J Korean Med Sci.
2020 Apr;35(14):e98. 10.3346/jkms.2020.35.e98.
Analysis of Associated Anomalies in Anorectal Malformation: Major and Minor Anomalies
- Affiliations
-
- 1Division of Pediatric Surgery, Department of Surgery, Korea University College of Medicine,Seoul,Korea.
- 2Department of Pediatric Surgery, Seoul National University Children's Hospital, Seoul National University College of Medicine,Seoul,Korea.
- KMID: 2509616
- DOI: http://doi.org/10.3346/jkms.2020.35.e98
Abstract
- Background
Fifty to sixty percent of patients with anorectal malformation (ARM) have at least one associated anomaly (AA). We determined the incidence of AA with the subtypes of ARM classified in accordance with the Krickenbeck classification and analyzed differences in the incidence rates of major and minor AAs according to organ system.
Methods
From January 1999 to May 2017, we retrospectively analyzed congenital anomalies in patients who underwent an anoplasty for ARM at our institution. The AAs were divided into nine organ systems. To analyze the difference in the incidence of AAs, we calculated odds ratios (ORs) using cases of perineal fistula as the base group.
Results
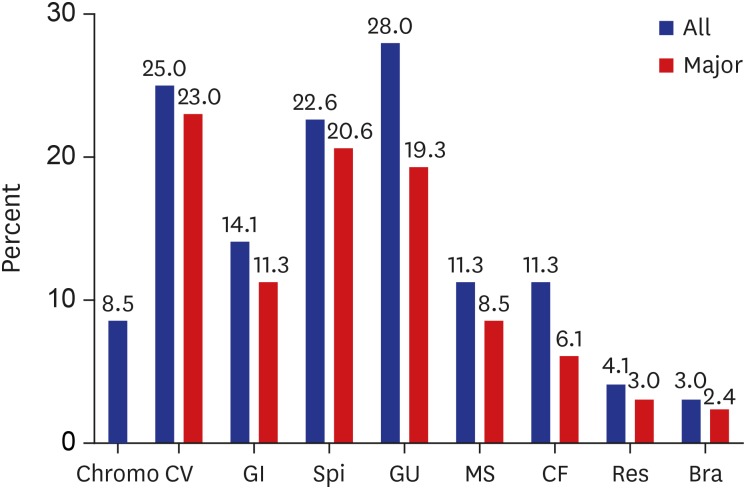
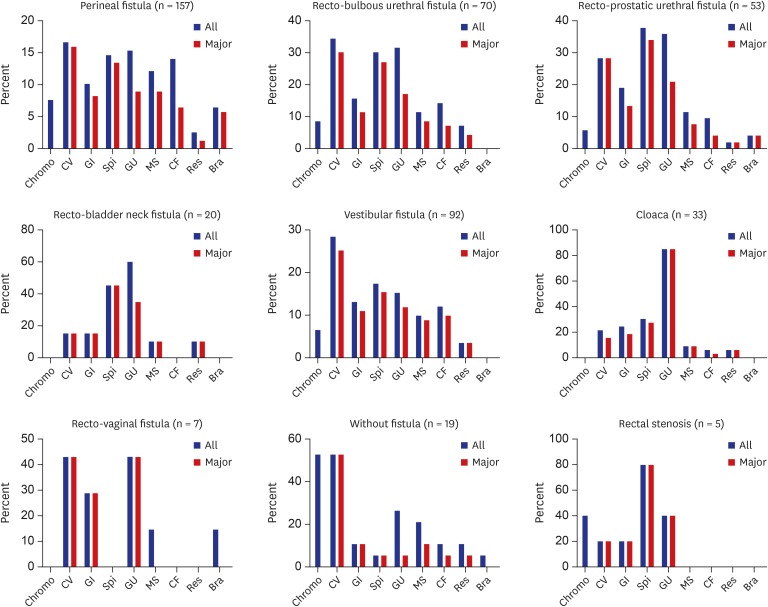
Of the 460 patients, 256 (55.7%) were male, 299 (65%) had at least one anomaly, and 274 (59.6%) had major AAs. According to organ system, AAs were most common in the genitourinary (28%), cardiovascular (25%), and spinal/vertebral systems (22.6%). Major AA was most common in the cardiovascular (23%) and spinal/vertebral and genitourinary systems (19.3%). According to ARM subtype, AAs were common in the order of cloaca (93.9%), rectovaginal fistula (85.7%), and recto-bladder neck fistula (85%). For the incidence of AAs, cloaca (OR, 15.7) and recto-bladder neck fistula (OR, 5.74) showed significantly higher ORs. In the analysis of major AAs, the cloaca (OR, 19.77) showed the highest OR, followed by no fistula (OR, 4.78) and recto-bladder neck fistula (OR, 3.83).
