K, Kwon J, Cho J, Heo Y, Lee JC, Jung K. Implementation of trauma center and massive transfusion protocol improves outcomes for major trauma patients: a study at a single institution in Korea. World J Surg. 2018; 42(7):2067–2075. PMID: 29290073.
Article21. Malone DL, Hess JR, Fingerhut A. Massive transfusion practices around the globe and a suggestion for a common massive transfusion protocol. J Trauma. 2006; 60(6):Suppl. S91–S96. PMID: 16763487.
Article22. Oriol MD. Crew resource management: applications in healthcare organizations. J Nurs Adm. 2006; 36(9):402–406. PMID: 16969251.23. Brohi K, Eaglestone S. Traumatic Coagulopathy and Massive Transfusion: Improving Outcomes and Saving Blood. Southampton, UK: NIHR Journals Library;2017.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Understanding Regional Trauma Centers and managing a trauma care system in South Korea: a systematic review
- Background and progress of regional trauma center development
- Outcomes of the support services for the establishment of regional level 1 trauma centers
- Major Causes of Preventable Death in Trauma Patients
- Survey of Recognition of Trauma and Trauma Care System