Conclusion
A considerable number of patients with ARM had AAs. Our data are useful for predicting AAs in patients with ARM.
Keyword
Figure
Reference
-
1. Santulli TV. The treatment of imperforate anus and associated fistulas. Surg Gynecol Obstet. 1952; 95(5):601–614. PMID: 12995253.2. Trusler GA, Wilkinson RH. Imperforate anus: a review of 147 cases. Can J Surg. 1962; 5:269–277. PMID: 13922716.3. Smith ED, Saeki M. Associated anomalies. Birth Defects Orig Artic Ser. 1988; 24(4):501–549. PMID: 3067774.4. Endo M, Hayashi A, Ishihara M, Maie M, Nagasaki A, Nishi T, et al. Analysis of 1,992 patients with anorectal malformations over the past two decades in Japan. Steering Committee of Japanese Study Group of Anorectal Anomalies. J Pediatr Surg. 1999; 34(3):435–441. PMID: 10211649.5. Stoll C, Alembik Y, Dott B, Roth MP. Associated malformations in patients with anorectal anomalies. Eur J Med Genet. 2007; 50(4):281–290. PMID: 17572165.
Article6. Nah SA, Ong CC, Lakshmi NK, Yap TL, Jacobsen AS, Low Y. Anomalies associated with anorectal malformations according to the Krickenbeck anatomic classification. J Pediatr Surg. 2012; 47(12):2273–2278. PMID: 23217888.
Article7. Bălănescu RN, Topor L, Moga A. Anomalies associated with anorectal malformations. Chirurgia (Bucur). 2013; 108(1):38–42. PMID: 23464767.8. Ratan SK, Rattan KN, Pandey RM, Mittal A, Magu S, Sodhi PK. Associated congenital anomalies in patients with anorectal malformations--a need for developing a uniform practical approach. J Pediatr Surg. 2004; 39(11):1706–1711. PMID: 15547838.
Article9. Holschneider A, Hutson J, Peña A, Beket E, Chatterjee S, Coran A, et al. Preliminary report on the International Conference for the Development of Standards for the Treatment of Anorectal Malformations. J Pediatr Surg. 2005; 40(10):1521–1526. PMID: 16226976.
Article10. European Surveillance of Congenital Anomalies. EUROCAT guide 1.4 and reference documents. Updated 2018. Accessed December 26, 2018. http://www.eurocat-network.eu/content/EUROCAT-Guide-1.4-Full-Guide.pdf.11. WHO/CDC/ICBDSR. Birth Defects Surveillance: a Manual for Programme Managers. Geneva: World Health Organization;2014.12. Quan L, Smith DW. The VATER association. Vertebral defects, anal atresia, T-E fistula with esophageal atresia, radial and renal dysplasia: a spectrum of associated defects. J Pediatr. 1973; 82(1):104–107. PMID: 4681850.13. Temtamy SA, Miller JD. Extending the scope of the VATER association: definition of the VATER syndrome. J Pediatr. 1974; 85(3):345–349. PMID: 4372554.
Article14. Cuschieri A. EUROCAT Working Group. Anorectal anomalies associated with or as part of other anomalies. Am J Med Genet. 2002; 110(2):122–130. PMID: 12116249.
Article15. Totonelli G, Catania VD, Morini F, Fusaro F, Mosiello G, Iacobelli BD, et al. VACTERL association in anorectal malformation: effect on the outcome. Pediatr Surg Int. 2015; 31(9):805–808. PMID: 26143411.
Article16. Levitt MA, Patel M, Rodriguez G, Gaylin DS, Pena A. The tethered spinal cord in patients with anorectal malformations. J Pediatr Surg. 1997; 32(3):462–468. PMID: 9094019.
Article17. Fanjul M, Samuk I, Bagolan P, Leva E, Sloots C, Giné C, et al. Tethered cord in patients affected by anorectal malformations: a survey from the ARM-Net Consortium. Pediatr Surg Int. 2017; 33(8):849–854. PMID: 28674920.
Article18. Heij HA, Nievelstein RA, de Zwart I, Verbeeten BW, Valk J, Vos A. Abnormal anatomy of the lumbosacral region imaged by magnetic resonance in children with anorectal malformations. Arch Dis Child. 1996; 74(5):441–444. PMID: 8669962.
Article19. Golonka NR, Haga LJ, Keating RP, Eichelberger MR, Gilbert JC, Hartman GE, et al. Routine MRI evaluation of low imperforate anus reveals unexpected high incidence of tethered spinal cord. J Pediatr Surg. 2002; 37(7):966–969. PMID: 12077750.
Article20. Uchida K, Inoue M, Matsubara T, Otake K, Koike Y, Okugawa Y, et al. Evaluation and treatment for spinal cord tethering in patients with anorectal malformations. Eur J Pediatr Surg. 2007; 17(6):408–411. PMID: 18072026.
Article21. Totonelli G, Morini F, Catania VD, Schingo PM, Mosiello G, Palma P, et al. Anorectal malformations associated spinal cord anomalies. Pediatr Surg Int. 2016; 32(8):729–735. PMID: 27372296.
Article22. Parrott TS. Urologic implications of anorectal malformations. Urol Clin North Am. 1985; 12(1):13–21. PMID: 3883618.
Article23. Santulli TV, Schullinger JN, Kiesewetter WB, Bill AH Jr. Imperforate anus: a survey from the members of the Surgical Secton of the American Academy of Pediatrics. J Pediatr Surg. 1971; 6(4):484–487. PMID: 5563891.24. Rich MA, Brock WA, Peña A. Spectrum of genitourinary malformations in patients with imperforate anus. Pediatr Surg Int. 1988; 3(2-3):110–113.
Article25. Parrott TS, Woodard JR. Importance of cystourethrography in neonates with imperforate anus. Urology. 1979; 13(6):607–609. PMID: 377750.
Article26. Shaul DB, Harrison EA. Classification of anorectal malformations--initial approach, diagnostic tests, and colostomy. Semin Pediatr Surg. 1997; 6(4):187–195. PMID: 9368270.27. Misra D, Mushtaq I, Drake DP, Kiely EM, Spitz L. Associated urologic anomalies in low imperforate anus are capable of causing significant morbidity: a 15-year experience. Urology. 1996; 48(2):281–283. PMID: 8753741.
Article28. Hoekstra WJ, Scholtmeijer RJ, Molenaar JC, Schreeve RH, Schroeder FH. Urogenital tract abnormalities associated with congenital anorectal anomalies. J Urol. 1983; 130(5):962–963. PMID: 6632109.
Article29. Rickwood AM, Spitz L. Primary vesicoureteric reflux in neonates with imperforate anus. Arch Dis Child. 1980; 55(2):149–150. PMID: 7377836.
Article30. Narasimharao KL, Prasad GR, Mukhopadhyay B, Katariya S, Mitra SK, Pathak IC. Vesicoureteric reflux in neonates with anorectal anomalies. Br J Urol. 1983; 55(3):268–270. PMID: 6850240.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- MR Findings of Congenital Anorectal Malformation
- A Case of Amniotic Band Syndrome with limb anomalies
- The currarino triad of anorectal, sacral, and presacral anomalies
- Anorectal Malformations: Diagnosis and Management in Neonatal Period
- Anorectal Malformations Associated with Esophageal Atresia in Neonates